Transcription
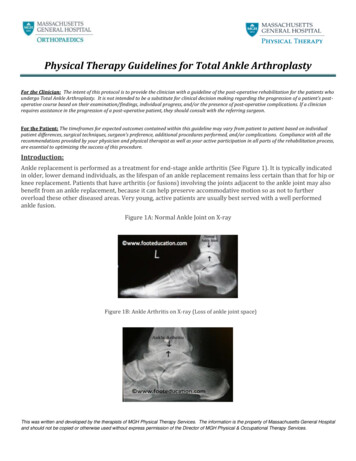
Physical Therapy Guidelines for Total Ankle ArthroplastyFor the Clinician: The intent of this protocol is to provide the clinician with a guideline of the post-operative rehabilitation for the patients whoundergo Total Ankle Arthroplasty. It is not intended to be a substitute for clinical decision making regarding the progression of a patient’s postoperative course based on their examination/findings, individual progress, and/or the presence of post-operative complications. If a clinicianrequires assistance in the progression of a post-operative patient, they should consult with the referring surgeon.For the Patient: The timeframes for expected outcomes contained within this guideline may vary from patient to patient based on individualpatient differences, surgical techniques, surgeon’s preference, additional procedures performed, and/or complications. Compliance with all therecommendations provided by your physician and physical therapist as well as your active participation in all parts of the rehabilitation process,are essential to optimizing the success of this procedure.Introduction:Ankle replacement is performed as a treatment for end-stage ankle arthritis (See Figure 1). It is typically indicatedin older, lower demand individuals, as the lifespan of an ankle replacement remains less certain than that for hip orknee replacement. Patients that have arthritis (or fusions) involving the joints adjacent to the ankle joint may alsobenefit from an ankle replacement, because it can help preserve accommodative motion so as not to furtheroverload these other diseased areas. Very young, active patients are usually best served with a well performedankle fusion.Figure 1A: Normal Ankle Joint on X-rayFigure 1B: Ankle Arthritis on X-ray (Loss of ankle joint space)This was written and developed by the therapists of MGH Physical Therapy Services. The information is the property of Massachusetts General Hospitaland should not be copied or otherwise used without express permission of the Director of MGH Physical & Occupational Therapy Services.
Physical Therapy Guidelines for Total Ankle ArthroplastySurgical Procedure:In all ankle replacements, the arthritic surface of the distal tibia (lower leg) is removed, as is the arthritic surface ofthe top surface talus (Figure 2). The resected areas of bone are then replaced with the prosthesis. The prosthesistypically has a metal surface on the tibia and talaris sides, with a polyethylene surface that articulates betweenthem to facilitate motion.Figure 2: Tornier Saltos Talaris Total Ankle ReplacementReference: footeducation.comThis was written and developed by the therapists of MGH Physical Therapy Services. The information is the property of Massachusetts General Hospitaland should not be copied or otherwise used without express permission of the Director of MGH Physical & Occupational Therapy Services.
Physical Therapy Guidelines for Total Ankle ArthroplastyPhasePre-operativePhase 1:0-2 weeksRestrictions and Precautions-Weight bearing as tolerated(WBAT)-Non-weight bearing in splintper MDPhysical Therapy TreatmentGoals-Instruct with use of assistivedevice based on gaitassessment, NWB on affectedside-Demonstrate safe ambulationwith assistive device NWB-Edema management andeducation regarding elevation oflimb-Manage swelling via elevationof limb and icing-Education regardingmonitoring skin surroundingincision for infection. Thisincludes increased temperature,increased drainage from wound,and a wound that is not healing.-Gait training and safety(emphasize precautions withweight bearing)-Able to maintain NWB withtransfers and stairs-Demonstrate safe ambulationwith assistive device NWB-Able to maintain NWB withtransfers and stairs-Perform ADLs in a modifiedindependent manner or withminimal assistance- Maintain range of motion andstrength of hip/knee/core-Education/modifications forADLs- Active movement of the hipand knee including isometrics(as instructed by PT to maintainprecautions)Phase 2:2-6 weeks-Splint removed, transition towalker boot per MD. Stichesmay remain in for 2-4 weeks- Weight bearing when standingONLY, maintain non-weightbearing while walking- Can remove boot to performexercises and hygiene. Keepboot on at night.-Exercises and hands-ontechniques (by the PT) for footand ankle active and passiverange of motion-Strengthening for core, hips,knees (maintain precautions)-Weight shifting with boot andassistive device (maintainprecautions)- Manage swelling via elevationof limb and icing-Increase range of motion offoot and ankle-Minimize the loss of strength inthe core, hips, and knees-Independence with homeexercise program to beperformed daily-Gait training to ensure safetyand to normalize pattern asweight bearing is allowedThis was written and developed by the therapists of MGH Physical Therapy Services. The information is the property of Massachusetts General Hospitaland should not be copied or otherwise used without express permission of the Director of MGH Physical & Occupational Therapy Services.
Physical Therapy Guidelines for Total Ankle ArthroplastyPhase 3:6-10 weeks-Wean from boot to be WBAT inshoe at 8 weeks, if the wound iscompletely healed.-No strengthening againstresistance until 3 months if anytendon transfers-No stretching tendons iftransferred-Ankle active/passive range ofmotion, stretching, and lightstrengthening.-Continuation of progressions ofhip/core exercises-Can begin cycling on stationarybicycle-Improve range of motion footand ankle-A normalized gait pattern on allsurfaces out of bootwith/without a walking aid asneeded-Joint mobilization/soft tissuemobilization techniques by thePT to restore motion of the footand ankle, including scarmassage-Activity progression per PTinstructions-Gait training to wean off theassistive devices and normalizegaitPhase 4:-None if healing complete10-14 weeks-Continue treatment as above-Proprioception and balanceexercises as appropriate by PT-Progressive resistive exercisesof the ankle as tolerated,continue progressinghip/knee/core exercises asappropriate by PTPhase 5:14-16 weeks-No repetitive, high impactsports or occupations-Continue treatment as above-Single leg activities progressinginto higher level balance andproprioceptive exercises- Bilaterally heel raisesprogressing into unilateral heelraises-Continue improving anklestrength and ROM- Normal ambulation without awalking aid-Begin to improvebalance/proprioceptive capacityof surgical ankle- Good balance and control onthe involved leg in all planes-Full ROM of ankle complexIdeal ROM GoalDorsiflexion: 10 degreesPlantarflexion: 35 degrees5/5 strength of anklemusculature (includingtransferred tendons ifapplicable)Phase 6:16 weeks 1 year -No repetitive, high impactsports or occupations-No repetitive, high impactsports or occupations-Continue treatment as above-Sport specific training andconditioning (avoid high impactforces of the ankle)-Continue maintenance homeexercise program for strengthand mobility-Participation in non-highimpact sports-Gradual return to functionalactivities, low impact/no impactsports-Full strength of the foot/ankle-Continue to maintain strengthand mobility of ankle and foot topreserve the life of thecomponents-Return to low/no impact sportsThis was written and developed by the therapists of MGH Physical Therapy Services. The information is the property of Massachusetts General Hospitaland should not be copied or otherwise used without express permission of the Director of MGH Physical & Occupational Therapy Services.
Physical Therapy Guidelines for Total Ankle ArthroplastyAdditional InformationPain and swelling:This is a procedure that can cause swelling for up to 6-12 months post-op. Redness does not necessarily indicateinfection but would be worrisome with the presence of progressive or persistent pain. Significant drainage fromthe wound is usually a sign of infection.Return to work:Return to work at a full sedentary job no earlier than 3-4 weeks post-op. Return to work at a job requiringsignificant amounts of standing or walking no earlier than 4 months post-op. Return to work for jobs with physicalrequirements between the above extremes is individualized (If uncertain, please contact the surgeon).Important: No patient with a total ankle arthroplasty should be doing a job, sport, or activity causingsignificant, repetitive, high impact to the joint.If you have any questions or concerns related to the content of these rehabilitation guidelines, please contact:MGH Physical and Occupational Therapy Services (MG Waltham)781-487-3800Website: http://www.massgeneral.org/physical-therapy/MGH Orthopedics Foot and Ankle617-724-9338Website: http://www.massgeneral.org/ortho-foot-ankle/This was written and developed by the therapists of MGH Physical Therapy Services. The information is the property of Massachusetts General Hospitaland should not be copied or otherwise used without express permission of the Director of MGH Physical & Occupational Therapy Services.
Physical Therapy Guidelines for Total Ankle Arthroplasty. This was written and developed by the therapists of MGH Physical Therapy Services. The information is the property of Massachusetts General Hospital and should not be copied or otherwise used without express permission of the Director of MGH Physical & Occupational Therapy Services. Phase 3:










