Transcription
ARTICLE IN PRESSSocial Science & Medicine 61 (2005) 1971–1982www.elsevier.com/locate/socscimedFood insufficiency and women’s mental health: Findings froma 3-year panel of welfare recipientsColleen M. Heflina, , Kristine Siefertb, David R. WilliamscaMartin School of Public Policy, University of Kentucky, 429 POT, Lexington, KY 40503, USANIMH Research Center on Poverty, Risk, and Mental Health, University of Michigan, 1080 S. University, Ann Arbor,MI 48109-1106, USAcInstitute for Social Research, University of Michigan, 426 Thompson Street, Rm. 2230, Ann Arbor, MI 48106-1248, USAbAvailable online 31 May 2005AbstractHousehold food insufficiency is a significant problem in the United States, and has been associated with poor outcomeson mental health indicators among low-income women. However, it is difficult to disentangle the mental healthconsequences of household food insufficiency from poverty and other shared risk factors. Drawing on theories of thesocial production of health and disease, research evidence linking food insufficiency with poor mental health, and highrates of food insufficiency among welfare recipients, we examined whether a change in household food insufficiency isassociated with a change in women’s self-reported mental health in a sample of current and recent welfare recipients overa 3-year period of time, controlling for common risk factors. Data were obtained from a prospective survey of womenwho were welfare recipients in an urban Michigan county in February 1997 (n ¼ 753). We estimated fixed effect modelsfor changes in mental health status that make use of information on household food insufficiency gathered in the fall of1997, 1998, and 1999. The relationship between household food insufficiency and respondents’ meeting the diagnosticscreening criteria for major depression remained highly significant even when controlling for factors known to conferincreased risk of depression and time invariant unobserved heterogeneity. These findings add to growing evidence thathousehold food insufficiency has potentially serious consequences for low-income women’s mental health. If confirmedby further research, they suggest that the public health burden of depression in welfare recipients and other low-incomewomen could be reduced by policy-level interventions to reduce their exposure to household food insufficiency.r 2005 Elsevier Ltd. All rights reserved.Keywords: Food insufficiency; Food security; Low-income women; Mental health; Depression; USAIntroductionThe Personal Responsibility and Work OpportunityReconciliation Act of 1996 eliminated entitlements to Corresponding author. Tel.: 1 859 257 8608;fax: 1 859 323 1923.E-mail addresses: cmh@uky.edu (C.M. Heflin),ksiefert@umich.edu (K. Siefert), wildavid@umich.edu(D.R. Williams).cash benefits for low-income families with children,imposed work requirements and a 5-year lifetime limiton benefits, and separated cash assistance from foodassistance. The maximum Food Stamp benefit wasreduced, and TANF recipients who leave welfare maylose Food Stamp benefits altogether. The number offood stamp recipients fell from a historic high of 27.5million in 1994 to 17.4 million by the end of 1999;welfare caseloads fell by 50% over this same time period(US Council of Economic Advisors, 1999). Since then,0277-9536/ - see front matter r 2005 Elsevier Ltd. All rights reserved.doi:10.1016/j.socscimed.2005.04.014
ARTICLE IN PRESS1972C.M. Heflin et al. / Social Science & Medicine 61 (2005) 1971–1982food stamp caseloads have rebounded to 22 million inJuly 2003, the most recent month available (USDA,2003). With the movement of millions of families fromwelfare to work, increased food insecurity and hungerand their effects on the well-being of current and recentwelfare recipients are a rising concern (Mills, Dorai-Raj,Peterson, & Alwang, 2001; Lerman & Wiseman, 2002).High rates of food insecurity, food insufficiency, andhunger1 are a significant problem in the United States(Alaimo, Briefel, Frongillo, & Olson, 1998). In 2000,10.5% of US households—over 33 million people—wereestimated to live in food insecure households, meaningthat at some time during the previous year, they wereunable to acquire or were uncertain of having enoughfood to meet basic needs due to inadequate householdresources (Nord, Kabbani, Tiehen, & Andrews, 2002).Among these, 3.3 million households were food insufficient, meaning that they were food insecure to the extentthat one or more household members went hungry atleast some time during the year because they could notafford food (Nord et al., 2002). Food insecurity wassubstantially higher among households with incomesbelow the poverty line and households with childrenheaded by a single woman, who had rates of 36.8% and31.0%, respectively. Among 753 women sampled fromthe welfare rolls in an urban county in Michigan andsurveyed a year later, 25% reported that their householdsometimes or often did not have enough to eat(Corcoran, Heflin, & Siefert, 1999). Food insufficiencywas higher among those who reported health and mentalhealth problems.Persistently high rates of household food insufficiencypose a significant problem, potentially affecting bothphysical and psychological well-being (Olson, 1999;Campbell, 1991; Dixon et al., 2001). However, it isdifficult to disentangle the health and psychosocialconsequences of food scarcity from those of povertyand other common risk factors (Olson, 1999; Campbell,1991). Building on previous work, the present studyinvestigates the effects of food insufficiency on current1Survey researchers use various terms to describe foodscarcity and deprivation. ‘‘Food insecurity’’ refers to the limitedor uncertain availability of food, while ‘‘food insufficiency’’refers to restricted household food stores or insufficient foodintake (Scott & Wehler, 1998). ‘‘Hunger’’ refers narrowly toinsufficient food intake. Food insecurity differs conceptuallyfrom food insufficiency and hunger, which can be consideredroughly equivalent (Rose, 1999). The distinction between foodinsufficiency and food insecurity or hunger can best beunderstood from a temporal frame of reference: food insecuritycan be experienced prior to the onset of food insufficiency orhunger, and may or may not result in food insufficiency orhunger (Scott & Wehler, 1998). Food insecurity with hunger, ameasure recently adopted by the United States Department ofAgriculture, is conceptually comparable to food insufficiency(Dixon, Winkleby, & Radimer, 2001).and recent welfare recipients’ mental health over a3-year time period. Using a fixed effects modeland controlling for potentially common risk factors,we examine the effects of changes in food insufficiencyon changes in two mental health indicators: respondents’ meeting the diagnostic screening criteriafor major depressive disorder and their sense ofmastery. We hypothesize that household food insufficiency will be associated with higher risk of depressionand lower levels of mastery, while controlling formeasured factors known to affect women’s mentalhealth and well-being and time invariant unobservedheterogeneity.Background: food insufficiencyRates of food insufficiency vary considerably by race,gender, and household income. The Third NationalHealth and Nutrition Examination Survey (NHANESIII) found rates of food insufficiency to be 11.8% amonglow-income whites, 13.5% among low-income nonHispanic Blacks, and 24.8% among low-income Mexican Americans (Alaimo et al., 1998). Low-middleincome single female-headed families with childrenwere 5.5 times more likely than other family typesto be food insufficient. More recently, the USDAfound that in 2000, the prevalence of food insecuritywith hunger (one or more household members werehungry, at least some time during the year, becausethey could not afford enough food) was 3.1%, or3.3 million households (Nord et al., 2002). Households with annual income below 185% of the povertyline were seven times more likely to report hunger thanthose with higher income (Nord et al., 2002). Foodinsecurity with hunger was 12.7% among householdswith incomes below the official poverty line, 9.0%among families headed by a single woman, 6.5% amongBlack households, and 4.8% among Hispanic households.Importantly, researchers have begun to establish arelationship between an inadequate household foodsupply and lower energy and nutrient intakes amongwomen. Rose and Oliveira (1997) analyzed the diets ofadult women in the 1989–1991 Continuing Survey ofFood Intake by Individuals and reported that householdfood insufficiency was significantly associated with lowenergy and nutrient intakes. This finding, based on asingle 24-h recall, does not necessarily imply dietaryinadequacy, but it supports the use of self-reportedhunger measures as valid indicators of increased risk ofdietary inadequacy (Sidel, 1997). Additional evidencecomes from a study of 145 women in families receivingemergency food assistance in Toronto; those reportinghunger in their household during the past monthreported systematically lower intakes of energy andnutrients, controlling for a broad range of potential
ARTICLE IN PRESSC.M. Heflin et al. / Social Science & Medicine 61 (2005) 1971–1982behavioral, economic, and sociocultural factors thatmight influence diet (Tarasuk & Beaton, 1999).A recent study by Dixon et al. (2001) found thatadults in food insufficient households were more likelyto have potentially health-compromising diets thanadults from food sufficient families, and also had lowerserum concentrations of essential nutrients, elevating therisk of a number of major chronic diseases. Thesefindings should be interpreted cautiously due to smallsample size and other methodological limitations, butthe observed association between systematically lowreported nutrient intakes and food insecurity withmoderate or severe hunger, independent of otherpotential influences on diet, supports concerns thatwomen in food insufficient households may be at higherrisk of nutrient shortfalls that can ultimately affect theirhealth and well-being.Poor mental health among the welfare-to-work populationFueled by increasing concern regarding welfarerecipients’ ability to meet federally mandated workrequirements in the post-welfare reform era, a growingbody of literature documents a high prevalence ofmental health problems and other barriers to employment among the welfare population. These barriersinclude depression, anxiety, and substance abuse disorders, physical health problems, and domestic violence(Olson & Pavetti, 1996; Kalil et al., 1998; Zedlowski &Loprest, 1999; Danziger et al., 2000; Polit, London, &Martinez, 2001). Given the growing emphasis of statewelfare programs on rapid labor market entry, mentalhealth disorders, which are strongly associated withreduced employment and earnings, are of particularconcern (Marcotte & Wilcox-Gok, 2001).Depression in particular has received considerableattention because it is a disabling and costly illness thatis highly prevalent among welfare recipients. High ratesof major depression among women receiving welfarehave been documented (Jayakody, Danziger, & Pollack,2000; Siefert, Bowman, Heflin, Danziger, & Williams,2000; Lennon, 2001); a recent review found that 44.5%reported depressive symptoms and a median of 22% metthe diagnostic criteria for major depression (Lennon,Blome, & English, 2002). Depression is associated withsubstantial impairment in vocational and social functioning (Wells, Stewart, & Hays, 1989; Murray & Lopez,1996; Kessler & Frank, 1997; Dewa & Lin, 2000), and isof concern to policy-makers trying to move women fromwelfare-to-work because it is associated with lower levelsof work and increased welfare receipt (Lehrer, Crittenden, & Norr, 2005; Horowitz & Kerker, 2001; Danzigeret al., 2000). In addition, welfare recipients must contendwith the demands of parenting while trying to meetfederally mandated work requirements, and maternaldepression has been associated with numerous adverse1973health and developmental consequences for children(Field, 1992; Leadbeater & Bishop, 1994; Heneghan,Johnson Silver, Westbrook, Stein, & Bauman, 1998).Recent research on the causes and course of depression indicates that social and environmental factors, thatis, stressful life events and conditions, confer increasedrisk for its onset and recurrence (Checkley, 1996;McEwen, 1998; Frank & Thase, 1999). Depression isassociated with hypothalamic dysfunction, specificallyhypercortisolism, and the effects of social and environmental risk factors probably operate through the highlystress-responsive hypothalamic–pituitary–adrenocortical (HPA) axis (Gold, Goodwin, & Chrousos, 1988;Checkley, 1992; Rubin, 1989; McEwen, 1998). Up totwo-thirds of those who experience one episode of majordepression suffer a recurrence, and multiple episodesincrease both risk of recurrence and length and severityof subsequent episodes (Wells, Sturm, Sherbourne, &Meredith, 1996; Frank & Thase, 1999). Thus, it is ofgreat importance to identify modifiable risk factorsrelated to a change in depression status.Research has also demonstrated that women receivingwelfare have lower levels of a sense of mastery thansimilar women not on welfare (Petterson & Friel, 2001;Kunz & Kalil, 1999). Mastery, a psychological constructthat captures perceptions about oneself as a causal agentin one’s environment, is widely considered a fundamental characteristic that affects individuals’ ability toinfluence their environment and control important lifeoutcomes (Rothbaum, Weisz, & Snyder, 1982). It is thebelief that one can hold one’s own life and solve one’sproblems (Lombardi & Ulbrich, 1997). High levels ofmastery and control have been inversely related tosocioeconomic status (Mirowsky & Ross, 1986), andpositively related to physical and mental health (Rodin,1986; Karasek, Tehorell, Schwartz, Peiper, & Alfredson,1982; Petterson & Friel, 2001; Danziger, Carlson, &Henley, 2001).Food insufficiency and poor mental healthAlthough the possible bi-directionality in the relationship between household food insufficiency and mentalhealth must be considered, it is quite plausible thathousehold food insufficiency could adversely affect themental health of welfare recipients. First, householdfood insufficiency may be subjectively experienced asstressful, and its presence or persistence could initiate ormaintain feelings of self-blame and the perception thatone is not efficacious. An individual’s sense of mastery islargely a consequence of experiencing oneself asefficacious (Gecas & Schwalbe, 1983), and exposure tostressful life experiences can erode one’s sense of mastery(Kraus & Tran, 1989). Likewise, the association betweencumulative or persistent stressful life events or conditions and onset or chronicity of depression, particularly
ARTICLE IN PRESS1974C.M. Heflin et al. / Social Science & Medicine 61 (2005) 1971–1982among single mothers with low self-esteem and lack ofsupport, is well documented (Brown & Harris, 1978;Costello, 1982; Brown & Moran, 1997).Second, food insufficiency could impair mental healththrough the direct effect of nutritional shortfalls onpsychological functioning and behavior. Even the earlystages of nutrient deficiency can adversely affect behaviorand mental performance; in an experimental study of 1081young men in good health, reduced vitamin intake over a2-month period was associated with negative changes inpsychological disposition and functioning (Heseker, Kubler, Pudel, & Westenhoffer, 1992). Inadequate vitaminintake was associated with increased irritability, nervousness, depression, feelings of fear and decreased well-being,memory and reaction performance. Importantly, several ofthese effects were reversed by providing vitamin supplements. More recent studies have focused on the role ofvitamin B12 and folate deficiency on depression anddementia (Tiemeier et al., 2002; Alpert, Mischoulon,Nirenberg, & Fava, 2000; Reynolds, 2002).Drawing on theories of the social production of healthand disease, which posit that an individual’s social andeconomic positioning determines their exposure tohealth-damaging risk factors (Krieger, Rowley, Herman, Avery, & Phillips, 1993; Krieger & Zierler, 1995;Link & Phelan, 1995; Williams, Yu, Jackson, &Anderson, 1997; Denton & Walters, 1999); researchevidence linking food insufficiency with poor health; andhigh rates of food insufficiency among welfare recipients, Siefert, Heflin, Corcoran, and Williams (2001)hypothesized that household food insufficiency couldcontribute to poor health and mental health in thispopulation. In a cross-sectional analysis that controlledfor other factors known to influence women’s health andwell-being, food insufficiency remained a significantpredictor of self-rated health, limitations in physicalfunctioning, and major depression. However, a limitation of this study was its cross-sectional design.The same authors then analyzed the relationshipbetween household food insufficiency and women’shealth in the same sample at two points in time: fall1997 and approximately 1 year later (Siefert, Heflin,Corcoran, & Williams, 2004). Controlling for commonrisk factors, women who reported food insufficiency atboth times were significantly less likely to report a highsense of mastery over their lives. Food insufficiency atwave 2 only was significantly associated with meetingthe diagnostic screening criteria for recent majordepression, as well as with a lower sense of mastery.These findings have potentially important implications;unlike household food insufficiency, many risk factorsfor depression, such as low socioeconomic status,gender, or genetic disposition, are global or not readilymodified (National Advisory Mental Health CouncilWork Group on Mental Disorders Prevention Research,1998). If food insufficiency is a contributing or causalfactor in major depression, preventing or ameliorating itmight reduce the risk of onset or recurrence of this costlyand disabling illness. However, these findings may bebiased due to the presence of unobserved heterogeneityand therefore, are not conclusive. The present study usesa fixed effects model to address this limitation bycontrolling for unmeasured time invariant factors.MethodsStudy design and sampleDetails of the data set and survey methods aredescribed elsewhere (Danziger et al., 2000). Briefly, weanalyzed data from the first three waves of the Women’sEmployment Study, a panel survey of barriers toemployment among 753 mothers who were receivingcash assistance in an urban Michigan county inFebruary 1997. Trained staff of the Survey ResearchCenter of the Institute for Social Research of theUniversity of Michigan conducted face-to-face, inhome, structured interviews between August and December 1997, August and December 1998, and November 1999 and March 2000. The first two interviews lastedapproximately 1 h; the third, about 90 min. Women wereeligible if they resided in the study county, received cashassistance in February 1997, were single and a US citizenbetween the ages of 18 and 54, and claimed a racialidentity of white or African-American (there were toofew other minority residents of this county to conductreliable analyses).A simple random sampling scheme was used. Caseswere systematically selected with equal probability froman ordered list of eligible single mothers. To derive arepresentative sample of the metropolitan area and thestudy population, cases were proportionately selected byzip code, race (African American or non-Hispanicwhite), and age. The response rate was 86.2% at waveone; 92% at the second wave; and 91% at the thirdwave. In the first wave about half the respondents wereAfrican-American, 27.0% were aged 35 years or older,36.8% had three or more children, and 31.2% had notcompleted high school. Given the very low attrition ratebetween each of the waves and subsequent analysesindicating that surveyed respondents do not differ fromattriters on characteristics such as race, food insufficiency, and the two outcomes examined here, the risk ofattrition bias is quite low. Therefore, the data were notweighted. Table 1 presents descriptive statistics from thepooled sample for variables used in the analysis.Variables assessed and definitionsFood insufficiency was defined narrowly as restrictedhousehold food stores or too little food intake among
ARTICLE IN PRESSC.M. Heflin et al. / Social Science & Medicine 61 (2005) 1971–1982Table 1Descriptive statistics (standard deviations)VariableMeanTotal numberof observationsFood umber of other adultsin the householdNumber of children inthe householdNet monthly householdincomeNeighborhood hazardsStressful lifecircumstancesDomestic violenceSex discriminationRace discrimination0.24 (0.42)0.20 (0.40)22.05 (3.35)0.31 (0.46)1.31 (0.70)201820162010201720172.34 (1.38)20181460.36 (904.38)201816.06 (4.49)2.15 (1.70)196020150.14 (0.35)0.37 (0.82)0.31 (0.71)201719841987either adults or children in the household (Scott &Wehler, 1998) and was operationalized using thequestion: ‘‘Which of the following describes the amountof food your household has to eat—enough to eat,sometimes not enough to eat, or often not enough toeat?’’ This single-item measure is widely accepted as avalid measure of food insufficiency (Rose and Oliveira,1997; Alaimo et al., 1998; Rose, 1999). Following theconvention that has been adopted in related research(Alaimo et al., 1998), we coded respondents as foodinsufficient who answer ‘‘sometimes’’ or ‘‘often.’’We operationalized our dependent variable, women’smental health, by using measures of both negative andpositive aspects of mental health and psychologicalfunctioning: major depression and sense of mastery.Major depression was assessed using the 12-monthscreening version of the World Health Organization’s(WHO) Composite International Diagnostic Interview(CIDI) (WHO, 1990; Kessler, Andrews, Mroczek,Ustun, & Wittchen, 1998). WHO field trials and othermethodological studies (Wittchen, 1994; Blazer, Kessler,McGonagle, & Swartz, 1994) have documented acceptable test–retest reliability and clinical validity of theCIDI diagnoses. We measured mastery, which refers tothe degree to which individuals perceive themselves to bein control of their own lives, by using the seven-itemPearlin Mastery Scale (Pearlin, Lieberman, Menaghan,& Mulan, 1981), a widely used measure of this constructwith a range of 0–28.Our independent variables include sociodemographicand personal characteristics known to be associated withwomen’s mental health, including number of children inthe household, marital status, the number of other1975adults in the household, and annual gross householdincome. A woman is coded as married if she is marriedor living with her partner.In keeping with our theoretical perspective on thesocial production of disease, we examined a broad arrayof social and environmental risk factors related to race,gender, and social class and known to be associated withincreased risk of mental health problems among women(Adler, Boyce, Chesney, Folkman, & Syme, 1993;Alaimo et al., 1998; Bassuk et al., 1996; Brown &Moran, 1997; Corcoran et al., 1999; Denton & Walters,1999; Kendall, Olson, & Frongillo, 1996; Link & Phelan,1995; Rose, 1999; Siefert et al., 2000, 2001). Thesefactors include poverty-related stressful life circumstances, such as homelessness or utility shutoffs, andliving in a hazardous neighborhood. We also measureddomestic violence, which has been shown to adverselyaffect physical and mental health among women and hasalso been associated with food insufficiency (Corcoranet al., 1999; Siefert et al., 2001; Tolman & Rosen, 1998).We also controlled for self-reported experiences ofdiscrimination based on race or gender. Perceiveddiscrimination has been associated with poor physicaland mental health (Kessler, Mickelson, & Williams,1999; Krieger et al., 1993; Williams, Neighbors, &Jackson, 2003), and women of color are disproportionately represented among the food insufficient (Bickel,Carlson, & Nord, 1999).Stressful life circumstances were defined as positiveresponses to an 11-item measure which we adapted forthis study from the Difficult Life Circumstances scale,which was developed by Booth, Mitchell, Barnard, andSpieker (1989) and adapted for use in the New Chancestudy of young mothers in poverty by Quint, Bos, andPolit (1997). Items measure ongoing or habitualstressors that are often a feature of living in poorcommunities, such as utility shutoff, eviction, andhomelessness. Neighborhood hazards were measuredusing an 11-item scale developed by Furstenberg, Cook,Eccles, Elser, and Sameroff (1998), which asks respondents to rate the presence of such problems as muggings,gangs, vandalism, and lack of police protection in theirneighborhood.Domestic violence was measured using items drawnfrom the Conflict Tactics Scale (Straus & Gelles, 1986), awidely used measure of family violence. In the presentstudy, respondents were defined as having experienceddomestic violence if they reported experiencing any ofthe six indicators of severe physical violence (hit with afist, hit with an object, beaten, choked, threatened orassaulted with a weapon, or forced into sexual activity)by a partner within the past year.Questions about perceived discrimination based onrace or gender were adapted from items used in surveysby Bobo (1995) and Williams et al. (1997). Discrimination based on race was defined as the number of positive
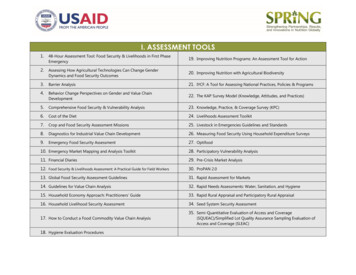
ARTICLE IN PRESSC.M. Heflin et al. / Social Science & Medicine 61 (2005) 1971–19821976responses to a series of five questions that asked aboutunfair treatment while seeking employment or in theworkplace, including whether respondents thought theyhad ever been refused a job, fired, or not promotedbecause of their race. Discrimination based on gender wasdefined the number of positive responses to a series ofsix questions which asked about unfair treatment whileseeking employment or in the workplace, includingwhether respondents thought they had ever been refuseda job, fired, or not promoted because of their sex,whether they had been sexually harassed, and if theirsupervisor made insulting remarks about women.Data analysisWe estimate fixed effect models for the change inmental health status. Changes in food insufficiency arethe main independent variables. This method has oneprincipal advantage. By controlling for all individualspecific factors that are constant over time, it eliminatescertain kinds of omitted variable biases in crosssectional research (Powers & Xie, 2000). With ordinaryleast squares regression, a component of the error termmay be correlated with other independent variables inthe model. Suppose that individual temperament affectsreports of both mental health and food insufficiency. Itcould be, for example, that women with outlooks thatare more negative than average are also more likely torate themselves as sometimes not having enough food toeat. In that case, the effect of food insufficiency ondepression status observed by Siefert et al. (2004) may bebiased due to personality characteristics not measureddirectly. Our analysis controls for unmeasured individual traits that affect both mental health and foodinsufficiency, as long as their effect does not change overtime.The specific fixed effect model used in this paper isshown in Eq. (1). Each variable in the equation isaveraged over all assessed time points for a specificwoman. This average value is then subtracted from thevalue at a specific time point for that woman. As aresult, the time invariant measured and unmeasuredcharacteristics for a specific woman, such as race, dropout of the modelY it Y i : ¼ ait ai : þ b1 ðfood insf it food insf i :Þþ g1 ðcontrolsit controlsi :Þ þ it i .ð1Þ2Hausman tests were performed to test for correlationof the omitted variables with other regressors in theequation and were all highly statistically significant(po0:001). Since depression is a dichotomous outcome,2If the Hausman tests were not significant, this would haveindicated that the omitted variables were randomly distributedwith respect to the error term and that random effect, and notfixed effect, models were appropriate.we use a conditional fixed effect logistic regressionmodel; mastery is modeled using linear fixed effectmodels.Using fixed effect models has one main conceptualdisadvantage that renders it an inappropriate methodfor some questions in that time invariant measuredcharacteristics are dropped from the model. This meansthat background characteristics such as race are notincluded in the analysis. Additionally, the interpretationof the relationship between the prime variable ofinterest, in this case food insufficiency, and the outcome(depression or mastery) is that of the change in X (foodinsufficiency) that is associated with the change in Y(depression or mastery). Consequently, this analysisdoes not yield any new information about respondentswho are persistently depressed nor can it speak to thecumulative effects on mental health of persistent foodinsufficiency.3 This paper examines whether a change infood insufficiency is associated with a change in mentalhealth.We estimate three nested models to examine theindependent effects of three sets of factors on our twodependent variables. In Model 1, we begin by showingthe bivariate relationships between food insufficiencyand each of the dependent variables. In Model 2, wecontrol for the household composition and householdincome. In Model 3, we control for the social andenvironmental risk factors described above.ResultsTable 1 presents descriptive statistics for variablesused in the analysis. Approximately one-quarter of theobservations meet the criteria for food insufficiency. Onein five meet the criteria for major depression and themean mastery score is 22. The average householdconsists of 1.31 adults and 2.34 children. Almost onethird of the observations report living with a husband oropposite-sex domestic partner. Mean net monthlyhousehold income is 1460. The average score
Campbell, 1991; Dixon etal., 2001). However, itis difficult to disentangle the health and psychosocial consequences of food scarcity from those of poverty and other common risk factors (Olson, 1999; Campbell, 1991). Building on previous work, the present study investigates the effects of food insufficiency on current