Transcription
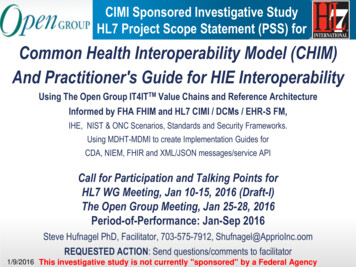
CIMI Sponsored Investigative StudyHL7 Project Scope Statement (PSS) forCommon Health Interoperability Model (CHIM)And Practitioner's Guide for HIE InteroperabilityUsing The Open Group IT4ITTM Value Chains and Reference ArchitectureInformed by FHA FHIM and HL7 CIMI / DCMs / EHR-S FM,IHE, NIST & ONC Scenarios, Standards and Security Frameworks.Using MDHT-MDMI to create Implementation Guides forCDA, NIEM, FHIR and XML/JSON messages/service APICall for Participation and Talking Points forHL7 WG Meeting, Jan 10-15, 2016 (Draft-I)The Open Group Meeting, Jan 25-28, 2016Period-of-Performance: Jan-Sep 2016Steve Hufnagel PhD, Facilitator, 703-575-7912, Shufnagel@ApprioInc.oomREQUESTED ACTION: Send questions/comments to facilitator1/9/2016 This investigative study is not currently "sponsored" by a Federal Agency
The Open Group Healthcare Forum can ad value tothe Common Health Interoperability Model (CHIM) at HL7» The Open Group IT4ITTM Value Chains & Reference Architecture can add architectural rigor» We are vendor-neutral and consensus-driven. We are independent and do not represent anystandard or technology» Forum members are from key organizations around the globe, represent different stakeholdergroups, and contribute innovative thinking» We combine a business and technology orientation with structured approaches—using models,frameworks and architecture-thinking—to help solve real-world business problems» We view health and healthcare from a person-centric perspective. We think health data shouldfollow the person. We reject point-to-point solutions in favour of longitudinal ones» We focus on making existing standards work and encourage collaboration among standardsdevelopment organizations (SDOs)» In short, our orientation to the interoperability problem is holistic and systems-oriented. Thisapproach is aligned with efforts to address the broad goals expressed in the IOM “triple aim”and the “learning healthcare system.” [Jason Lee, The Open Group Healthcare Forum]1/9/2016This is a working document; it is not approved for official use / public distribution.2
The Open Group IT4ITTM Value Chains andReference Architecture Within HL7 SAIF CD “The HL7 Service-Aware Interoperability Framework CanonicalDefinition (SAIF CD) is an architecture for achieving interoperability; but, itis not a whole-solution design for Enterprise architecture management.” “SAIF CD must be adapted to an organization's implementationrequirements through the production of a SAIF implementation Guide.” The Health IT4ITTM Business Value Chains and Health InformationExchange (HIE) Reference Architecture is intended to be the HIEInteroperability Practitioner's SAIF Implementation Guide for “organizationsbuilding large-scale integrated health IT infrastructures at the national level.” This Practitioner's Guide will address the implementers’ conundrum of“models, models everywhere; but, I need to develop, test and deploy aninteroperable solution architecture now.”1/9/2016This is a working document; it is not approved for official use / public distribution.3
Executive Summary (Vision, Goal)» Our vision is to allow for the development of secure free-flow of medical information tobecome a reality, thereby creating a patient/clinician friendly environment; wherecurrently, standards in health IT are numerous and varied across systems, making asmooth Exchange among EHR related systems difficult.» Our goal is for Data Objects to flow across Health IT Systems and their HIE IntegrationComponents supporting Health Business Value Chains; where, a Common Health Interoperability Model (CHIM) is the foundation of an authoritativearchitectural model of the health information landscape and benchmark for health ITstandards; and where, we instantiate the Open Group IT4IT Value Chain and Reference Architecture withHL7 EHR related System Models, System Components and Integration Components.» IT4IT Value Chains define use cases for strategy, requirements, portfolio, deployment,operations, change and error recovery.1/9/2016This is a working document; it is not approved for official use / public distribution.4
Vision/Goal: Common Health Interoperability Model“HIE Interoperability: A Practitioner's Approach”Health IT4ITTM Business Value Chainsand HIE Reference ArchitectureClear, Complete, Concise,Correct and Consistent FullyIntegrated and Tool-BasedArchitectural Model faster, better, cheaper HIEsArchitecture identifies Laws, Policies,Health IT Strategy, Health IT Roadmap,Interoperability Standards Advisory for alearning health system to improve thepatient experience of care, to improvethe health of populations, and to reducethe per capita cost of health care.1/9/2016»»»»Agile, Aligned, InteroperableStrategic, Standards Based, SimpleKnowledge Driven, Reliable, ReusableAccessible, Secure, SustainableThis is a working document; it is not approved for official use / public distribution.5
Executive Summary (Objective, Approach)» The objective, of this 9 month HL7 investigative study, is to demonstrate that we can automatically transform an instance of one data standard into an instanceof another data standard, based on a single shared & documented understanding of information &functional requirements, automatically.– This capability will support actual semantic interoperability among stakeholders currentlyprevented from such interoperability by divergent standards,– and it will do so in a way that enforces consistent semantics across any community that uses it. Demonstrate Open Group IT4IT instantiated with Health IT models and standards, including– Common Information Modelling Initiative (CIMI) archetype models,– Federal Health Information Model (FHIM) and Detailed Clinical Models (DCMs) UML Models Demonstrate archetype versus UML Modeling styles.– Demonstrate UML archetype Modeling Language profile models and CIMI reference models. Document processes, products and tools in “Practitioner's Guide for HIE Interoperability .” Develop a comprehensive HL7 FY2017 Project Scope Statement / Program Plan» The approach will instantiate The Open Group IT4IT Reference Architecture and Value Chain-basedoperating model with Health IT models, Frameworks and artifacts, following a cyclic Agile build, test,evaluate, document and re-plan methodology.1/9/2016This is a working document; it is not approved for official use / public distribution.6
Objective: Common Health Interoperability ModelBusiness Value Chains & HIE Reference ArchitectureCommon Logical Information Model (CLIM)Informed by FHIMCIMI & DCMsLinked to S&IFramework UseCase SimplificationLinked to IBRM &EHR SystemFunctional ModelLinked toNIST Riskand SecurityFrameworkLinked to IHETechnicalFrameworkLinked to NISTHIT Standardsand TestingTool basedTraceability to Laws and RegulationsJurisdictional PoliciesDOD-VA IBRM, ISA, JIPClinical GuidelinesClinical PathwaysQuality MeasuresImplementationsTests and CertificationsMDHT-MDMINIEMFHIRCDA/CCDAXML / JSONObjective is consistent data formats and semantics across implementation paradigms IAW ONC 2015 Interoperability Roadmap1/9/2016This is a working document; it is not approved for official use / public distribution.7
Approach: Common Health Interoperability ModelModel Driven Architecture (MDA)1/9/2016This is a working document; it is not approved for official use / public distribution.8
Schedule: Common Health Interoperability ModelBusiness Value Chains & HIE Reference Architecture» Jan/Feb 2016 – investigative study HL7 Project Scope Statement (PSS)» May/Aug 2016 – Demonstration and draft FY2017 Program Plan» Sept/Oct 2016 – Comprehensive FY2017 HL7 Project Scope Statement» Sept/Oct 2017 – HL7 Draft Standard for Trial Use (DSTU) 1» Sept/Oct 2018 – HL7 Draft Standard for Trial Use (DSTU) 2» Sept/Oct 2019 – HL7 Normative Ballot1/9/2016This is a working document; it is not approved for official use / public distribution.9
AcronymsCDAClinical Document ArchitectureIGImplement GuideCCDAConsolidated CDAIHEIntegrating the Healthcare EnterpriseCLIMCommon Logical Information ModelIMInformation ManagementCMSCenters for Medicare & Medicaid ServicesISAInteroperability Standards AdvisoryDAFData Access FrameworkITInformation TechnologyDBADatabase AnalystJIP(DOD-VA) Joint Interoperability PlanDCMDetailed Clinical ModelMDHTModel Driven Health ToolCIMIClinical Information Modelling InitiativeMDMIModel Driven Message InteroperabilityEHR-S FMEHR System Functions ModelNIEMNational Information Exchange ModelEHR-S FIMEHR System Functions and Information ModelNISTNational Institute of Standards and TechnologyFHIMFederal Health Information ModelNLMNational Library of MedicineHIEHealth Information ExchangeONCUS Health Office of the National CoordinatorHITHealthcare Information TechnologyS&IStandards and InteroperabilityHHSHealth and Human Services AgencySDOStandards Development OrganizationIBRMDoD-VA Integrated Business Reference ModelSMESubject Matter ExpertICIBInteragency Clinical Informatics BoardV2HL7 Version 2 MessagingVLERVirtual Lifelong Electronic Record1/9/2016This is a working document; it is not approved for official use / public distribution.10
Health IT4IT Value Chains & Reference ArchitectureModel-Driven Architecture (MDA)Prioritized ListsISABusinessUse CasesIBRM & EHR SystemFunctions ModelHealth InformationExchange ModelFHIR, NIEM, CDA, CCDA,XML, ASTM, DICOM, NCPDP,X-12, etc.1/9/2016BehaviorBusiness TechnicalFHIM, DCMs,CIMI ArchetypesCommon LogicalInformation ModelInformationPhysicalRepository ModelIHE FrameworkNIST Risk-SecurityFrameworkThis is a working document; it is not approved for official use / public distribution.11
Software Development Lifecycle (SDLC)Health IT MDA Users and UsesNotional User-Story / Use Case1.Clinician Lists are prioritize by Health Data Sharing (HDS) initiatives; where, the lists inform2.Business Use Cases (UCs) developed by Analysts; and, the UCs inform / constrain3.System Objects, Capabilities, Services, and Information Exchange Requirements (IERs) describedby Analysts and Architects, who are informed by» IBRM and/or EHR-S System Functional Model» CLIM informed by FHIM, HL7 Detailed Clinical Models (DCMs) and CIMI models4.System Physical Repositories are specified by Architects and Designers, based on» System Objects, Capabilities, and Services specified as EHR-S FM & FHIM subsets.5.»»»»6.7.System Information Exchanges are specified by Architects & Designers, based onMDHT-MDMI (FHIM) generated Implementation Guides (IGs)» for CDA, NIEM, FHIR and XML/JSON messages/service APIFHIM-based queries/APIs to obtain required data from Physical Repositories.NIST Security Framework and IHE Technical Framework to manage the exchanges.NIST SP-800 Risk Assessment/Management Framework to manage network risk.Implementation Guides (IGs) can be specified by analysts/engineers using MDHT-MDMIDevelopers/testers use IGs to construct/test interoperable information exchanges.1/9/2016This is a working document; it is not approved for official use / public distribution.12
Software Development Lifecycle (SDLC)Health IT MDA Users and UsesPrioritized ListsISAClinical SMEsuse to inform/constrainStakeholdersuse toinformBusinessUse CasesAnalystscreate/use to identify functionsinformFHIM, DCMs,CIMI ArchetypesAnalystscreate/use to identify dataIBRM & EHR SystemFunctions ModelAnalysts and Architectsdefine system objectsand capabilities*Analysts and Architectsconstrain to specify workflow supported byinformHealth InformationExchange ModelArchitects & Designersspecify standard queries,IHE & NIST FrameworksDesigners use MDHT - MDMIto generate Implementation GuidesinformFHIR, NIEM, CDA, CCDA,XML, ASTM, DICOM, NCPDP,X-12, etc.Developersimplement interoperable exchangesTesterscertify interoperable exchanges1/9/2016Clinical SMEsuse to inform/constrainCommon LogicalInformation ModelinformAnalysts and Designersconstrain to specify data/value sets forPhysicalRepository ModelsinformIHE FrameworkNIST Risk-SecurityFrameworkThis is a working document; it is not approved for official use / public distribution.13
Significant Milestones2001-2009 Bush Administration 2004 ONC Established 2005 HITSP established Dec 2005 through Apr 20092009-2017 Obama Administration 2009 ARRA:HITECH Act / VLER Program established 2009 FHIM established, Tim Cromwell & Nancy Orvis, proponents HITSP Lesson Learned MDHT/FHIM needed to empower Developers 2011 DOD-VA iEHR / IPO established by NDAA / S&I Framework Established by ONC 2011 MDHT capable of doing CDA Implementation Guides 2012 FHIM-based Immunization Information Model with CDC 2012 MDHT/FHIM Immunization Implementation Guide/Spec for CDC 2013 FHIM-based Population Health Information Model with CDC 2013 DoD-VA Data Sharing Accelerator Initiative, VistA & DHMSM Modernization announced 2013 MDHT capable of doing NIEM Implementation Guides 2015/6 MDHT capable of doing FHIR Profile / implementation Guide 2017/9 Common Health Interoperability Model & Practitioner's Guide for HIE Interoperability1/9/2016This is a working document; it is not approved for official use / public distribution.14
HL7 Investigative Study Project Scope Statement (PSS) andCall for Participation: Common Health Interoperability Model (CHIM) andPractitioner's Guide for HIE InteroperabilitySteve Hufnagel PhD, Facilitator, 703-575-7912, SHufnagel@ApprioInc.comREQUESTED ACTION: Please send questions/comments to facilitator.1. Project Name and IDProject ID: itCommon Health Interoperability Model (CHIM)And Practitioner's Guide for HIE InteroperabilityTSC Notification Informative/DSTU to NormativeDate :Jan-Sep 2016 Investigative ProjectDate : January 9, 2016 DRAFT I2. Sponsoring Group(s) / Project TeamCIMIPrimary Sponsor/Work Group (1 Mandatory)EHR, PC, CIC, SOACo-sponsor Work Group(s)Co-Sponsor Approval Date CCYY-MM-DDCo-Sponsor Group Approval DateIndicate the level of involvement that the co-sponsor will have for this project:Request formal content review prior to ballotRequest periodic project updates. Specify period: Monthly, at WGMs, etc.Other Involvement. Specify details here:Project Team:Project facilitator (1 Mandatory)Steve HufnagelStan HuffMark JanczewskiJay LyleFacilitatorCIMI Co-chairEHR Co-chairPC co-chairCIC co-chairSOA co-chairGary DickinsonS&I Simplification co-chairNancy OrvisDoD Proponent*Bob BishopVA Proponent*Nona HallIPO Proponent*Gail Kalbfleisch FHIM Sponsor*Jason LeeThe Open Group HealthcareForum* This project is not currently "sponsored" by afederal agency.Other interested parties and their rolesMulti-disciplinary project team (recommended)Modeling facilitatorPublishing facilitatorVocabulary facilitatorDomain expert repSteve Hufnagel2016-01-09-DRAFT-I HL7-PSS for2015 ReleaseCommon Health InteroperabilityModel.docx 2016 Health Level Seven International. All rights reservedPage 1 of 8
Business requirement analystConformance facilitator (for IG projects)Other facilitators (SOA, SAIF)Implementers (2 Mandatory for DSTU projects)NOT APPLICABLE FOR INVESTIGATIVE Project3. Project Definition3.a. Project Scope Our vision is to allow for the development of secure free-flow of medicalinformation to become a reality, thereby creating a patient/clinician friendlyenvironment; where currently, standards in health IT are numerous and varied acrosssystems, making a smooth Exchange among EHR related systems difficult.Our goal is for Data Objects to flow across Health IT Systems and their HIEIntegration Components supporting Health Business Value Chains; where,a Common Health Interoperability Model (CHIM) is the foundation of an authoritativearchitectural model of the health information landscape and benchmark for healthIT standards; and where,we instantiate the Open Group IT4IT Value Chain and Reference Architecture withHL7 EHR related System Models, System Components and Integration Components.IT4IT Value Chains define use cases for strategy, requirements, portfolio,deployment, operations, change and error recovery.The objective, of this 9 month HL7 investigative study, is todemonstrate that we can automatically transform an instance of one data standardinto an instance of another data standard, based on a single shared & documentedunderstanding of information & functional requirements, automatically.This capability will support actual semantic interoperability among stakeholderscurrently prevented from such interoperability by divergent standards,and it will do so in a way that enforces consistent semantics across any communitythat uses it.Demonstrate Open Group IT4IT instantiated with Health IT models and standards,includingCommon Information Modelling Initiative (CIMI) archetype models,Federal Health Information Model (FHIM) and Detailed Clinical Models (DCMs) UMLModelsDemonstrate archetype versus UML Modeling styles.Demonstrate UML archetype Modeling Language profile models and CIMI referencemodels.Document processes, products and tools in “Practitioner's Guide for HIEInteroperability .”Develop a comprehensive HL7 FY2017 Project Scope Statement / Program PlanThe approach will instantiate The Open Group IT4IT Reference Architecture andValue Chain-based operating model with Health IT models, Frameworks and artifacts,following a cyclic Agile build, test, evaluate, document and re-plan methodology.This Investigative Project is not currently "sponsored" by a federal agency.2016-01-09-DRAFT-I HL7-PSS for2015 ReleaseCommon Health InteroperabilityModel.docx 2016 Health Level Seven International. All rights reservedPage 2 of 8
3.b. Project NeedThe Need to Architect the Health Information Standards LandscapeStandards in health IT are numerous and varied across systems, making a smooth exchange of EHRs difficult; where,Secure exchange of meaningful healthcare information requires that parties agree upon a common application ofstandards that define the type of content being exchanged and the manner in which this takes place. But currently,numerous standards exist. There are different standards that define content from their most basic elements andexpected values through their packaging and transmission frameworks. There are numerous developmentorganizations that support health information technology. It is not uncommon to perform a target scan of theenvironment and discover relevant healthcare standards supported by a standards development organization whoseprimary purpose is other than healthcare. Numerous standards utilized for the same purpose often exist within asingle standards development organization. Choices of standards, standards bodies, and archetypes appear to havea geographical component as well with nations tending to favor one approach over the other.The fluidity of the landscape in health information technology and the high level of information security that isneeded to protect patient information has created a very difficult environment. For instance, it is currently much harderfor systems to exchange a medical record than it is for an ATM machine to exchange information regardingidentification of an account and available credit.An authoritative architectural model of the present international health information landscape would benefit thehealth information technology vendor community. It would create a benchmark for health IT standards, allowing forthe development of a secure free-flow of medical information to become a reality and creating a patient/clinicianfriendly environment. [Gail Kalbfleisch, FHA Director]Interoperability is not simply a technical issue, a leadership issue, an organizational issue, or a money issue. Rather,it is all of these, considered together in an integrated manner. To do this, we simplify by representing the fundamentalstructure of health care systems in a landscape in which key actors produce essential actions. This simplificationmakes it is easier to identify barriers and gap-filling steps necessary for improvement and advancement In this waywe can see both gaps and benefits. In short, our orientation to the interoperability problem is holistic and systemsoriented. We do not believe solutions are merely technical. Rather, they build on a keen understanding of theinterdependence of the key elements of the healthcare landscape. This approach is aligned with efforts to addressthe broad goals expressed in the “triple aim” and the “learning healthcare system.”1 [Jason Lee, The Open GroupHealth Forum]The US-based Institute for Healthcare Improvement (IHI) coined the term “Triple Aim” in 2007 to refer to “thesimultaneous pursuit of improving the patient experience of care, improving the health of populations, and reducingthe per capita cost of health care. . . The IHI Triple Aim framework often functions as a statement of purpose forhealth care system transformation that will better meet the needs of people and patients. Its successfulimplementation will result in fundamentally new systems contributing to the overall health of populations whilereducing the cost to society.”1(http://www.ihi.org/communities/blogs/ layouts/ihi/community/blog/itemview.aspx?List 81ca4a47-4ccd-4e9e-89d9-14d88ec59e8d&ID 63, accessed October 28, 2015.)The US Institute of Medicine (IOM) describes a learning healthcare system as one that is “designed to generateand apply the best evidence for the collaborative healthcare choices of each patient and provider; to drive theprocess of discovery as a natural outgrowth of patient care; and to ensure innovation, quality, safety, and value inhealth care. IOM 20122016-01-09-DRAFT-I HL7-PSS for2015 ReleaseCommon Health InteroperabilityModel.docx 2016 Health Level Seven International. All rights reservedPage 3 of 8
The Healthcare Forum at The Open Group can help this Health IT work at HL7 because:» The Open Group IT4ITTM Value Chains & Reference Architecture can add architecturalrigor» We are vendor-neutral and consensus-driven. We are independent and do not representany standard or technology» Forum members are from key organizations around the globe, represent differentstakeholder groups, and contribute innovative thinking» We combine a business and technology orientation with structured approaches—usingmodels, frameworks and architecture-thinking—to help solve real-world businessproblems» We view health and healthcare from a person-centric perspective. We think health datashould follow the person. We reject point-to-point solutions in favour of longitudinal ones» We focus on making existing standards work and encourage collaboration amongstandards development organizations (SDOs)» In short, our orientation to the interoperability problem is holistic and systems-oriented.This approach is aligned with efforts to address the broad goals expressed in the IOM“triple aim” and the “learning healthcare system.” [Jason Lee, The Open GroupHealthcare Forum]The Open Group IT4ITTM Value Chains and Reference Architecture Within HL7 SAIF CD» “The HL7 Service-Aware Interoperability Framework Canonical Definition (SAIFCD) is an architecture for achieving interoperability; but, it is not a whole-solution designfor Enterprise architecture management.”» “SAIF CD must be adapted to an organization's implementation requirements through theproduction of a SAIF implementation Guide.”» The Health IT4ITTM Business Value Chains and Health Information Exchange (HIE)Reference Architecture is intended to be the HIE Interoperability Practitioner's SAIFImplementation Guide for “organizations building large-scale integrated health ITinfrastructures at the national level.”» This Practitioner's Guide will address the implementers’ conundrum of “models, modelseverywhere; but, I need to develop, test and deploy an interoperable solution architecturenow.”3.c. Success CriteriaApproved FY2017 comprehensive PSS3.d. Project RisksRisk Description:Impact:Likelihood:Risk Type:Risk To HL7:Mitigation Plan:TBD in FY2017 PSSCriticalHighRequirementsInternal to alExternal to HL7LowTechnology2016-01-09-DRAFT-I HL7-PSS for2015 ReleaseCommon Health InteroperabilityModel.docx 2016 Health Level Seven International. All rights reservedPage 4 of 8
3.e. Security Risks TBD in FY2017 PSSWill this project produce executable(s), for example, schemas, transforms,stylesheets, executable program, etc. If so the project must review anddocument security risks.YesNoUnknown3.f. External DriversDoD and VA EHR modernization and interoperability, CDC Public Health initiatives,CMS and FDA initiatives.3.g. Project Objectives / Deliverables / Target DatesFirst “work-in progress” Investigative Project demo / lessons-learnedDemonstration, FY2017 Program PlanComprehensive FY2017 Common Health Interoperability Model (CHIM)PSS for HL7 review/processing Example Health IT4IT CLIM informed by FHIM, CIMI, DCMs Example Health IT4IT Business Value Chains & Reference Architecture Example MDHT-MDMI IG for CDA, NIEM, FHIR and XML/JSONmessages/service API Prototype Users Guide for Common Health Interoperability Model (CHIM) & Tools FY2017 Work Breakdown Structure (WBS) / Program Plan Risks and risk mediations identifiedTarget DateMay 2016 HL7 WG mtg.June-Aug 2016Sep 2016 HL7 WH mtg.3.h. Common Names / Keywords / AliasesCIMI, DCM, FHIM, HIT, CLIM, NIEM, FHIR, CDA, V2, IT4IT, HL7, Open Group3.i. LineageNA3.j. Project RequirementsThe Investigative Project will demonstrate The Open Group IT4IT processes and products including the HIT-CLIM Specificationof “Common Clinical Data Set” IAW ONC “Connecting Health and Care for theNation: A Shared Nationwide Interoperability Roadmap” Traceability too Use Case Simplification (S&I Framework Project)o IHE Technical Frameworko EHR-S Functional Modelo NIST Security and Risk Frameworko Interoperability Standards Advisory, Strategy and Roadmap XMI support for Use Case Authoring Tool (UCAT)and/or UML SDLC Tools, such asSparx EA, IBM RSA, MagicDraw, NIST Prometheus, open source Papyrus3.k. Project DependenciesFHIM, CIMI, DCMs, EHR-S FM, FHIR, OpenGroup IT4IT, S&I Framework Use CaseSimplification, eclipse.org MDHT3.l. Project Document Repository LocationCIMI wiki3.m.Backwards Compatibility2016-01-09-DRAFT-I HL7-PSS for2015 ReleaseCommon Health InteroperabilityModel.docx 2016 Health Level Seven International. All rights reservedPage 5 of 8
Click here to go to Appendix A for more information regarding this section and FHIR project instructions.YesAre the items being produced by this project backward compatible?YesFor V3, are you using the current data types?If you check 'No' please explain the reason:NoUnknownN/ANo3.n. External VocabulariesClick here to go to Appendix A for more information regarding this section.YesNoUnknownN/AWill this project include/reference external vocabularies?If yes, please list the vocabularies: Vocabularies used by CIMI, FHIM and DCMs such as, but not limited to,SNOMED, LOINC, RxNorm4. ProductsNon Product Project- (Comprehensive HL7 PSS for FY2017)Arden SyntaxClinical Context Object Workgroup (CCOW)Domain Analysis Model (DAM)Electronic Health Record (EHR) Functional ProfileLogical ModelV2 Messages – AdministrativeV2 Messages - ClinicalV2 Messages - DepartmentalV2 Messages – InfrastructureFHIR ResourcesFHIR ProfilesNew/Modified/HL7 Policy/Procedure/ProcessNew Product DefinitionNew Product FamilyV3 Domain Information Model (DIM / DMIM)V3 Documents – Administrative (e.g. SPL)V3 Documents – Clinical (e.g. CDA)V3 Documents - KnowledgeV3 Foundation – RIMV3 Foundation – Vocab Domains & Value SetsV3 Messages - AdministrativeV3 Messages - ClinicalV3 Messages - DepartmentalV3 Messages - InfrastructureV3 Rules - GELLOV3 Services – Java Services (ITS Work Group)V3 Services – Web Services (SOA)5. Project Intent (check all that apply)Create new standardRevise current standard (see text box below)Reaffirmation of a standardNew/Modified HL7 Policy/Procedure/ProcessWithdraw an Informative DocumentN/A (Project not directly related to an HL7 Standard)Supplement to a current standardImplementation Guide (IG) will be created/modifiedProject is adopting/endorsing an externally developed IG:Specify external organization in Sec. 6 below;Externally developed IG is to be (select one):Adopted - OR EndorsedComprehensive FY2017 PSS forCommon Health Interoperability Model (CHIM)And Practitioner's Guide for HIE Interoperability5.a. Ballot Type (check all that apply)Comment Only for Investigative ProjectInformativeDSTU to NormativeNormative (no DSTU)Joint Ballot (with other SDOs or HL7 Work Groups)N/A (project won’t go through ballot)Investigative Project in support of a comprehensive FY2017 PSS to define DSTU and ultimately a normative ballot.5.b. Joint CopyrightCheck this box if you will be pursuing a joint copyright. Note that when this box is checked, a Joint Copyright Letter of Agreement must besubmitted to the TSC in order for the PSS to receive TSC approval.Joint Copyrighted Material will be producedTBD for FY2017 PSS2016-01-09-DRAFT-I HL7-PSS for2015 ReleaseCommon Health InteroperabilityModel.docx 2016 Health Level Seven International. All rights reservedPage 6 of 8
6. Project Logistics6.a. External Project CollaborationInclude SDOs or other external entities you are collaborating with, includinggovernment agencies as well as any industry outreach. Indicate the nature andstatus of the Memorandum of Understanding (MOU) if applicable.TBD for FY2017 PSSFor projects that have some of their content already developed:100% for InvestigativeHow much content for this project is already developed?ProjectThe Open Group IT4ITWas the content externally developed (Y/N)? YESReference Architecture,FHA FHIM,NIST Security &Risk Framework, IHETechnical Framework,ONC S&I SimplificationApproval date CCYY-MM-DDDate of external content review by the ARB? TBD for FY2017 PSSYesNoIs this a hosted (externally funded) project? (not asking for amount just iffunded)6.b. RealmUniversalRealm SpecificCheck here if this standard balloted or was previousl
DAF Data Access Framework IT Information Technology DBA Database Analyst JIP (DOD-VA) Joint Interoperability Plan DCM Detailed Clinical Model MDHT Model Driven Health Tool CIMI Clinical Information Modelling Initiative MDMI Model Driven Message Interoperability EHR-S FM EHR System Functions Model NIEM National Information Exchange Model