Transcription
Guide for Young Patients
FOREWORDThis booklet explains what toexpect when your child comes intothe Ulster Independent Clinic foran operation or investigation undergeneral anaesthetic.The contents have been adaptedfrom the leaflet – ‘Your Child’sGeneral Anaesthetic – Informationfor Parents and Guardians ofChildren’, produced by the RoyalCollege of Anaesthetists, TheAssociation of Anaesthetists ofGreat Britain and Ireland, andThe Association of PaediatricAnaesthetists of Great Britain andIreland, Fourth Edition 2014.Guide for Young Patients
CONTENTSWelcome. 04Preparing your child for hospital. 06Fasting. 09On the day of admission.10Parents’ guide to anaesthesia.12Consent.14Going to theatre.16After surgery.18Pain relief.19Going home. 20Side-effects and complications.21Checklist. 22Key information. 22Useful organisations. 23Getting here. 24CHKS accreditation. 26Fair Processing Notice.27Additional information.313
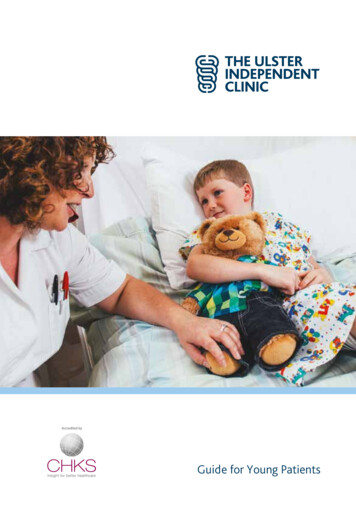
WELCOMEOn behalf of the staff, I’d like to welcomeyou to the Ulster Independent Clinic.We understand that the prospectof your child going into hospitalcan be worrying – for you as wellas your child. Rest assured,we’ll make every effort tolessen any anxieties by creatinga calming atmosphere for yourchild and ensuring they’re caredfor at all times by skilled andprofessional staff.This booklet sets out thebasic things you should knowabout preparing your child foradmission, about the treatmentthey will receive, and also aboutthe Clinic itself and its facilities.Guide for Young PatientsIf you have any questions or ifyou would like further details,please don’t hesitate to ask anymember of our team. We’ll behappy to help.Diane GrahamMatron / Chief Executive
5
PREPARING YOURCHILD FOR HOSPITALThere are several things that you can do to prepareyour child for coming into hospital. Unless your child isvery young, you should try and explain:– that they are goinginto hospital– that they will be having anoperation or investigationGuide for Young Patients– some basic informationabout what will happento them when they arein hospital.
Your child can help pack theirown bag and decide whichnightclothes and toys to bring.Each room has a TV with accessto children’s channels.When you are explaining things,try to use simple language thatthey can understand.– Explain that the operation orinvestigation will help yourchild get better.– Encourage your child to talkabout the operation and askquestions. Books, games,role-play and stories can helpwith this.– Talk about timing – when yourchild will have the operationor investigation and how longthey will stay in hospital.– If your child is going to bestaying in hospital overnight,let them know that you willbe able to stay with them inthe same room in a parent bednext to theirs.If you like, we can makearrangements for you andyour child to visit the wardand operating theatre beforeadmission day itself. To make anappointment, please call028 9068 7666 on Monday toFriday between 9am and 5pm.Do let us know in advance of anyspecial requirements your childhas and we will do whatever wecan to help.ImportantPlease let us know as soonas possible before the day ofthe procedure if your childhas been ill – developeda severe cough or cold,vomiting or diarrhoea,or had contact with anyinfectious diseases, forexample chickenpox. In thesecircumstances it may be bestto delay the operation untilthey are better.7
When should I tell my child?Use your child’s age as a rule ofthumb to judge when best to tellthem about going into hospital.That is:Aged 2–3Children between two and threeyears of age should be told twoto three days before and again onthe day of admission.Guide for Young PatientsAged 4–7Children between four and sevenyears of age should be told fourto seven days before the day ofadmission – and reminded againthe day before.Aged 7 Older children will usually beinvolved in making decisionsabout the operation orinvestigation, and discussion cantake place a few weeks before theday of admission.
FASTINGNothing to eat and drink: ‘Nil by Mouth’When we send you the letterabout your child’s admission,you’ll find instructions aboutwhen to stop your child eatingand drinking. Please note that thisincludes chewing gum as well.It is important for you and yourchild to follow these instructions.This is because, if there is foodor liquid in your child’s stomachduring anaesthetic, it could comeup into the back of the throat anddamage his or her lungs.These are the latest times atwhich you should give your childanything to eat or drink:6 hours before: Your child canhave a light meal, a glass of milkor a fizzy drink. Bottle-fed babiescan have formula feed.4 hours before: Babies canhave breast milk.2 hours: Children and babiescan have a drink of water ordiluted cordial – but not a fizzydrink or milk.9
ON THE DAY OF ADMISSIONA pre-operative visitThe anaesthetist will visit you onthe ward before the procedure todiscuss your child’s anaesthetic.This is a good point to ask anyquestions you may have aboutthis hospital visit, for example:The anaesthetist needs to findout about your child’s generalhealth, previous experiences ofanaesthesia, any medicines yourchild is taking and any allergies heor she might have.– What type of anaesthetic doyou recommend?– What are the risks of this typeof anaesthetic?– Does my child have anyspecial risks?– How will my child feelafterwards?Guide for Young Patients
Delays in the procedureOccasionally the anaesthetist maylearn something about your childthat means it would be safer notto do the procedure on that day.This could happen if your child hasa bad cold, has a rash or has eatenfood too recently. In this case,we will discuss rescheduling theprocedure with you.PremedicationPremedication (sometimes knownas a pre-med) is the name fordrugs sometimes given before ananaesthetic. Although they areused less often today, a pre-medmay help your child to relax, or itmay be recommended in relationto the kind of surgery your childwill be having.If your child does need apre-med, this will usually begiven as a liquid, some timebefore the anaesthetic.A pre-med may make your childdrowsier afterwards. If youplan to take them home on thesame day, this will influence thedischarge time.The drugs used can be:– sedatives to ease yourchild’s anxiety– pain-relieving drugs such asparacetamol that can help atthe end of the procedure– medications to protect yourchild from side-effects of theanaesthetic, such as nausea– an extra dose of treatment forillnesses like asthma.About an hour before theoperation is scheduled, a localanaesthetic “Magic Cream’’ canbe put on the hand or arm so thatinjections do not hurt. This creamis held in place with a special clearplaster. It works well for 9 out of10 children. This cream is calledEMLA or Ametop.11
PARENTS’ GUIDE TO ANAESTHESIAWhat is anaesthesia?The word anaesthesia means‘loss of sensation’:– a general anaesthetic ensuresthat your child is unconsciousand free of pain during anoperation or procedure– general anaesthesia is a stateof controlled unconsciousnessand freedom from painGuide for Young Patients– anaesthetics are the drugsthat are used to start andmaintain anaesthesia– anaesthetists are specialistdoctors who give theanaesthetic and look after thehealth of your child duringsurgery, and are also closelyinvolved with your child’s painrelief after surgery.
Anaesthetics, choice & your childIt’s often possible for you andyour child to choose how theanaesthetic and other medicinesare given. Sometimes there aremedical reasons why things haveto be done a certain way. If so,this will be explained to you.However, nothing will happenunless you understand and agreewith what has been planned. Yourwishes and those of your child arevery important.13
CONSENTBefore going to theatre, the ConsultantSurgeon will visit you both on the wardto discuss the surgery and answer anyquestions you or your child might have.The Consultant will ask you to givewritten consent to the surgery(if your child is under the age ofsixteen). Please ensure you havebeen given adequate informationto enable you and your child tomake an informed choice.Adolescents are encouragedto be actively involved in theprocess of consent and, if deemedcompetent by their Consultant,may sign their own consent formif under 16. However, generallythe parent or main carer of a childunder 16 signs the form, or ispresent to give verbal consent.Note: not all parents haveparental responsibility.It is recommended that childrenshould be accompanied during allmedical consultations.Information regarding consentmay be found online atwww.doh.uk/consentGuide for Young Patients
Who can provide consent?1. the child’s mother2. the child’s father:– where he has married thechild’s mother– where he is not married,but has obtained anauthorisation from thecourt or through a parentalresponsibility agreement– where he is registered as thefather on the child’s birthcertificate for children born onor after 15th April 20023. a person who has acquiredparental responsibility througha court order, residence orderor guardianship order forexample, foster parents,step-parents or grandparents4. the young person who is 16years or over5. a young person under 16years where the Consultantbelieves they are capable ofunderstanding the issuesand consequences6. the child’s legallyadoptive parents.Who cannot consent?A partner who is not married tothe child’s mother/father and doesnot have a court authorisationconfirming his/her parental rightscannot give consent.15
GOING TO THEATREIn the Anaesthetic RoomThe anaesthetic room is the room next tothe operating theatre where anaesthetics areusually administered.A nurse from the ward willaccompany you both to theanaesthetic room. Your child maytravel either in their bed, walk orbe carried by a parent.Your child will be able to take atoy or comforter with them, andthey will be able to wear theirown pyjamas to the operatingtheatre. (Or, if preferred, wewill provide a colourful gown.)Your child will be able to keepunderwear on.You will normally be welcome tostay with your child until they areanaesthetised. It may be possibleto give the anaesthetic while yourchild is sitting on your lap.The anaesthetist will use eithergas or an injection through acannula to start the anaesthetic.This will have been agreed withyou beforehand.Guide for Young PatientsMost older children will have aninjection through a cannula.If both methods are safe for yourchild, you may be able to choosewhich is used.If a cannula is used, your child willnormally become unconsciousvery quickly indeed. Theanaesthetist will then use a maskto continue the anaesthetic.If the anaesthetic is started withgas, the anaesthetist generallyuses a mask to give the gas,or may pass the gas through acupped hand gently placed overyour child’s nose and mouth.Anaesthetic gases smell similar tofelt-tip pens. It normally takes alittle while (one or two minutes)for the anaesthetic to take effect.It is normal for the child tobecome restless during this time.
What is a cannula?What happens next?A cannula is a thin plastic tubethat is placed into a vein underthe skin, usually on the back ofthe hand. A needle is used to putthe cannula in, but the needle isremoved immediately, leavingonly the soft cannula in place.Your child will be taken intothe operating theatre for theoperation or investigation. Youwill not be able to accompanyyour child further at this stage.A cannula can be left in place forhours or days so that drugs andfluids can be given without needfor further injections. Sometimesblood samples can also be takenthe same way.The anaesthetist will stay withyour child, monitoring their bloodpressure, pulse and breathingthroughout the procedure andensuring that they are safe andremain fully sedated.The cannula is removed beforeyour child is discharged.17
AFTER SURGERYRecovery roomMost children spend a period oftime in the recovery room. This isa place near the operating theatrewhere patients go immediatelyafter surgery until the effects ofthe anaesthetic drugs wear off. Thenursing staff in the recovery roomwill telephone you to let you knowyour child’s surgery has finished.Each child is cared for by aspecialist nurse until they haveregained consciousness and arecomfortable enough to return totheir room.Many children, especially youngerchildren, show signs of confusionor distress when they wake upin the recovery room. A fewchildren become very agitated.This may last around 30 minutes.Guide for Young PatientsIt’s naturally worrying for parentsand carers if a child wakes indistress. However, the recoveryroom nurses are very experiencedin this situation, and will adviseyou on how best to comfort andreassure your child.If your child is distressed, it mayalso be possible for you to be withthem in the recovery room duringthis time.The wardWhen your child returns to theroom, they may still be quitedrowsy. This is normal, andnursing staff will maintain closeobservation. Your child may drinkon return to the room and willbe given an ice-lolly and/or foodwhen more awake.
PAIN RELIEFPain-relieving drugs (analgesics)are given during anaesthesiato ensure that your child is ascomfortable as possible. Thetype of pain relief will depend onthe procedure. The anaesthetist,Surgeon and nurses will talk toyou about the best type of painrelief for your child.How pain relief is administered– Syrups and tablets:just like at home.– Suppositories:some pain-relieving medicineslike paracetamol can be givenrectally (into the bottom).These are often given whileyour child is anaesthetisedand last for several hours.Suppositories are very helpfulwhen children cannot takemedicines by mouth or arefeeling sick.– Local anaesthetics:these are injected near thenerves around the operationsite to numb the area. Theinjections are given whileyour child is anaesthetisedand the pain relief lasts forseveral hours.– Strong pain-relieving drugssuch as morphine can be givenin many different ways.19
GOING HOMEMany children have their investigations oroperations carried out as ‘day patients’ and gohome on the same day, while others may stayfor one or two nights post-operatively.After surgery, your childmay experience some pain ordiscomfort. You will be givenpain-relieving medications totake home with you, and we willexplain how these should betaken. You will also be given anadvice sheet and any dressingsthat may be required.Your child may not sleep wellafter a stay in hospital. Theirbehaviour might be a little moreclingy or difficult than before.This is a normal reaction, andthey will usually return to normalwithin three to four weeks.Occasionally children may feelsick after they have left hospital,or even vomit. This sometimeshappens in the car on the wayhome, so two adults are requiredto accompany the child.If you have any concernsabout your child when you gethome, contact the Clinic onthe number provided on thedischarge information leaflet.Guide for Young Patients
SIDE-EFFECTS AND COMPLICATIONSIn modern anaesthesia, seriousproblems are uncommon. Riskcannot be removed completely,but today’s equipment, trainingand drugs have made it a muchsafer procedure in recent years.Most children recover quickly andare soon back to normal. Somemay experience side-effects likesickness or a sore throat. Theseusually last only a short time andthere are medicines available totreat them if necessary.The exact likelihood ofcomplications depends on yourchild’s medical condition and onthe nature of the surgery andanaesthesia your child needs.The anaesthetist can discussthis with you in detail at thepre-operative visit.For a child in good health havingminor surgery:– 1 child in 5 becomes agitatedon waking– 1 child in 10 experiencesa headache, sore throat,sickness or dizziness– around 1 child in 10,000develops a serious allergicreaction to anaesthetic.To put this into context,throughout the whole of their life,an individual is at least 100 timesmore likely to suffer serious injuryor death in a road traffic accidentthan as a result of anaesthesia.21
CHECKLISTPrepare your child as instructed in this bookletMake sure your child fasts from the time statedBring pyjamas / t-shirts and pants, dressing gown, slippersFavourite toy or blanket, favourite mug / cup or bottleAny medications and inhalersNote of any drug or food allergiesKEY INFORMATION: AT A GLANCE– A child under the age of 12coming into the Clinic mustbe accompanied by one parentat all times throughout theirstay. This includes overnight.– If you have medical insurance,the company will cover thecost of this, in most cases.– If one parent of an adolescentwishes to stay with themovernight, arrangementscan be made for this at anadditional cost.– The parent who remainswith their child will receive asnack, light meal or full meal/ meals depending on theirlength of stay.Guide for Young Patients– There are tea and coffeefacilities on each ward foryour use.– If your child is stayingovernight, a fold-away parentbed will be placed in theirroom for you.– You will have full use of thefacilities in the room – en-suitefacilities with towels supplied,telephone and television.– All other visiting children mustbe supervised at all times.– Two adults are required toaccompany the child home inthe car.
USEFUL ORGANISATIONSRoyal College of AnaesthetistsAction for Sick ChildrenThe organisation is responsiblefor the standards in anaesthesia,critical care and pain managementthroughout the UK.www.rcoa.ac.ukThis is a children’s healthcarecharity, specially formed toensure that sick children alwaysreceive the highest standardof care. They have a series ofinformation leaflets specificallyto help parents cope with, andprepare for, different aspects ofchildren’s n of Anaesthetistsof Great Britain & IrelandThis organisation works topromote the development ofanaesthesia and the welfare ofanaesthetists and their patients inGreat Britain and Ireland.www.aagbi.orgFurther information, includingadditional information leafletsfor children to download, can befound on the websitewww.rcoa.ac.uk/patientinfo23
GETTING HEREThe Ulster Independent Clinic is situatedin South Belfast at the corner of StranmillisRoad and Malone Road.By car from M1 MotorwayPrepare for turning right on toStranmillis Road at the lights.From M1 take exit at Junction 2 forA55 Outer Ring.The Ulster Independent Clinic isclearly signposted on the left.Continue through two sets oftraffic lights, under railway bridgeand through a third set of lights toBalmoral Avenue.Continue along Balmoral Avenue tojunction with Malone Road.Take the slip road on the left on toMalone Road.By car from Belfast city centreFrom Queen’s University, keep in theleft-hand lane.Continue uphill to Stranmillis andpast Ulster Museum.Continue through Stranmillis Village.Prepare for turning right on toStranmillis Road at the lights.At roundabout, take 3rd exitsignposted for M1.The Ulster Independent Clinic isclearly signposted on the left.Continue along Stranmillis Road.By car from M2 MotorwayThe Ulster Independent Clinic is thelast entrance on the right, just beforethe traffic lights.Follow signposts for the Westlink/M1from the M2.By busTake the exit at Junction 2 for A55Outer Ring.The nearest bus stop is a 5–10 minutewalk from the Clinic. From DonegallSquare East in the city centre, take:Number 8A Stranmillis or Numbers8B or 8C for Malone.Continue through two sets oftraffic lights, under railway bridgeand through a third set of lights toBalmoral Avenue.Continue along Balmoral Avenue tojunction with Malone Road.Take the slip road on the left on toMalone Road.Guide for Young PatientsBy trainThe nearest train station is BotanicStation. It is a 30-minute walk or10-minute taxi journey to the Clinic.
St.St.Rd.k.Donegal RdRd.LisbuStEm ranmba illnk ismentMalornd.lis RneRd.nmilA1Boucher Rd.RdStraM1aumeOrUniversTates Avenueity Rd.A1ShaftesburySquare.ac StCromBRo roaun dwda ayboutinWest LA24St.Great VictoriaGrosvenorOxford St.riaVictoDivisRd.M1Lisburn Rd.StockmansLaneKing’sHallOuter RingBalmoral Av.A55MaloneRd.illisanmStr25
The Ulster Independent Clinic isaccredited by CHKS. The primaryobjective of accreditation is tohelp healthcare organisationsimprove their managementand operational systems, anddemonstrate their ability toprovide quality services. Theclinic undergoes regular reviewsand service improvements tomaintain this accreditation.Guide for Young PatientsThe HDSU department of theUlster Independent Clinic isaccredited by ISO.
FAIR PROCESSING NOTICE1: What is the purpose of this document?2: Data Protection PrinciplesUlster Independent Clinic (the “Clinic”) iscommitted to protecting the privacy andsecurity of your personal information.We will comply with data protection law.This says that the personal information wehold about you must be:This fair processing notice describes how wecollect and use personal information aboutyou during and after your treatment, inaccordance with the General Data ProtectionRegulation (GDPR).1. Used lawfully, fairly and in a transparentway.Ulster Independent Clinic is a “datacontroller” for any of your personal data itholds. This means that we are responsiblefor deciding how we hold and use personalinformation about you. We are requiredunder data protection legislation to notifyyou of the information contained in thisprivacy notice.The Consultant/s providing your privatemedical treatment at the Clinic are joint“data controllers” in relation to your personaldata which they hold for the provision ofyour private medical care.This notice is for all patients of the Clinic.We reserve the right to update this privacynotice at any time. We may also notify youin other ways from time to time about theprocessing of your personal information.If you have any questions about this fairprocessing notice or how we handle yourpersonal information, please contact theDPO, Company Secretary at 028 9066 1212.You have the right to make a complaint atany time to the Information Commissioner’sOffice (ICO), the UK supervisory authority fordata protection issues2. Collected only for valid purposes that wehave clearly explained to you and not usedin any way that is incompatible with thosepurposes.3. Relevant to the purposes we have told youabout and limited only to those purposes.4. Accurate and kept up to date.5. Kept only as long as necessary for thepurposes we have told you about.6. Kept securely.3: The kind of information we hold about youPersonal data, or personal information,means any information about an individualfrom which that person can be identified. Itdoes not include data where the identity hasbeen removed (anonymous data).There are “special categories” of moresensitive personal data which require ahigher level of protection.We will collect, store, and use certain personalinformation about you which includes:Non-sensitive personal data:– Personal contact details such as name, title,addresses, telephone numbers and personalemail addresses.– Personal details such as date of birth,gender, marital status, photographic IDand dependants.– Next of kin and emergency contactinformation.– Medical insurance details, includingmembership numbers and compensationhistory.27
FAIR PROCESSING NOTICE– Payment information, including paymentmethods, bank/card details and billingaddress.Sensitive personal data:– Details of your health comprising recordsof treatments and care received, includingnotes and reports about your health fromyour GP.– Results of x-rays, blood tests and otherrelevant medical examinations.4: How is your personalinformation collected?We collect personal information aboutpatients through the referral process, eitherdirectly from the patient or sometimesfrom the patient’s GP, consultant or otherhealthcare provider by a referral letter,medical insurance provider or in someinstances from a legal representative.Situations in which we willuse your personal informationWe need all the categories of data in the listabove primarily to allow us to provide anyagreed healthcare services and to enable usto comply with legal obligations. In somecases we may use your personal informationto pursue legitimate interests of our own orthose of third parties, provided your interestsand fundamental rights do not overridethose interests. The situations in which wewill process your personal information arelisted below.– Administering our healthcare services asagreed.– To help inform the decisions yourconsultant and healthcare team makeabout your treatment.– To ensure that your treatment is safe andeffective.The Clinic will collect additional personalinformation in the course of providing yourprivate medical care.– To work effectively with the joint datacontrollers who may be involved in yourcare.5: How we will use yournon-sensitive personal data– To prevent fraud.We will only use your personal informationwhen the law allows us to. Most commonly,we will use your personal information in thefollowing circumstances:1. Where we need to perform an agreementwe have entered into with you.2. Where we need to comply with a legalobligation.3. Where it is necessary for our legitimateinterests (or those of a third party) andyour interests and fundamental rights donot override those interests.We may also use your personal informationin the following situations, which are likelyto be rare:1. Where we need to protect your interests(or someone else’s interests).2. Where it is needed in the public interest.Guide for Young Patients– Complying with health and safetyobligations.– Where it is needed in relation to legalclaims or where it is needed to protect yourinterests (or someone else’s interests).Some of the above grounds for processingwill overlap and there may be several groundswhich justify our use of your personalinformation.Change of purposeWe will only use your personal informationfor the purposes for which we collected it,unless we reasonably consider that we needto use it for another reason and that reasonis compatible with the original purpose. If weneed to use your personal information for anunrelated purpose, we will notify you and wewill explain the legal basis which allows usto do so.Please note that we may process yourpersonal information without yourknowledge or consent, in compliance withthe above rules, where this is required orpermitted by law.
6: How we use particularlysensitive personal data7: Data SharingWe may have to share your data“Special categories” of particularly sensitivepersonal information require higher levelsof protection. We need to have furtherjustification for collecting, storing and usingthis type of personal information. We have inplace an appropriate security and safeguardswhich we are required by law to maintainwhen processing such data. We may processspecial categories of personal information inthe following circumstances:1. Primarily for carrying out our legalobligations in connection with your medicalcare for the purpose of preventative oroccupational medicine, medical diagnosis,provision of health or social care ortreatment or the management of healthand social care systems and services,carried out under the supervision of ahealth professional or another person whoowes a duty of confidentiality under law(being your consultant/s).2. In limited circumstances, with yourexplicit written consent.3. Less commonly, we may process this typeof information where it is needed in relationto legal claims or where it is needed toprotect your interests (or someone else’sinterests) and you are not capable of givingyour consent, or where you have alreadymade the information public.Do we need your consent?We do not need your consent if we use specialcategories of your personal information inaccordance with our written policy to carryout our legal obligations or exercise specificrights in the field of your medical care. Inlimited circumstances, we may approach youfor your written consent to allow us to processcertain particularly sensitive data. If we doso, we will provide you with full details of theinformation that we would like and the reasonwe need it, so that you can carefully considerwhether you wish to consent. You shouldbe aware that it is not a condition of yourcontract with us tha
you to the Ulster Independent Clinic. We understand that the prospect of your child going into hospital can be worrying - for you as well as your child. Rest assured, we'll make every effort to lessen any anxieties by creating a calming atmosphere for your child and ensuring they're cared for at all times by skilled and professional staff.