Transcription
Delta Dental of North Carolina4242 Six Forks Road, Suite 970Raleigh, NC 27609AGREEMENT AND CONSIDERATIONYour dental coverage is underwritten by Delta Dental of North Carolina, a North Carolinadental service corporation (hereinafter referred to as "Delta Dental"). Delta Dental will payBenefits for Covered Services as set forth in this Policy. This Policy is issued in exchange forand on the basis of the statements made on your application and payment of the firstpremium. It takes effect on the Effective Date shown on your Summary of Dental PlanBenefits. It will remain in force for such further periods for which it is renewed automaticallyupon payment of the required premium as set forth in your application for coverage. Allperiods will begin and end at 12:01 A.M., Standard Time, where you live.10-DAY RIGHT TO EXAMINE AND RETURN THIS POLICYPLEPlease read this Policy. If you are not satisfied, you may return the Policy within 10 days afteryou received it. Mail or deliver it to Delta Dental or to your agent. Any premium paid will berefunded. This Policy will then be void from its start. If you are eligible for Medicare by reasonof age and purchased this Policy directly from Delta Dental without using an agent, this returnperiod is extended to 30 days.MThis Policy is signed for the Underwriting Company, Delta Dental of North Carolina, as of itsEffective Date.SAPresident & CEODelta Dental of North CarolinaThis Policy Has Been Certified by the Health Insurance Marketplace as Meeting theEssential Coverage Requirements for Pediatric Dental Services as Part of the EssentialHealth Benefits in Accordance with the Affordable Care Act.THIS DENTAL POLICY IS CONDITIONALLY RENEWABLE REFER TO RENEWABILITYAND TERMINATION PROVISIONTHIS POLICY IS A PPO DENTAL PLANIMPORTANT CANCELLATION INFORMATION— PLEASE READ THE PROVISIONSENTITLED “CONDITIONALLY RENEWABLE-PREMIUM MAY CHANGE” AND“TERMINATION.”READ YOUR POLICY AND SUMMARY OF DENTAL PLAN BENEFITSCAREFULLYThis Policy is a legal contract between the Insured and Delta Dental of North D-INVD-EHB-POL
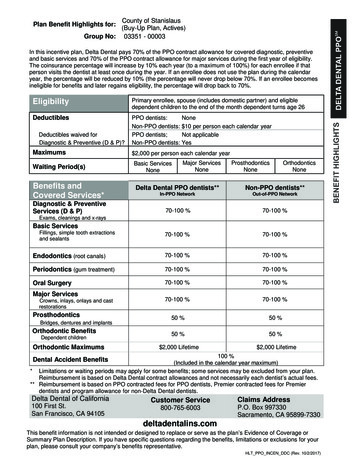
Delta Dental of North Carolina4242 Six Forks Road, Suite 970Raleigh, NC 27609Delta Dental PPO SM (Plus Delta Dental Premier Plan)Summary of Dental Plan BenefitsHigh Plan A EnhancedEThis Summary of Dental Plan Benefits should be read along with your Policy. Your Policy providesadditional information about your Delta Dental plan, including information about plan exceptions andreductions. If a statement in this Summary conflicts with a statement in the Policy, the statement in thisSummary applies to you and you should ignore the conflicting statement in the Policy. The percentagesbelow are applied to Delta Dental's allowance for each service and it may vary due to the Dentist's networkparticipation.*PLTHIS DOCUMENT IS INTENDED TO SERVE AS AN EXAMPLE AND IS NOT AN ACTUAL POLICY. UPONCOMPLETION OF YOUR ENROLLMENT YOU WILL RECEIVE AN ACTUAL COPY OF YOUR POLICYSAMCovered Services provided under your Policy are divided into two general categories: Non-EHB CoveredServices and EHB Covered Services. EHB Covered Services are Essential Health Benefits, as that term isdefined by the Patient Protection and Affordable Care Act (“PPACA”), and are available for individuals age18 and under. EHB Covered Services are subject to specific Out-of-Pocket Maximums, Maximum Payments,Deductibles and frequency limitations. You will find these Out-of-Pocket Maximums, Maximum Payments,Deductibles and frequency limitations, as well as a listing of all specific procedures that will be administeredas EHB Covered Services, at the end of this Summary under the heading “EHB Covered Services”. Pleasenote, in no event will the general frequency limitations found in your Policy apply to any of the EHB CoveredServices listed in this Summary of Dental Plan Benefits. The remaining general exceptions and reductionsfound in your Policy shall only apply to EHB Covered Services to the extent those general exceptions andreductions do not conflict with the specific Out-of-Pocket Maximums, Maximum Payments, Deductibles, andfrequency limitations found in this Summary of Dental Plan Benefits. An individual will be considered age 18and under until the end of the Benefit Year/policy year in which the individual attains the age of 19.As noted above, your Policy also covers Non-EHB Covered Services. Non-EHB Covered Services areavailable for eligible individuals regardless of age. For individuals 19 years of age or older, all procedurescovered under your Policy are considered Non-EHB Covered Services. For individuals age 18 and under,Non-EHB Covered Services includes only those procedures that are covered under your Policy which arenot specifically listed as EHB Covered Services at the end of this Summary. Non-EHB Covered Services aresubject to specific Out-of-Pocket Maximums, Maximum Payments, Deductibles, Waiting Periods andfrequency limitations. You will find these Out-of-Pocket Maximums, Maximum Payments, Deductibles,Waiting Periods and frequency limitations immediately following this paragraph under the heading “NonEHB Covered VD-HIGH-PLANAENH-SUM-5100i
Non-EHB Covered ServicesOut-ofNetworkDentistIn-Network DentistInclude all Covered Services that are notEssential Health Benefits (EHB) as definedby the Patient Protection and AffordableCare Act.Delta DentalPPO DentistDelta entistSAMPLEPlan PaysPlan PaysPlan Pays*Diagnostic & PreventiveDiagnostic and Preventive Services –100%90%90%NONEexams, cleanings, fluoride, and spacemaintainersBrush Biopsy – to detect oral cancer100%90%90%NONEEmergency Palliative Treatment – to100%100%100%NONEtemporarily relieve painRadiographs – X-rays100%90%90%NONESealants – to prevent decay of permanent100%90%90%NONEteethBasic ServicesMinor Restorative Services – fillings and80%70%70%6 monthscrown repairOral Surgery Services – extractions and80%70%70%6 monthsdental surgeryEndodontic Services – root canals80%70%70%6 monthsPeriodontic Services – to treat gum80%70%70%6 monthsdiseaseRelines and Repairs – prosthetic80%70%70%6 monthsappliancesOther Basic Services – misc. services80%70%70%6 monthsMajor ServicesMajor Restorative Services – crowns50%40%40%12 monthsProsthodontic Services – bridges,50%40%40%12 monthsdentures and crowns over implantsMaximum Payments and DeductiblesBenefit Year Maximum Payment 1,000 per personDeductible (per Benefit Year) 50 per person 150 per family*When you receive services from a Nonparticipating Dentist, the percentages in this column indicate theportion of Delta Dental’s Nonparticipating Dentist Fee that will be paid for those services. This amount maybe less than what the Dentist charges and you are responsible for that difference. Oral exams (including evaluations by a specialist) are payable twice per calendar/Benefit Year.Prophylaxes (cleanings) are payable twice per calendar/Benefit Year.People with specific at-risk health conditions may be eligible for additional prophylaxes (cleanings)or fluoride treatment. The patient should talk with his or her Dentist about treatment.Fluoride treatments are payable twice per calendar/Benefit year for people up to age 19.Bitewing X-rays are payable once per calendar/Benefit year and full mouth X-rays (which includebitewing X-rays) are payable once in any five year period.Porcelain crowns are optional treatment on posterior teeth. Implants and implant related services are payable once per tooth in any five-year period.Having Delta Dental coverage makes it easy for you to get dental care almost everywhere in the world! Youcan now receive expert dental care when you are outside of the United States through our Passport Dentalprogram. This program gives you access to a worldwide network of dentists and dental clinics. Englishspeaking operators are available around the clock to answer questions and help you schedule care. LANAENH-SUM-5100ii
more information, check our Web site or contact your benefits representative to get a copy of our PassportDental information sheet.Maximum Payments for Non-EHB Covered Services – 1000 per person total per Calendar Year on allservices.Out-of-Pocket Maximum Payment for Non-EHB Covered Services – An Out-of-Pocket Maximum is themaximum amount that you or your Eligible Dependent will pay for Covered Services throughout a BenefitYear. There is no Annual Out-of-Pocket Maximum Payment for Non-EHB Covered Services. You will beresponsible for all Coinsurance, Copayments, Deductibles and other out-of-pocket expenses associated withall Non-EHB Covered Services provided to you or your Eligible Dependent throughout the Benefit Year.Deductible for Non-EHB Covered Services – The Deductible per individual per Benefit Year is 50, limitedto a maximum of 150 per family per Benefit Year.Waiting Period for Non-EHB Covered Services– Individuals will be eligible for coverage for Diagnostic andPreventive, Basic, and Major Services in accordance with the applicable Waiting Periods set forth in theCovered Services chart above, measured from your or their date of coverage under this Policy.EEligible Dependents enrolled after your date of enrollment will have their own waiting period in accordancewith the above.PLEligibility - You and your Eligible Dependents, including your Domestic Partner are also eligible forcoverage under this Policy.A Domestic Partner is defined as follows and shall be treated as a “legal spouse” under the terms of thePolicy: M each party is the sole Domestic Partner of the other;each party is at least 18 years of age or older and competent to enter into a contract in the state inwhich they reside;both parties currently share a common legal residence and have shared said residence for at least sixmonths prior to application for Domestic Partner coverage;neither party is married to anyone other than the other or related to the other by adoption or bloodto a degree of closeness that would otherwise bar marriage in the state in which they legally reside;both parties are in a relationship of mutual support, caring, and commitment and intend to remain insuch a relationship in the indefinite future;both parties are jointly responsible for basic living expenses (basic living expenses are defined as thecost of basic food, shelter, and any other expenses of the common household-the partners need notcontribute equally or jointly to the payment of these expenses as long as they agree that both areresponsible for them); andneither party filed a Termination of Domestic Partnership within the preceding nine months.SA You and your Eligible Dependents must enroll for a minimum of 12 months. If Coverage is terminated priorto completing 12 months, you may not re-enroll for at least 12 months from the date of termination.If you and your Legal Spouse are both eligible for coverage under this Plan, you may be enrolled togetheron one application or separately on individual applications, but not both. Your Children may only be enrolledon one application.Payment of ClaimsWhile your Policy may pay the same percentage of Benefits for certain procedures regardless of whetheryou use a Delta Dental PPO Dentist or a Delta Dental Premier Dentist, your costs will generally be lowerwhen you use a Delta Dental PPO Dentist. Delta Dental PPO Dentists and Delta Dental Premier Dentistshave agreed to accept the pre-negotiated fee as payment in full. This limits your cost to the percentage ofCoinsurance listed, along with any applicable deductible. A Nonparticipating Dentist has not agreed toaccept the pre-negotiated fee as payment in full, and payment is based on an average of the rate GH-PLANAENH-SUM-5100iii
by Dentists for that procedure in the area. If your Nonparticipating Dentist charges a rate higher than thisaverage, you may be required to pay more than the percentage listed.Emergency services that are not reasonably available from a Delta Dental Participating Dentist without anunreasonable delay will be treated as if they had been provided by a Delta Dental PPO Dentist.For example, if a claim is submitted for several diagnostic and preventative services, along with radiographs,totaling 1,000:(For demonstration purposes only—Costs will vary based on your situation)Out-of-NetworkServiceIn-Network ServiceDelta Dental PPODentistsDelta Dental PremierDentistsOther Dentists 1,000 1,000 1,000Pre-Negotiated Fee 750 800N/AAllowed Amount 750 800 850Charges higher thanthe Allowed Amountthat are yourresponsibility 0 0Percentage listed inthe Plan Pays column100%Amount Paid byDelta Dental100% x 750 750100% x 800 800100% x 850 850Percentage listed inYou Pay column0%0%0%Dollar amount, basedon the percentagelisted in the You Paycolumn, which is Yourresponsibility0% x 750 00% x 800 00% x 850 0 0 0 0 0 00 0 150 00 150N/A 150 - 0 150N/APLECharges Submittedby the DentistSAM100% 150100%Your Total Cost:(The cost over theAllowed AmountPLUS the dollaramount based on thepercentage in theYou Pay Column)Savings for using aPremier Dentistinstead of a -INVD-HIGH-PLANAENH-SUM-5100iv
Savings for using aDelta Dental PPODentist instead of aNon-PPO Dentist: 150 - 0 150N/AN/ANOTICE: Your actual expenses for Covered Services may exceed the stated Coinsurance percentagebecause actual provider charges may not be used to determine Delta Dental’s and your paymentobligations.In-Network DentistEHB Covered Services(for individuals age 18 and under)Delta DentalPremierDentistPlan PaysDelta DentalPPO Plan Pays*SAMPLEPlan PaysDiagnostic & PreventiveDiagnostic and Preventive Services – exams,100%100%100%cleanings, fluoride, and space maintainersEmergency Palliative Treatment – to temporarily100%100%100%relieve painRadiographs – X-rays100%100%100%Sealants – to prevent decay of permanent teeth100%100%100%Basic ServicesMinor Restorative Services – fillings and crown80%60%60%repairOral Surgery Services – extractions and dental80%60%60%surgeryEndodontic Services – root canals80%60%60%Periodontic Services – to treat gum disease80%60%60%Relines and Repairs – prosthetic appliances80%60%60%Other Basic Services – misc. services80%60%60%Major ServicesMajor Restorative Services – crowns50%50%50%Prosthodontic Services – bridges, dentures and50%50%50%crowns over implantsOrthodontic ServicesOrthodontic Services –medically necessary only50%50%50%* When you receive services from a Nonparticipating Dentist, the percentages in this column indicate theportion of Delta Dental’s Nonparticipating Dentist Fee that will be paid for those services. This amount maybe less than what the Dentist charges and you are responsible for that difference.In-Network Annual Out-of-Pocket Maximum for EHB Covered Services – An Out-of-Pocket Maximum isthe maximum amount that you or an Eligible Person will pay for EHB Covered Services throughout a BenefitYear.The In-Network Annual Out-of-Pocket Maximum for EHB Covered Services shall be 350 per Benefit Year ifthis Policy covers one Eligible Person age 18 and under, or 700 per Benefit Year if this Policy covers two ormore Eligible Persons age 18 and under.Any Coinsurance, Copayments , Deductibles or other out-of-pocket expenses paid by an Eligible Person forIn-Network EHB Covered Services shall count toward that In-Network Annual Out-of-Pocket Maximum. TheIn-Network Annual Out-of-Pocket Maximum will not include any amounts paid for the following: (i)premiums; (ii) non-covered services; (iii) Out-of-Network Dentists; (iv) Coinsurance, Copayments,Deductibles , or other out-of-pocket expenses for services other than EHB Covered Services; or (v)Coinsurance, Copayments, Deductibles, or other out-of-pocket expenses for EHB Covered Servicesprovided to individuals 19 years of age and older. Once your applicable In-Network NVD-HIGH-PLANAENH-SUM-5100v
Maximum is reached for the Benefit Year, all In-Network EHB Covered Services provided Eligible Personswill be covered at 100% of the Maximum Approved Fee.Out-of-Network Out-of-Pocket Maximum for EHB Covered Services –There is no annual Out-of-PocketMaximum for Out-of-Network EHB Covered Services. Eligible Persons will be responsible for all Coinsurance,Copayments, Deductibles, and other out-of-pocket expenses associated with all Out-of-Network EHBCovered Services provided to Eligible Persons throughout the Benefit Year.Annual and Lifetime Maximum Payments for EHB Covered Services–There are no annual or lifetimeMaximum Payments. For EHB Covered Services under this Policy.Deductible for EHB Covered Services –The Deductible is 50 per individual per Benefit Year, limited to amaximum Deductible of 150 for all individuals under the age of 19 covered by this Policy per Benefit Year.The Deductible does not apply to Diagnostic and Preventive services, Emergency Palliative Treatment, Xrays, Sealants, and Orthodontics.Waiting Period for EHB Covered Services – There are no waiting periods for individuals age 18 and underseeking EHB Covered Services.EHB Covered ServicesEThe following services are the specific EHB Covered Services under this Policy to the extent they arereceived by an individual age 18 and under:SAMPLClass ADiagnostic and Preventive ServicesExaminations/EvaluationsD0120 – periodic oral evaluationD0140 – limited oral evaluation – problem focusedD0145 – oral evaluation for a patient age 2 and underD0150 – comprehensive oral evaluationD0160 – detailed and extensive oral evaluation (problem focused)D0180 –comprehensive periodontal evaluation Benefits for the foregoing clinical oral evaluations are payable twice in any BenefitYear, whether provided under one or more Delta Dental plan(s).Cleanings (Prophylaxes)D1110 – prophylaxis – adultD1120 – prophylaxis – child Benefits for prophylaxis including periodontal maintenance or scaling in the prescne ofmoderate or severe gingival inflammation are payable twice in any Benefit Year.Benefits for full mouth debridement are payable once in a lifetime.Fluoride TreatmentD1206 – topical fluoride varnishD1208 – topical application of fluoride (prophylaxis not included) Benefits for topical application of fluoride are payable twice in any Benefit Year.Space maintainersD1510 – space maintainer – fixed – unilateralD1516 – space maintainer – fixed – bilateral, maxillaryD1517 – space maintainer – fixed – bilateral, mandibularD1520 – space maintainer – removable – unilateralD1526 – space maintainer – removable – bilateral, maxillaryD1527 – space maintainer – removable – bilateral, mandibularD1550 – re-cementation of space maintainerD1575 – distal shoe – fixed, unilateral, up to age NAENH-SUM-5100vi
Emergency Palliative TreatmentD9110 – palliative (emergency) treatmentERadiographs (X-rays)D0210 – intraoral-complete series (including bitewings)D0330 – panoramic film Benefits for a complete intraoral radiographic series (including bitewing radiographs)or a panoramic film (with/or without bitewing films) are payable once in any five-yearperiod.D0220 – intraoral-periapical first filmD0230 – intraoral-periapical each addl filmD0240 – intraoral-occlusal filmD0270 – bitewing – single filmD0272 – bitewings – two filmsD0273 – bitewings – three filmsD0274 – bitewings – four filmsD0277 – bitewing, vertical, 7 to 8 films Benefits for bitewing images (posterior or vertical) are payable twice in any BenefitYear.SAClass BBasic ServicesMPLSealantsD1351 – Sealant – per tooth – unrestored permanent molars Sealants are payable only for the occlusal (biting) surface of unrestored permanentmolars, free from decay and restorations. Sealants are a Benefit payable once in any three-year period per tooth.D1352 – Preventive resin restorations in a moderate to high caries risk patient – permanenttooth Payable one sealant per tooth in any three-year period.D1353- sealant repair-per toothMinor Restorative Services (local anesthesia is considered to be part of restorative procedures)D2140 – amalgam – one surface, primary or permanentD2150 – amalgam – two surfaces, primary or permanentD2160 – amalgam – three surfaces, primary or permanentD2161 – amalgam – four or more surfaces, primary or permanentD2330 – resin-based composite – one surface, anteriorD2331 – resin-based composite – two surfaces, anteriorD2332 – resin-based composite – three surfaces, anteriorD2335 – resin-based composite – four or more surfaces (anterior) Tooth preparations, acid etching, adhesives (including resin bonding agents), linersand bases and curing are included as part of the restoration.D2910 – recement inlay, only or partial coverage restoration D2915 – recement cast orprefabricated post and coreD2920 – recement crownD2980 – crown repairD2981 – inlay repairD2982 – onlay repairD2983 – veneer repairD2990 – resin infiltration/smooth GH-PLANAENH-SUM-5100vii
Limited to 1 in any 36 month periodD2929 – prefabricated porcelain crown – primary toothD2930 – prefabricated stainless steel crown – primary toothD2931 – prefabricated stainless steel and porcelain crown – permanent tooth Stainless steel crowns are payable once per tooth in any five-year period. Benefits for stainless steel crowns with esthetic facings, veneers or coatings are optionaltreatment. Delta Dental will only pay the amount that it would pay for a conventionalstainless steel crown.D2940 – sedative fillingD2951 – pin retention – per tooth, in addition to restorationSAMPLEOral Surgery ServicesD7111 – extraction, coronal remnants – primary toothD7140 – extraction, erupted tooth or exposed rootD7210 –removal of erupted D7220 – removal of impacted tooth – soft tissueD7230 – removal of impacted tooth – partial bonyD7240 – removal of impacted tooth – completely bonyD7241 – removal of impacted tooth – completely bony, with unusual surgical complicationsD7250 –removal of residual tooth rootsD7251 – coronectomy – intentional partial tooth removalD7270 – tooth reimplantation and/or stabilization of accidentally evulsed or displaced toothD7280 – exposure of an unerupted toothD7282 – mobilization of erupted or malpositioned tooth to aid eruptionD7283 – placement of device to facilitate eruption of impacted toothD7310 – alveoloplasty in conjunction with extractions – four or more teeth per quadrantD7311 – alveoloplasty in conjunction with extractions – one to three teeth or tooth spaces, perquadrantD7320 – alveoloplasty not in conjunction with extractions – four or more teeth per quadrantD7321 – alveoloplasty, not in conjunction with extractions – one to three teeth or toothspaces, per quadrantD7471 – removal of exostosisD7510 – incision and drainage of abscess – intraoral soft tissueD7910 – suture of recent small wounds up to 5 cmD7953 – bone replacement graft for ridge preservation – per siteD7971 – excision of pericoronal gingivaEndodontic ServicesD3220 – therapeutic pulpotomy (excluding final restoration)D3221 – pulpal debridement, primary or permanent teethD3222 – Partial Pulpotomy for Apexogenesis – permanent tooth with incomplete rootdevelopment*** If a root canal is within 45 days of the pulpotomy, the pulpotomy is not a CoveredService as it is considered a part of the root canal procedure and Benefits are not payableseparately.D3230 – pulpal therapy (resorbable filling) – anterior, primary tooth (excluding finalrestoration)D3240 – pulpal therapy (resorbable filling) – posterior, primary tooth (excluding finalrestoration) Benefit for root canal fillings on primary teeth are limited to primary teeth withoutsuccedaneous (replacement) H-PLANAENH-SUM-5100viii
D3310 – anterior (excluding final restoration)D3320 – premolar (excluding final restoration)D3330 – molar tooth(excluding final restoration)D3346 – retreatment of previous root canal therapy – anteriorD3347 – retreatment of previous root canal therapy – premolarD3348 – retreatment of previous root canal therapy – molarD3351 – apexification/recalcification – initial visit (apical closure/calcific repair or perforations,root resorptions)D3352 – apexification/recalcification – interim visit D3353 – apexification/recalcification –final visit D3355 – Pulpal regeneration – initial visitD3410 – apicoectomy surgery – anteriorD3421 – apicoectomy surgery – premolar (first root)D3425 – apicoectomy surgery – molar (first root)D3426 – apicoectomy surgery – (each addl root)D3430 – retrograde filling– per rootD3450 – root amputation – per rootD3920 – hemisection (including any root removal)MPLEPeriodontic ServicesD4210 – gingivectomy or gingivoplasty – four or more teethD4211 – gingivectomy or gingivoplasty – one to three teethD4212 – gingivectomy or gingivoplasty – to allow access for restorative proceduresD4240 – gingival flap procedure, including root planing – four or more teethD4241 – gingival flap procedure, including root planing – one to three contiguous teeth orbounded teeth or bounded teeth spacesD4260 – osseous surgery (including flap entry and closure) – four or more contiguous teethor bounded teeth spaces per quadrantD4261 – osseous surgery (including flap entry and closure) – one to three contiguous teeth orbounded teeth spaces per quadrantD4263 – bone replacement graft – retained natural tooth first site in quadrantSAD4249 – clinical crown lengthening – hard tissueD4270 – pedicle soft tissue graft procedureD4273 – autogenous connective tissue graft procedures (including donor site surgery)D4275 – soft tissue allograftD4277 – free soft tissue graft procedure (including donor site surgery), first tooth oredentulous tooth positionD4278 – free soft tissue graft procedure (including donor site surgery), each contiguoustooth, implant or edentulous tooth positionD4283 – autogenous connective tissue graft procedure (including donor site surgery) – eachadditional contiguous tooth, implant, or edentulous tooth positionD4341 – periodontal scaling and root planing, four or more teethD4342 – periodontal scaling and root planing, one to three teeth, Benefits for the foregoing scaling and root planing are payable once, per quadrant, inany two-year period.D4346 – scaling in presence of moderate or severe gingival inflammation Benefits for prophylaxis including periodontal maintenance or scaling in the presenceof moderate or severe gingival inflammation are payable twice in any Benefit Year.Benefits for full mouth debridement are payable once in a lifetime.D4355 – full mouth debridement Full mouth debridement is payable once per lifetime.D4910 – periodontal maintenance procedures Benefits for periodontal maintenance following therapy, including adult prophylaxisare payable four times in any Benefit -PLANAENH-SUM-5100ix
D7921 – collect-apply autologous product Limited to 1 in any 36 month periodSAMPLERelines and RepairsD5410 – adjust complete denture – maxillaryD5411 – adjust complete denture – mandibularD5421 – adjust partial denture – maxillaryD5422 – adjust partial denture – mandibularD5511 – repair broken complete denture base, mandibularD5512 – repair broken complete denture base, maxillaryD5520 – replace missing or broken teeth – complete dentureD5611 – repair resin denture base, mandibularD5612 – repair resin denture base, maxillaryD5621 – repair cast partial framework, mandibularD5622 – repair cast partial framework, maxillaryD5630 – repair or replace broken clasp, per toothD5640 – replace broken teeth – per toothD5650 – add tooth to existing partial dentureD5660 – add clasp to existing partial denture, per toothD5670 – replace all teeth and acrylic on cast metal framework (maxillary)D5671 – replace all teeth and acrylic on cast metal framework (mandibular)D5710 – rebase complete maxillary dentureD5711 – rebase complete mandibular dentureD5720 – rebase maxillary partial dentureD5721 – rebase mandibular partial dentureD5730 – reline complete maxillary dentureD5731 – reline complete mandibular dentureD5740 – reline maxillary partial dentureD5741 – reline mandibular partial dentureD5750 – reline complete maxillary denture (laboratory)D5751 – reline complete mandibular denture (laboratory)D5760 – reline maxillary partial denture (laboratory)D5761 – reline mandibular partial denture (laboratory) Benefits for the foregoing rebase and reline of a complete or partial denture base arepayable once in any three-year period per appliance, six months after the initialinstallationD5850 – tissue conditioning denture (maxillary)D5851 – tissue conditioning denture (mandibular)D6930 – recement fixed partial dentureD6980 – fixed partial denture repair by reportOther Basic ServicesD0340 – 2D cephalometric imagesD0350 – Oral/facial photographic imagesD0391 – interpretation of diagnostic imageD0470 – diagnostic castsD9222 – deep sedation/general anesthesia – first 15 minD9223 – deep sedation/general anesthesia – each subsequent 15 minD9239 – intravenous consciousD9243 – intravenous conscious sedation/analgesia – each subsequent 15 minD9310 – consultationD9610 – therapeutic drug injection, single administrationD9612 – therapeutic drug injection, two or more administrations, different medicationsD9613 – infiltration of sustained release therapeutic drug – single or multiple sitesD9930 – treatment of complications -INVD-HIGH-PLANAENH-SUM-5100x
D9944 – occlusal guard – hard appliance full arch, by reportD9946 – occlusal guard – hard appliance partial arch, by reportBenefits for an occlusal guard are payable once per Benefit Year for individuals 13-18 years of age.Class CMajor ServicesSAMPLEMajor Restorative ServicesD2510 inlay – metallic – one surfac
Delta Dental of North Carolina . QINVD-200-Delta-2020-HIGH 2020-NC-DD-INVD-HIGH-PLANAENH-SUM-5100 . i . Delta Dental of North Carolina . 4242 Six Forks Road, Suite 970 . Raleigh, NC 27609 . Delta Dental PPOSM (Plus Delta Dental Premier Plan) Summary of Dental Plan Benefits .