Transcription
3/18/2015Optimal ArthritisManagement: BridgingClinic to the CommunityMary Altpeter, MSW, PhDJulie Keysor, PT, PhDLori Schrodt, PT, PhDAmerican Physical Therapy Association Combined Sections MeetingFebruary 6, 2015APTA CSM 2015Disclosures Julie Keysor—None Mary Altpeter—None Lori Schrodt‐‐NoneAPTA CSM 20151
3/18/2015Objectives Discuss evidence‐based aerobic, strength training, andself‐management strategies for arthritis Describe the application of motivation and behaviorchange theories to arthritis self‐management andphysical activity recommendation adherence. Discuss opportunities in the community that canpromote use of evidence‐based strategies. Discuss integration models of physical therapypractice and community programsAPTA CSM 2015Presentations1) Epidemiology and Clinical Management2) Motivation and Behavior Change3) Community Resources: Evidence‐ BasedHealth Promotion ProgramsAPTA CSM 20152
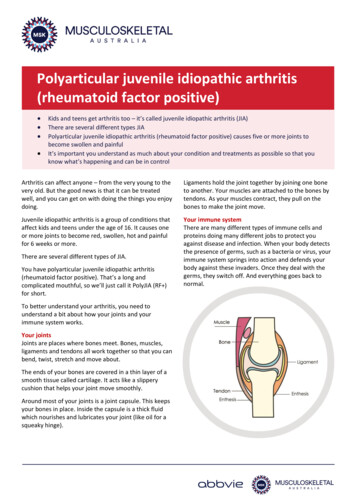
3/18/2015Epidemiology andClinical ManagementJulie Keysor, PT, PhDAmerican Physical Therapy Association Combined Sections MeetingFebruary 6, 2015APTA CSM 2015Boston UniversityWhat is Arthritis?The term arthritis is used todescribe more than 100rheumatic diseases andconditions that affect joints,the tissues which surroundthe joint and otherconnective tissuePain, activity limitation, andparticipation restriction arecommonAPTA CSM 20153
3/18/2015Types of Arthritis or Rheumatic ConditionsMost Common Conditions Osteoarthritis Rheumatoid Arthritis Fibromyalgia Lupus GoutOthers Psoriatic arthritis Ankylosing spondylitis Juvenile arthritis MyositisAPTA CSM 2015Arthritis the Leading Cause of Disability in the USStrokeBlindness or vision problemsDeformity or limbDeafnessDiabetesLung or respiratory problemMental or emotional problemsHeart troubleBack or spine problemsArthritis0246810Hootman JM, Brault MW, Helmick CG, Theis KA, Armour BS. MMWR 2009;58(16):421‐426.APTA CSM 20154
3/18/2015Boston University52,000,000 million people doctor‐diagnosed arthritisAll ages; both genders; all ethnicitiesAPTA CSM 2015Arthritis in theUS: A Snapshot750,000HospitalizationsHootman et al. MMWR2006;55(40):1089–1092; Bolin etal. MMWR 2005; 54(5): 119‐1238.3 Million (31%)Limited in Work22.7 million (42.4%)Limited in activities78 millionAmbulatory Care Visits (5% total visits)52,000,000 Million PeopleSelf‐reported, Doctor‐diagnosedAdapted from Theresa Brady, Centers of Disease Control and PreventionAPTA CSM 20155
3/18/2015A Growing Problem: Increasing Prevalence70,000MenWomen60,00050,00063 Million56 Million 59 Million48 Million 52 25Hootman JM, Helmick CG. Arthritis Rheum 2006;54(1):226–229.APTA CSM 201512Percent of persons age 18‐64 reportingarthritis/rheumatism as the main cause of activitylimitation (not including chronic back pain)10089.97551.15053.925.72532.90Difficulty with Walking three Climbing a flightcity blocksof stairsany of the 4activitiesGraspingobjectsLifting/carrying10 lbsAdapted from K Theis, Centers of Disease Control and PreventionHootman et al. Arthritis Rheum 2004;50(9, suppl):5641APTA CSM 20156
3/18/201544% older adults with arthritis are inactive vs. 36% olderadults without arthritis13% of older adults witharthritis do resistiveexerciseShih et al., Am J Prev Med 2006;30(5):385‐93APTA CSM 2015Summary Arthritis is the most prevalent chronic painfulmusculoskeletal condition among adults Arthritis is the leading cause of disability among olderadults Arthritis is a chronic, often progressive, condition thatresults in pain, activity limitations, and participationrestrictions Affects all ages, both genders, and all ethnicitiesAPTA CSM 20157
3/18/2015Arthritis State of the Science Meeting April 7, 2014Arthritis, Your Patients,Your PracticeArthritis: A common primary orsecondary condition among yourpatientsAPTA CSM 2015Scenario 1: You received a referral for Mrs. Sfrom her primary care physician for kneerange of motion and strengthening with a dxof arthritisScenario 2: Mrs. S sought physical therapycare form you after a recommendation fromher primary care physician who told her shelikely had a little arthritis.APTA CSM 20158
3/18/2015Mrs. S Does she have knee OA? 75 years old Female Knee pain constant; worse in the morning; some pain withactivity Stiffness 1‐2 hours in the morning Noticeable joint warmth and swelling Stiffness less than 30 minutes CrepitusAPTA CSM 2015Mrs. S has an inflamed knee, metacarpalswelling, and wrist swelling Do you treat? Flare: treat inflammation active ROM and isometric strengthening protect loading of joint during flare maybe ice Questions: Is she getting any treatment for her joint inflammation? Has she seen a rhuematologist or primary care physician for this? How long has she had joint swelling? What is she doing for the joint inflammation? Referral: Referral to rheumatologist for inflammatory disease managementAPTA CSM 20159
3/18/2015Mrs. S now has inflammation under controland is referred from rheumatologist to PT Patient reports pain with exercise and difficulty walking in thecommunity, doing household activities, and caring forgrandchildren Evaluation: Mild pain with walking, strength 4 /5 quad, hip abductors, and gluts;timed up and go test 12 seconds; gait shows asymmetrical step lengthand wide base of support What are your treatment goals? Goals: Strength 5/5 t/o lower extremity; decrease timed up and go;adhere to an exercise program during flare; engage in 150 minutes ofmoderate activity weekly and resistance training 2x/weekAPTA CSM 2015Mrs. C (with knee OA) Do you treat? Yes Evaluation: Mild pain with walking, strength 4 /5 quad, hip abductors, and gluts;timed up and go test 12 seconds; WOMAC score 30/68, asymmetric gait,wide base of support Assuming little impact of comorbidities, what are thetreatment goals? Goals: Strength 5/5 t/o lower extremity; decrease timed up and go test;adhere to an exercise program; engage in 150 minutes of moderateactivity weekly and resistance training 2x/weekAPTA CSM 201510
3/18/2015Treatment‐Get Moving Start low impact activity (5‐15 minutes) Progress activity: duration and intensity Posture and alignment are important! Monitor pain with activity Pain during or after activity MAY requiremodification of activity (May be okay ifpain is not long lasting)APTA CSM 2015Treatment: Aerobic Conditioning American College of SportsMedicine Guidelines forOlder Adults 30 to 60 minutes per session 50‐70% of heart rate reserve (HRR)Low impact activity Short bouts of 10 minutes okay, particularly initially MOVE!APTA CSM 201511
3/18/2015Treatment—Strength Training Progressive resistance training American College of Sports Medicine Recommendations forOlder Adults –60‐80% 1 RM, 8‐12 reps, 1‐3 sets, with 1‐3 min restbetween sets. – For endurance training, use lighter loads (50‐60%) withhigher reps (10‐15 or more) Need to achieve enough resistance to improve strength andneed to progress to optimal strength Neuromuscular training Closed chain sensorimotor learning and dynamic motorcontrol NEMEX‐TJR (Eva Ageberg, Anne Link, Ewa M Roos, 2010)APTA CSM 2015Boston UniversityOverall TreatmentConsiderations Posture and positioning Strengthen tissues withoutoverloading joint Pace activities (24‐7 approach) Respect joint pain Teach people how to modify activity if pain ispresentAPTA CSM 201512
3/18/2015Goals for People with Arthritis? Engage in gentle range of motion exercise,gentle pool activity; no strengthening Most people with arthritis (that ismedically controlled) can engage in somesort of strengthening and aerobic exercise(may need to accommodate)APTA CSM 2015What are these treatment approachesbased on?APTA CSM 201513
3/18/2015Systematic ReviewsOsteoarthritis and Rheumatoid teSmallGoodGoodGoodStrength Strengthtraining PainFunctionLevel of EvidenceOttowa Panel. Physical Therapy, 84: 2004 & 85: 2005; MOVE Consensus 2005;Jamtvedt et al. Physical Therapy 88:2008; Fransen M., McConnell S. TheCochrane Collaboration, 2009; Wang et al., Ann Inter Med 157: 2012APTA CSM 2015Knee Osteoarthritis Strongly recommended: (ACR 2012 PracticeGuidelines; EULAR 2013 Practice Guidelines;OARSI 2014 Practice Guidelines) Aerobic and/or aquatic exercise Resistance exercisesAPTA CSM 201514
3/18/2015Other approaches—limited evidence ofbenefit Knee bracing Orthotics Shoes Manual therapyAPTA CSM 2015Boston UniversityCaution: Red FlagsUncontrolled disease activityCurrent Severe PainPain non‐arthritis joints and tissuesBalance/ functional impairmentsPatient not responding to exerciseAPTA CSM 201515
3/18/2015RED FLAGS Connect with health care team andre‐evaluate approach Physical therapist Rheumatologist Pain management Orthopedist Rehabilitation medicine Gerontologist Occupational therapist Psychologist Social workerAPTA CSM 2015Boston UniversityYour patient is doing well with PT treatment.Strength increased and gait speed has improved.Will your patient maintain these improvementsafter discharge? Is she doing the right activities tooptimize her health?APTA CSM 201516
3/18/2015Boston UniversityA “Simple” Medical ModelHealth Care Provider: Exercise is goodfor you. You need to exercise.Patient: OkayThis does not happen because lifestyle andbehavior changes are difficult.APTA CSM 2015Boston UniversityChronic Disease Medical‐Behavior Model:More Complex Patient with Pain/FunctionalLimitationReturn to (prior) long History ofInactivityExercise in PastDiseaseComplexityAvoid Exercising or MovementFailed ExercisingBelieve that exercise is painful,can’t be done, & isn’t beneficialAPTA CSM 201517
3/18/2015Boston UniversityWe know exercise is good for people with arthritis.Being active with arthritis is not easy!Are we doingall we can?APTA CSM 2015Boston UniversityHave they acquired enough change inbehavior to be active after discharge?APTA CSM 201518
3/18/2015Acknowledgements:Saralynn AllaireMolly VaughanMary SlavinENACTHealth and Disability Research InstituteClinical Epidemiology Research andTraining UnitThe National NIDRR Arthritis Rehabilitation Research andTraining CenterNIDRR PR/Award #H133B100003APTA CSM 201512 miles north ofBoston 44 inchesof snow so far 12more inches on thewayAPTA CSM 201519
adults without arthritis 13% of older adults with arthritis do resistive exercise Shih et al., Am J Prev Med 2006;30(5):385‐93 APTA CSM 2015 Summary Arthritis is the most prevalent chronic painful musculoskeletal condition among adults Arthritis is the leading cause of disability among older adults