Transcription
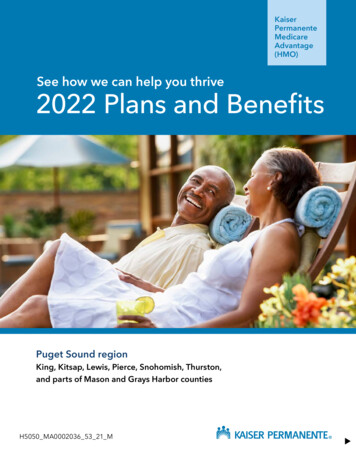
Delta Dental PPOOur nationalPoint-of-ServiceprogramUniversity of MichiganDental PlanWelcome!Delta Dental Plan of Michigan, Inc. is a nonprofit dental care corporation, doing business as Delta Dental ofMichigan. Delta Dental of Michigan is the state’s dental benefits specialist. Good oral health is a vital part of goodgeneral health, and your Delta Dental program is designed to promote regular dental visits. We encourage you to takeadvantage of this program by calling your Dentist today for an appointment.This Certificate, along with your Summary of Dental Plan Benefits, describes the specific benefits of your DeltaDental program and how to use them. If you have any questions about this program, please call our Customer Servicedepartment at (800) 524-0149 or access our Web site at www.deltadentalmi.com.You can easily verify your own benefit, claims and eligibility information online 24 hours a day, seven days a week byvisiting www.deltadentalmi.com and selecting the link for our Consumer Toolkit. The Consumer Toolkit will alsoallow you to print claim forms and ID cards, search our dentist directories, and read oral health tips.We look forward to serving you!
TABLE OF CONTENTSI.Dental Care Certificate .2II.Definitions.2III.Selecting a Dentist .4IV.Accessing Your Benefits .5V.How Payment is Made .6VI.Classes of Benefits.6Summary of Option 1 Dental Plan Benefits .8VII.Option 1 Exclusions and Limitations.9Summary of Options 2 & 3 Dental Plan Benefits.12VIII.Options 2 & 3 Exclusions and Limitations .13IX.Coordination of Benefits.17X.Informal Claims Appeal Procedure.18XI.Termination of Coverage .20XII.Continuation of Coverage .20XIII.General Conditions .20Note: This Dental Care Certificate should be read in conjunction with the Summary of Dental Plan Benefits that is providedwith the Certificate. The Summary of Dental Plan Benefits lists the specific provisions of your group dental Plan.1Form No. UMMIPPOPOSRevised 10/2008
Control Plan (Delta Dental)I. Delta Dental PPODental Care CertificateThe Delta Dental Plan that contracts with the University.The Control Plan will provide all claims processing,service, and administration for a group. The Summary ofDental Plan Benefits identifies your Control Plan. TheControl Plan will be referred to as Delta Dental in thisdocument.Delta Dental issues this Certificate to you, theSubscriber. The Certificate is an easy-to-read summaryof your dental benefits Plan. It reflects and is subject tothe agreement between Delta Dental and the Universityof Michigan.Concurrent Care ClaimsThe benefits provided under the Plan may change if anystate or federal laws change.Claims for benefits where an ongoing course of treatmenthas been agreed to by Delta Dental and/or the administratorof your Plan and the coverage for that treatment is reducedor terminated before the treatment has been completed. AConcurrent Care Claim may also arise if you ask the Planto extend coverage beyond the time period or number oftreatments previously agreed to.Delta Dental agrees to provide dental benefits asdescribed in this Certificate.All the provisions in the following pages form a part ofthis document as fully as if they were stated over thesignature below.CopaymentIN WITNESS WHEREOF, this Certificate is executed atDelta Dental’s home office by an authorized officer.As provided by your Plan, the percentage of the charge,if any, that you will have to pay for Covered Services.Covered ServicesThomas J. Fleszar, DDS, MSPresident and CEODelta Dental Plan of Michigan, Inc.The unique benefits selected in your Plan. The Summaryof Dental Plan Benefits provided with this Certificatelists the Covered Services provided by your Plan.II. DefinitionsDeductibleThe amount a person and/or a family must pay towardCovered Services before Delta Dental begins paying forservices. The Summary of Dental Plan Benefits lists theDeductible that applies to you, if any.CertificateThis document. Delta Dental will provide dental benefitsas described in this Certificate. Any changes in thisCertificate will be based on changes to the Plan.Delta DentalChildrenEligibility is determined by the University of Michigan.Delta Dental Plan of Michigan, Inc., a dental carecorporation providing dental service benefits. DeltaDental is not a commercial insurance company.Completion DatesDelta Dental PlanSome procedures may require more than one appointmentbefore they can be completed. Treatment is complete:An individual dental benefit plan that is a member of theDelta Dental Plans Association, the nation’s largest, mostexperienced system of dental health plans. For dentures and partial dentures, on the delivery dates;Delta Dental PPO (Point-of-Service) For crowns and bridgework, on the cementationdates;Delta Dental’s national preferred provider organizationprogram that can reduce your out-of-pocket expenses ifyou receive care from one of Delta Dental’s PPO For root canals and periodontal treatment, on thedate of the final procedure that completes treatment.2Form No. UMMIPPOPOSRevised 10/2008
Dentists. This program has back-up coverage throughDelta Dental Premier when treatment is received from anon-PPO Dentist.eligibility. Please note, however, that under nocircumstances can you cover: Anyone who works for the University and has his orher own coverage as an employee of the University;Delta Dental Premier Any dependent child who works for the Universityand is eligible for benefits as an employee of theUniversity; orDelta Dental’s national fee-for-service dental benefitsprogram that covers you when you go to a non-PPODentist. Any eligible dependents who are already covered byanother employee of the University, unless you arecourt-ordered to provide such coverage.DentistA person licensed to practice dentistry in the state orcountry in which dental services are rendered.Maximum Approved Fee Delta Dental PPO Dentist (PPO Dentist) orParticipating Dentist – a Dentist who has signed anagreement with the Delta Dental Plan in his or her stateto participate in Delta Dental PPO. PPO Dentists agreeto accept Delta Dental’s fee determination as paymentin full for Covered Services.A system used by Delta Dental to determine theapproved fee for a given procedure for a given DeltaDental Premier Dentist. A fee meets MaximumApproved Fee requirements if it is the lowest of: The Submitted Amount. Delta Dental Premier Dentist (Premier Dentist) orParticipating Dentist – a Dentist who has signed anagreement with the Delta Dental Plan in his or herstate to participate in Delta Dental Premier. DeltaDental Premier Dentists agree to accept DeltaDental’s fee determination as payment in full forCovered Services. The lowest fee regularly charged, offered, or receivedby an individual Dentist for a dental service,irrespective of Dentist’s contractual agreement withanother dental benefits organization. The maximum fee that the local Delta Dental Planapproves for a given procedure in a given regionand/or specialty, under normal circumstances.Wherever a term of this Certificate differs from yourstate Delta Dental and its agreement with aParticipating Dentist, the agreement in that state withthat Dentist will be controlling.Delta Dental may also approve a fee under unusualcircumstances.Participating Dentists are not allowed to charge DeltaDental patients more than the Maximum Approved Feefor the Covered Service. In all cases, Delta Dental willmake the final determination about what is theMaximum Approved Fee for the Covered Service. Nonparticipating Dentist – a Dentist who has notsigned an agreement with Delta Dental to participatein Delta Dental PPO or Delta Dental Premier. Out-of-Country Dentist – A Dentist whose office islocated outside of the United States and itsterritories. Out-of-Country Dentists are not eligibleto sign participating agreements with Delta Dental.Maximum PaymentThe maximum dollar amount Delta Dental will pay inany benefit year or lifetime for covered dental services.(See the Summary of Dental Plan Benefits.)PPO Dentist ScheduleNonparticipating Dentist FeeThe maximum amount allowed per procedure forservices rendered by a PPO Dentist as determined bythat Dentist’s local Delta Dental Plan.The maximum fee allowed per procedure for servicesrendered by a Nonparticipating Dentist.Eligible DependentOut-of-Country Dentist FeeDependent eligibility is determined by the University ofMichigan. Contact the University for specificinformation about your plan’s rules for dependentThe maximum fee allowed per procedure for servicesrendered by an Out-of-Country Dentist.3Form No. UMMIPPOPOSRevised 10/2008
PlanSummary of Dental Plan BenefitsThe arrangement for the provision of dental benefits toeligible people established by the contract between DeltaDental and your employer or organization.A description of the specific provisions of your groupdental Plan. The Summary of Dental Plan Benefits isincluded in this Dental Care Certificate.Post-Service ClaimsUrgent Care ClaimsClaims for benefits that are not conditioned on yourseeking advance approval, certification, or authorizationto receive the full amount of any covered benefit. Inother words, Post-Service Claims arise when you receivethe dental service or treatment before you file a claim forthe benefit payment.Those potentially life-threatening claims as defined inthe U.S. Department of Labor Regulations at 29 CFR2560.503-1(M)(1)(I). Any such claims that may ariseunder this dental coverage are not considered to be PreService Claims and are not subject to anyPredetermination requirements.Predetermination (Pre-Service Claims)III. Selecting a DentistAn estimate of the costs of Covered Services to beprovided. A Dentist may submit his or her treatment planto Delta Dental before providing services. Delta Dentalreviews the treatment plan and advises you and yourDentist of what services are covered by your Plan andwhat Delta Dental’s payments may be. Delta Dental’spayment for predetermined services depends oncontinued eligibility and the annual or lifetimeMaximum Payments available under your Plan. You arenot required to seek a Predetermination. You will receivethe same benefits under your Plan whether or not aPredetermination is requested. Predetermination ismerely a convenience so that you will know before thedental service is provided how much, if any, of the costof that service is not covered under your Plan. Since youmay be responsible for any cost not covered under yourPlan, this is likely to be useful information for you whendeciding whether to incur those costs.You may choose any Dentist. Your out-of-pocket costsare likely to be less if you go to a Delta Dental PPODentist. PPO Dentists agree to accept payment accordingto the PPO Dentist Schedule, and, in most cases, thisresults in a reduction of their fees. Delta Dental may alsopay a higher percentage for Covered Services if you goto a PPO Dentist.If the Dentist you select is not a PPO Dentist, you willhave back-up coverage through Delta Dental Premier.Again, your out-of-pocket expenses will vary dependingon the participating status of the Dentist. Your coveragelevels may be slightly lower, but you can still savemoney. In this case, there are two options: If you go to a non-PPO Dentist who participates inDelta Dental Premier, the fee reduction is not thesame as with the PPO Dentists. However, PremierDentists agree to accept Delta Dental’s MaximumApproved Fee as payment in full for CoveredServices.Processing PoliciesDelta Dental’s policies and guidelines used forPredetermination and payment of claims. The ProcessingPolicies may be amended from time to time. If you choose a Dentist who does not participate ineither program, you will be responsible for anydifference between Delta Dental’s allowed fee andthe Dentist’s Submitted Fee, in addition to anyCopayment.Submitted Amount or Submitted FeeThe fee a Dentist bills to Delta Dental for a specifictreatment.A list of Participating Dentists will not be provided as itchanges frequently and is accurate only as of the date itis printed. To verify that a Dentist is a ParticipatingDentist, you can use Delta Dental’s online DentistDirectory at www.deltadentalmi.com or call (800) 5240149.SubscriberYou, when your employer or organization notifies DeltaDental that you are eligible to receive dental benefitsunder your employer’s or organization’s Plan.4Form No. UMMIPPOPOSRevised 10/2008
within 12 months of the date the services werecompleted. If there is not enough information to decideyour claim, Delta Dental will notify you or your Dentistwithin 30 days. The notice will (a) describe theinformation needed, (b) explain why it is needed, (c)request an extension of time in which to decide theclaim, and (d) inform you or your Dentist that theinformation must be received within 45 days or yourclaim will be denied. You will receive a copy of anynotice that is sent to your Dentist. Once Delta Dentalreceives the requested information, it will have 15 daysto decide your claim. If you or your Dentist fails tosupply the requested information, Delta Dental will haveno choice but to deny your claim. Once Delta Dentaldecides your claim, it will notify you within five days.IV. Accessing YourBenefitsTo use your Plan, follow these steps:1. Please read this Certificate and the Summary ofDental Plan Benefits carefully so you are familiarwith the benefits, payment mechanisms, andprovisions of your Plan.2. Make an appointment with your Dentist and tell himor her that you have dental benefits coverage withDelta Dental. If your Dentist is not familiar withyour Plan or has questions about the Plan, have himor her contact Delta Dental by (a) writing DeltaDental, Attention: Customer Service, P.O. Box30416, Lansing, Michigan, 48909-7916, or (b)calling the toll-free number, (800) 524-0149.If you have been approved for a course of treatment andthat course of treatment is reduced or terminated before ithas been completed, or if you wish to extend the course oftreatment beyond what was agreed upon, you may file aConcurrent Care Claim seeking to restore the remainderof the treatment regimen or extend the course oftreatment. All Concurrent Care Claims will be decided insufficient time so that, if your claim is denied (in whole orin part), you can seek a review of that decision before thecourse of treatment is scheduled to terminate.3. After you receive your dental treatment, you or thedental office staff will file a claim form, completingthe information portion with:a. The Subscriber’s full name and address;b. The Subscriber’s Member ID number;c. The name and date of birth of the personreceiving dental care;You may also appoint an authorized representative todeal with the Plan on your behalf with respect to anybenefit claim you file or any review of a denied claimyou wish to pursue (see the Claims Appeal Proceduresection). You should call Delta Dental’s CustomerService department, toll-free, at (800) 524-0149, or writethem at P.O. Box 30416, Lansing, Michigan, 489097916, to request a form to fill out designating the personyou wish to appoint as your representative. While insome circumstances your Dentist may be treated as yourauthorized representative, generally only the person youhave authorized on the last dated form filed with DeltaDental will be recognized. Once you have appointed anauthorized representative, Delta Dental willcommunicate directly with your representative and willnot inform you of the status of your claim. You will haveto get that information from your representative. If youhave not designated a representative, Delta Dental willcommunicate with you directly.d. The group’s name and number.Claims and completed information requests should bemailed to:Delta DentalP.O. Box 9085Farmington Hills, Michigan 48333-9085Delta Dental recommends Predetermination before yourDentist provides any services where the total chargeswill exceed 200. Predetermination is not a prerequisiteto payment, but it allows claims to be processed moreefficiently and allows you to know what services will becovered before your Dentist provides them. You andyour Dentist should review your PredeterminationNotice before treatment. Once treatment is complete, thedental office will enter the dates of service on thePredetermination Notice and submit it to Delta Dentalfor payment.If you have questions regarding your plan or coveragecall Delta Dental’s Customer Service department, tollfree, at (800) 524-0149. You may also write to DeltaDental’s Customer Service department, P.O. Box 30416,Lansing, Michigan, 48909-7916. When writing to DeltaDental, please include your name, the group’s name andBecause the amount of your benefits is not conditionedon a Predetermination decision by Delta Dental, allclaims under this Plan are Post-Service Claims. Once aclaim is filed, Delta Dental will decide it within 30 daysof receiving it. All claims for benefits must be filed5Form No. UMMIPPOPOSRevised 10/2008
The Subscriber will be responsible for the lesser ofthe Maximum Approved Fee or the Dentist'sSubmitted Amount for most commonly-performednoncovered services. For other noncoveredservices, the Subscriber will be responsible for theDentist's Submitted Amount.number, the Subscriber’s Member ID number, and yourdaytime telephone number.V. How Payment is Made1.If the Dentist is a PPO Dentist and a Premier Dentist,Delta Dental will base payment on the lesser of:4.a. The Submitted Amount;b. The PPO Dentist Schedule; ora. The Submitted Amount; orc. The Maximum Approved Fee.b. The Nonparticipating Dentist Fee.Delta Dental will send payment to the PPO Dentist,and the Subscriber will be responsible for anydifference between Delta Dental’s payment and thePPO Dentist Schedule or the Maximum ApprovedFee for Covered Services. The Subscriber will beresponsible for the lesser of the PPO ScheduleAmount, the Maximum Approved Fee, or theDentist's Submitted Amount for most commonlyperformed noncovered services. For other noncoveredservices, the Subscriber will be responsible for theDentist's Submitted Amount.2.Delta Dental will usually send payment to theSubscriber, who will be responsible for makingpayment to the Dentist. The Subscriber will beresponsible for any difference between DeltaDental’s payment and the Dentist’s SubmittedAmount.5.For dental services rendered by an Out-of-CountryDentist, Delta Dental will base payment on thelesser of:a. The Submitted Amount; orIf the Dentist is a PPO Dentist but is not a PremierDentist, Delta Dental will base payment on thelesser of:b. The Out-of-Country Dentist Fee.Delta Dental will usually send payment to theSubscriber, who will be responsible for makingpayment to the Dentist. The Subscriber will beresponsible for any difference between DeltaDental’s payment and the Dentist’s SubmittedAmount.a. The Submitted Amount; orb. The PPO Dentist Schedule.Delta Dental will send payment to the PPO Dentist,and the Subscriber will be responsible for anydifference between Delta Dental’s payment and thePPO Dentist Schedule for Covered Services. TheSubscriber will be responsible for the lesser of thePPO Schedule Amount or the Dentist's SubmittedAmount for most commonly-performed noncoveredservices. For other noncovered services, theSubscriber will be responsible for the Dentist'sSubmitted Amount.3.If the Dentist does not participate in Delta DentalPPO or Delta Dental Premier, Delta Dental willbase payment on the lesser of:VI.Classes of BenefitsImportanta. The Submitted Amount; orEligible people are entitled to ONLY those benefitslisted in the Summary of Dental Plan Benefits. Thefollowing is a description of various dental benefits thatcan be selected for a dental program. Please be certain toreview the Summary of Dental Plan Benefits and theExclusions and Limitations section for Option 1 andOption 2 & 3 regarding the benefit information listedbelow.b. The Maximum Approved Fee.Class I BenefitsDelta Dental will send payment to the PremierDentist, and the Subscriber will be responsible forany difference between Delta Dental’s payment andthe Maximum Approved Fee for Covered Services.Diagnostic and Preventive ServicesIf the Dentist is not a PPO Dentist but is a PremierDentist, Delta Dental will base payment on thelesser of:Services and procedures to evaluate existing conditionsand/or to prevent dental abnormalities or disease. These6Form No. UMMIPPOPOSRevised 10/2008
services include examinations/evaluations, prophylaxes,space maintainers, sealants, and fluoride treatments.that are exempt from the Class II and III calendar yeardeductible and 1,250 calendar year maximum underOption 2 and Option 3.)Brush BiopsyMinor Restorative ServicesOral brush biopsy procedure and laboratory analysis todetect oral cancer, an important tool that uses “StarWars” technology to identify and analyze precancerousand cancerous cells. The brush biopsy represents abreakthrough in the fight against oral cancer. Using thisdiagnostic procedure, dentists can identify and treatabnormal cells that could become cancerous, or they candetect the disease in its earliest and most treatable stage.The test is quick, accurate, and involves little or nopatient discomfort.Minor services to repair natural tooth structure damaged bydisease or injury, such as amalgam (silver) fillings, andcomposite resin (white) fillings on anterior and posteriorteeth.Class III BenefitsRelines and RepairsRelines and repairs to bridges, partial dentures, andcomplete dentures.RadiographsMajor Restorative ServicesX-rays as required for routine care or as necessary forthe diagnosis of a specific condition. Covered Servicesinclude full mouth X-rays once every five years andbitewing X-rays no more than once in a Plan Year unlessspecial need is shown.Major restorative services, such as onlays and crowns torebuild natural tooth structure damaged by disease orinjury, when the teeth cannot be restored with anotherfilling material such as amalgam or resin.Class II BenefitsProsthodontic ServicesEmergency Palliative TreatmentServices and appliances that replace missing naturalteeth (such as bridges, endosteal implants, partialdentures, and complete dentures).Emergency treatment to temporarily relieve pain.(Please note: there are limited procedure codes withinthis service that are exempt from the Class II and IIIcalendar year deductible and 1,250 calendar yearmaximum under Option 2 and Option 3.)TMD ServicesOral Surgery ServicesServices to relieve oral symptoms associated withmalfunctioning of the Temporomandibular joint. TMDservices include:Extractions and dental surgery, including preoperativeand postoperative care. Occlusal orthotic TMD device including anyadjustments.Endodontic ServicesClass IV BenefitsThe treatment of teeth with diseased or damaged nerves(for example, root canals). Covered Services include rootcanals and periapical services to treat the root of the tooth.Orthodontic ServicesServices, treatment, and procedures to correct malposedteeth (e.g. braces) for eligible people to age 19.Periodontic ServicesThe treatment of diseases of the gums and supportingstructures of the teeth. This includes periodontal surgeryto remove diseased gum tissue surrounding the teeth,periodontal scaling to remove tartar from the root of thetooth, and treatment of gingivitis and periodontitis(diseases of the gums and gum tissue). (Please note:there are limited procedure codes within this service7Form No. UMMIPPOPOSRevised 10/2008
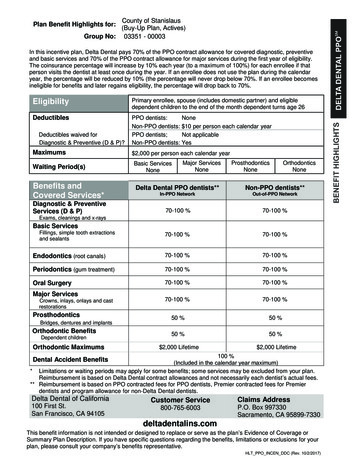
Summary of Dental Plan BenefitsDelta Dental PPO (Point-of-Service)University of Michigan – Group No. 5970Subgroup Numbers:Actives, LTD, COBRA: 1001Retirees & Survivors: 1099OPTION 1PPO DentistCLASS IDiagnostic and Preventive Services – Used to diagnose and/or prevent dentalabnormalities or disease. Includes prophylaxes [cleanings], including periodontalprophylaxes, and routine oral examinations / evaluations payable twice in a calendar year.(People with certain high-risk medical conditions or with a documented history ofperiodontal disease may be eligible for two additional prophylaxes.)Radiographs – Including one set of bitewing X-rays in a calendar year and either apanoramic film or one set of full mouth X-rays once in any five-year period.Sealants – Sealants are payable on permanent bicuspids and molars once per toothper lifetime to age 16.Fluoride Treatment – Preventive fluoride treatments are payable once in a calendaryear for people up to age 14. (People over age 14 with certain high-risk medicalconditions may be eligible for additional prophylaxes or fluoride treatment.)Space Maintainers – Space maintainers are payable for people up to age 19.Premier DentistNonpar %0%0%0%0%0%0%50%50%50%CLASS IIEmergency Palliative Treatment – Used to temporarily relieve pain.Occlusal Guards – Payable once in a five-year period.Periodontal Scaling & Root PlaningPeriodontal Maintenance – Two additional prophylaxes or periodontal maintenanceprocedures will be covered for individuals with a documented history of periodontaldisease. (No more than four prophylaxes [cleanings] and/or periodontal prophylaxes ormaintenance procedures will be payable in a calendar year.)All Other PeriodonticsOral SurgeryMinor Restorative ServicesEndodonticsCLASS IIIRelines & RepairsMajor Restorative ServicesProsthodonticsTMD TreatmentCLASS IVOrthodontic Services (to age 19)Calendar Year and Lifetime Maximum Payable BenefitsThere is no calendar year maximum dollar amountapplied to covered Class I and II services underOption 1.A 1,500 per person total lifetime maximum appliesto covered orthodontic Class IV Benefits. This is acombined maximum under all plan options, even ifyou change dental plan options from year to year.NoneDeductible8Form No. UMMIPPOPOSRevised 10/2008
VII.Option 1Exclusions andLimitationsExclusionsDelta Dental will make no payment for thefollowing services, unless otherwise specified in theSummary of Dental Plan Benefits. All charges forthe following services will be the responsibility ofthe Subscriber (though the Subscriber’s paymentobligation may be satisfied by insurance or someother arrangement for which the Subscriber iseligible):1.Services for injuries or conditions payable underWorkers’ Compensation or Employer’s Liabilitylaws. Benefits or services that are available fromany government agency, political subdivision,community agency, foundation, or similar entity.NOTE: This provision does not apply to anyprograms provided under Title XIX SocialSecurity Act; that is, Medicaid.2.Services, as determined by Delta Dental, forcorrection of congenital or developmentalmalformations, cosmetic surgery, or dentistry foraesthetic reasons.3.Services or appliances started before a personbecame eligible under this Plan. This exclusiondoes not apply to orthodontic treatment inprogress (if a Covered Service).4.Prescription drugs (except intramuscularinjectable antibiotics), medicaments/solutions,premedications, and relative analgesia.9.Treatment by other than a Dentist, except forservices performed by a licensed dentalhygienist under the scope of his or her license.10.Those benefits excluded by the policies andprocedures of Delta Dental, including theProcessing Policies.11.Services or supplies for which no charge ismade, for which the patient is not legallyobligated to pay, or for which no charge wouldbe made in the absence of Delta Dentalcoverage.12.Services or supplies received as a result ofdental disease, defect, or injury due to an act ofwar, declared or undeclared.13.Services that are covered under a hospital,surgical/medical, or prescription drug program.14.Services that are not within the classes ofbenefits that have been selected and that are notin the contract.15.Fluoride rinses, self-applied fluorides, ordesensitizing medicaments.16.Preventive control programs (including oralhygiene instruction, caries susceptibility tests,dietary control, tobacco counseling, home caremedicaments, etc).5.General anesthesia and/or intravenous sedationfor restorative dentistry or for surgicalprocedures, unless medically necessary.6.Charges for hospitalization, laboratory tests, andhistopathological examinations.17.Charges for failure to keep a scheduled visitwith the Dentist.Space maintainers for maintaining space due topremature loss of anterior primary
Delta Dental Plan of Michigan, Inc. is a nonprofit dental care corporation, doing business as Delta Dental of Michigan. Delta Dental of Michigan is the state's dental benefits specialist. Good oral health is a vital part of good general health, and your Delta Dental program is designed to promote regular dental visits. We encourage you to take