Transcription
Case Mix IndexANALYZING CASE MIX INDEX AND THE IMPACT ON CDI PROGRAMSwww.huronconsultinggroup.com/healthcare 1-866-229-8700
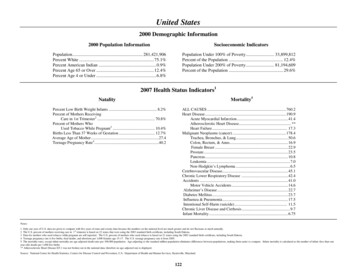
Case Mix IndexANALYZING CASE MIX INDEX AND THE IMPACT ON CDI PROGRAMSBy Gerri Birg, MSN, RN, CCDS, managing director, Huron HealthcareCase Mix Index (CMI) is the average relative weight for all cases reported in a Base MS-DRG. MS-DRGs at lower severitylevels have lower relative weights and MS-DRGs at higher severity levels have higher relative weights. Therefore, CMI isa barometer that summarizes a patient population and is a predictor of illness severity and expected reimbursement.CMI Sum of all DRG RWs divided by the number of cases/month/yearThe CMI value is used in determining theallocation of resources necessary to providecare for and/or treat the patients in anidentified group. The CMI of a facility reflectsthe diversity and clinical complexity of thepatients and the associated resources utilizedin the care of those patients.The Case Mix Index has historically been usedto calculate adjusted average cost per patient(or day) for a given hospital relative to theadjusted average cost for other hospitals bydividing the average cost per patient (or day)by the hospital’s calculated CMI. The adjustedaverage cost per patient would reflect theFactors Impacting CMI13Accuracy andspecificity ofdocumentationVolumes:24Service lines: Medical versus Transplantation High-weighted Cardiothoracicsurgicalof organsDRG’s such astracheostomies,major surgeries5Accuracyof codingAnnual updatesto the DRGrelative weightssurgeries Neurosurgeries6Coding guidelinechangescharges reported for the types of casestreated in that year. For example, if HospitalA has an average cost per patient of 1,000and a CMI of 0.80 for a given year, theiradjusted cost per patient is 1,000 / 0.80 1,250. Likewise, if Hospital B has an averagecost per patient of 1,500 and a CMI of 1.25,their adjusted cost per patient is 1,500 /1.25 1,200. Therefore, if a hospital hasa CMI greater than 1.00, their adjusted costper patient or per day will be lowered and,conversely, if a hospital has a CMI less than1.00, their adjusted cost will be higher.CMI of a facility“ Thereflects the diversity andclinical complexity of thepatients and the associatedresources utilized in the careof those patients.”Fran Jurcaksenior directorHuron HealthcareThese factors directly impact the ability toadopt CMI as a performance metric of a ClinicalDocumentation Improvement (CDI) program.While CMI has traditionally been a gut checkto measure CDI program success, annualchanges in relative weights over the past threeyears for the top medical DRGs have negativelyimpacted most of these DRGs, preventingaccurate comparison of CMI from year to year.Fluctuations in patient admissions and surgicalstaff/services also impact the ability to utilizethe CMI as an accurate measurement of CDIprogram influence on overall facility finances.A high volume of short stays can negativelyimpact CMI as these short stay cases are oftenreimbursed under the lowest relative weight.Source: Huron Healthcare2
CASE MIX INDEXANALYZING CMIIt is important to remove as many of the variables as possible when analyzing CMI. Thus,separating volumes of medical and surgical DRGs is necessary to create a base level ofmeasurement. Separating the high-weighted DRGs, such as tracheostomies and ventilators, andmonitoring the volumes of high-weighted surgical procedures will create a base from which tomeasure the impact from improved documentation.Example of Recommended Data Points for CMI Review and AnalysisTotal DischargesOverall CMIMedical DischargesMedical CMISurgical DischargesSurgical CMISept. 14Oct. 14Nov. 14Dec. 14Jan. 15Feb. Source: Huron Healthcare* Number of tracheostomies (DRGs 3, 4, & 11 – Surgical DRGs)**Number of ventilators (DRGs 207, 208 & 870 – Medical DRGs(Note: In this example, CDI staff was in training through month of September.)Analysis by MonthThis chart demonstrates how to separate the data to better track trends and issues that are measuredby the CMI, including the potential impact of a CDI program on the quality of documentation.MedicalSept ‘14Oct ‘14Nov ‘14SurgicalAverage number of surgeries with slightlyhigher than average surgical relative weightsCDI program needs to refocus efforts on medical dischargesIncreased CMI with lower thanaverage number of dischargesMuch higher than average surgicaldischarges with lower than averagerelative weightsSpecificity of documentation resulted in increased capture of medical CMILower than average number ofdischarges with significant increasein medical CMISurgical volumes slightly above averagewith higher relative weightsTrachs/vents likely impacted overall CMIHigher than average number of trachsHigher than average number of ventsDec ‘14Jan ‘15Analysis/CommentsAverage number of medicaldischarges with lower than averagemedical relative weightsHigh acuity of surgical casesVolume of surgeries, while lower-weighted, still impacted the overall CMIHigher acuity of patient population reflected in CMICDI program likely significant impact to overall CMIHigher than average medicaldischarges with below average CMILower than average surgical dischargeswith average CMIHoliday month, review for shorter LOS (typically means lower relative weights for medical and surgical)Higher than average medicaldischarges with higher CMIAverage surgical discharges with averagerelative weightsHigher acuity of medical discharges, could be impacted by increased ventsLower than average surgical dischargesHigher acuity of patient population reflected through higher relative weights for medical and surgicalAbove average CMIWould review CDI program metrics for validation of CMIReview CDI staffing and metrics of coverageHigher than average vents couldimpact Medical CMIFeb ‘15Lower than average medicaldischargesHigher than average ventsHighest medical CMISource: Huron Healthcarewww.huronconsultinggroup.com/healthcare 1-866-229-87003
CASE MIX INDEXThis analysis demonstrates that changes inCase Mix Index are often multifactorial andrequire a further deep dive into key data tounderstand the impact of documentationimprovement programs. The importanceof accurate, complete, and consistentdocumentation is imperative to ensure anaccurate CMI. Yet, it is also important toreview for other influences that can positivelyand negatively impact the CMI regardless ofthe quality of documentation. CMI in itself isnot an accurate measurement of CDI programsuccess but should be utilized in conjunctionwith other metrics to evaluate programgrowth and sustainability.OTHER METRICS TO CONSIDERCDI productivity metrics reflect the impactof CDI staff work in supporting accurateand compliant documentation that has thepotential to increase the relative weight ofthe final coded DRG. Metrics that should bemonitored include: review rates, query rates,physician response rates, and physicianacceptance rates. Achieving industrybenchmarks for these metrics should bereflected in an improved CMI.CDI PRODUCTIVITYMETRICSReview RatesQuery RatesPhysician Response RatesPhysician Acceptance RatesAdditionally, the average length of stay shouldalso be monitored in conjunction with the CMIto demonstrate that more acutely ill patientswith higher weighted DRGs are admitted for alonger period of time than those patients whoare less acutely ill. Monitoring medical versussurgical length of stay should also occur toalign the data with the types of patients andanticipated outcomes.TRENDING DATA OVER TIMEAdjustment to the relative weights of eachDRG occurs annually on October 1, makingit difficult to accurately monitor trends overtime. They are revised to accommodatechanges in operating and capital expensesin acute care hospitals to better reflectthe severity of illness and average costsassociated with monitoring and treatingmedical conditions. Comparing current CMI toa previous year’s CMI provides no informationregarding the direct impact of the CDIprogram. Many of the common medical DRGshave seen significant decline of their relativeweight over the past few years. This indicatesthat overall medical CMI will be decreasedlast year to this year regardless of volumes.As surgical volumes shift from the inpatientto the outpatient environment, overall surgicalCMI should increase simply due to theincreased relative weights of those surgicalDRGs that require inpatient status to perform.in itself is not an“ CMIaccurate measurementof CDI program successbut should be utilized inconjunction with othermetrics to evaluate programgrowth and sustainability.”Gerri Birgmanaging directorHuron HealthcareThe use of overall payer CMI as the solemeasurement of patient acuity or CDI programsuccess is shortsighted and inappropriate. It isimportant to take a deeper dive into the dataand separate medical and surgical volumes,average length of stay, and CMI.SUMMARYAlthough there are many factors thatcan influence a healthcare facility’s CaseMix Index, a well-established clinicaldocumentation improvement program isnecessary to ensure and provide accurate,consistent and compliant documentation toreflect an accurate CMI. It is also important toreview additional CDI metrics to optimize theimpact of the CDI program and make gooddecisions regarding budgets, staffing, andprogram expectations and growth. Leadingpractice workflows that drive accuratedocumentation and data integrity, anddashboards that provide validated metricssupport decisions that sustain successfulCDI programs.www.huronconsultinggroup.com/healthcare 1-866-229-87004
CASE MIX INDEXCONTACTTo find out more about analyzing Case Mix Index and the impact of CDI programs, please contact:Gerri Birg, MSN, RN, CCDS, managing Gerri Birg is the National Lead for Huron’s CDI solution practice. Over the last 12 years, she has led large-scaleCDI implementation efforts working with a variety of clients, including children’s hospitals, large academic medicalcenters, and multi-hospital systems. Her extensive background in healthcare operations management encompassesutilizing outcome data to coach, guide, and train staff in providing strategic direction, benchmarking opportunities, andappropriate outcome management techniques as it integrates into continuous quality improvement. 2016 Huron Consulting Group Inc. All Rights Reserved. June 16 #150751ABOUT HURON HEALTHCAREHuron Healthcare is the premier provider of performance improvement and clinical transformation solutions for hospitals and healthsystems. In 2015, Huron acquired Studer Group, the market leader in driving healthcare cultural transformation. The combination ofHuron and Studer Group is focused on improving healthcare providers’ clinical, operational, and financial outcomes. By partneringwith clients, Huron delivers solutions that improve quality, increase revenue, reduce expenses, and enhance physician, patient, andemployee satisfaction across the healthcare enterprise. Clients include leading national and regional integrated healthcare systems,academic medical centers, community hospitals, and physician practices. Modern Healthcare ranked Huron Healthcare third onits 2014 list of the largest healthcare management consulting firms. Learn more at www.huronconsultinggroup.com/healthcare orfollow us on Twitter: @Huron.To see how Huron Healthcare solutions can empower your mission, contact usat 1-866-229-8700 or visit Ginsburg, Paul B. and Grace M. Carter. “Medicare case-mix index increase.”Health Care Finance. Rev. 1986 Summer; 7(4): 51–65.Mendez, Carmen M., Darrell W. Harrington, Peter Christenson, and Brad Spellberg. “Impact of Hospital Variables on Case Mix Index as a Marker of Disease Severity.” Popul Health Managazine. 2014 February 1;17(1): 28–34. doi: 10.1089/pop.2013.0002.Murphey, Brian. “Case Mix Index: Use with Caution.” Association of Clinical Documentation Improvement Specialists. 2012 July.www.huronconsultinggroup.com/healthcare 1-866-229-87005
For example, if Hospital A has an average cost per patient of 1,000 and a CMI of 0.80 for a given year, their 1,250. Likewise, if Hospital B has an average their adjusted cost per patient is 1,500 / a CMI greater than 1.00, their adjusted cost per patient or per day will be lowered and, conversely, if a hospital has a CMI less than