Transcription
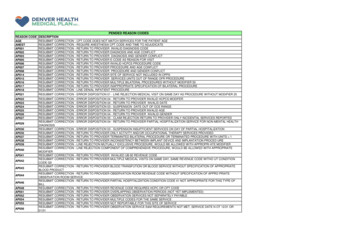
PENDED REASON CODESREASON 14AP015AP016AP017AP018DESCRIPTIONRESUBMIT CORRECTION - CPT CODE DOES NOT MATCH SERVICES FOR THE PATIENT AGERESUBMIT CORRECTION - REQUIRE ANESTHESIA CPT CODE AND TIME TO ADJUDICATERESUBMIT CORRECTION - RETURN TO PROVIDER INVALID DIAGNOSIS CODERESUBMIT CORRECTION - RETURN TO PROVIDER DIAGNOSIS AND AGE CONFLICTRESUBMIT CORRECTION - RETURN TO PROVIDER DIAGNOSIS AND GENDER CONFLICTRESUBMIT CORRECTION - RETURN TO PROVIDER E-CODE AS REASON FOR VISITRESUBMIT CORRECTION - RETURN TO PROVIDER INVALID HCPCS PROCEDURE CODERESUBMIT CORRECTION - RETURN TO PROVIDER PROCEDURE AND AGE CONFLICTRESUBMIT CORRECTION - RETURN TO PROVIDER PROCEDURE AND GENDER CONFLICTRESUBMIT CORRECTION - RETURN TO PROVIDER SITE OF SERVICE NOT INCLUDED IN OPPSRESUBMIT CORRECTION - RETURN TO PROVIDER SERVICES UNITS OUT OF RANGE OFR PROCEDURERESUBMIT CORRECTION - RETURN TO PROVIDER MULTIPLE BILATERAL PROCEDURES WITHOUT MODIFIER 50RESUBMIT CORRECTION - RETURN TO PROVIDER INAPPROPRIATE SPECIFICATION OF BILATERAL PROCEDURERESUBMIT CORRECTION - LINE DENIAL INPATIENT PROCEDUREAP021RESUBMIT CORRECTION - ERROR DISPOSITION 01 - LINE REJECTION MEDICAL VISIT ON SAME DAY AS PROCEDURE WITHOUT MODIFIER 25AP022AP023AP024AP025AP026AP027RESUBMIT CORRECTION - ERROR DISPOSITION 04 - RETURN TO PROVIDER INVALID HCPCS MODIFERRESUBMIT CORRECTION - ERROR DISPOSITION 04 - RETURN TO PROVIDER INVALID DATERESUBMIT CORRECTION - ERROR DISPOSITION 03 - SUSPENSION DATE OUT OF OCE RANGERESUBMIT CORRECTION - ERROR DISPOSITION 04 - RETURN TO PROVIDER INVALID AGERESUBMIT CORRECTION - ERROR DISPOSITION 04 - RETURN TO PROVIDER INVALID GENDERRESUBMIT CORRECTION - ERROR DISPOSITION 05 - CLAIM REJECTION RETURN TO PROVIDER ONLY INCIDENTAL SERVICES REPORTEDRESUBMIT CORRECTION - ERROR DISPOSITION 04 - RETURN TO PROVIDER PARTIAL HOSPITALIZATION SERVICE FOR NON-MENTAL HEALTHDIAGNOSISRESUBMIT CORRECTION - ERROR DISPOSITION 03 - SUSPENSION INSUFFICIENT SERVICES ON DAY OF PARTIAL HOSPITALIZATIONRESUBMIT CORRECTION - RETURN TO PROVIDER ONLY ACTIVITY AND/OR OCCUPATIONAL THERAPY SERVICES PROVIDEDRESUBMIT CORRECTION - RETURN TO PROVIDER TERMIANTED BILATERAL PROCEDURE OR TERMINATED PROCEDURE WITH UNITS 1RESUBMIT CORRECTION - RETURN TO PROVIDER INCONSISTENCY BETWEEN IMPLANT DEVICE AND IMPLANTATION PROCED URERESUBMIT CORRECTION - LINE REJECTION MUTUALLY EXCLUSIVE PROCEDURE, WOULD BE ALLOWED WITH APPROPRI ATE MODIFIERRESUBMIT CORRECTION - LINE REJECTION COMPONENT OF COMPREHENSIVE PROCEDURE, WOULD BE ALLOWED WITH APPROPRIATEMODIFIERRESUBMIT CORRECTION - RETURN TO PROVIDER INVALIED UB-92 REVENUE CODERESUBMIT CORRECTION - RETURN TO PROVIDER MULTIPLE MEDICAL VISITS ON SAME DAY, SAME REVENUE CODE WITHO UT CONDITIONCODE G0RESUBMIT CORRECTION - RETURN TO PROVIDER BLOOD TRANSFUTION OR BLOOD SERVICE WITHOUT SPECIFICATION OF APPROPRIATEBLOOD PRODUCTRESUBMIT CORRECTION - RETURN TO PROVIDER OBSERVATION ROOM REVENUE CODE WITHOUT SPECIFICATION OF APPRO PRIATEOBSERVATION ROOM SERVICERESUBMIT CORRECTION - RETURN TO PROVIDER PARTIAL HOSPITALIZATION CONDITION CODE 41 NOT APPROPRIATE FOR THIS TYPE OFBILLRESUBMIT CORRECTION - RETURN TO PROVIDER REVENUE CODE REQUIRES HCPC OR CPT CODERESUBMIT CORRECTION - RETURN TO PROVIDER OVERLAPPING OBSERVATION PERIODS (NOT YET IMPLEMENTED)RESUBMIT CORRECTION - RETURN TO PROVIDER OBSERVATION SERVICES NOT SEPARATELY PAYABLERESUBMIT CORRECTION - RETURN TO PROVIDER MULTIPLE CODES FOR THE SAME SERVICERESUBMIT CORRECTION - RETURN TO PROVIDER NOT REPORTABLE FOR THIS SITE OF SERVICERESUBMIT CORRECTION - RETURN TO PROVIDER OBSERVATION SERVICE E&M REQUIREMENTS NOT MET, SERVICE DATE N OT 12/31 42AP043AP044AP046AP048AP051AP052AP054AP055AP056
AP058RESUBMIT CORRECTION - RETURN TO PROVIDER G0379 ONLY ALLOWED WITH G0378AP059RESUBMIT CORRECTION - RETURN TO PROVIDER CLINICAL TRIAL REQUIRES DIAGNOSIS CODE V707 AS OTHER THAN PR IMARY P073BILLRESUBMIT CORRECTION - RETURN TO PROVIDER USER OF MODIFIER CA WITH MORE THAN ONE PROCEDURE NOT ALLOWEDRESUBMIT CORRECTION - RETURN TO PROVIDER CODE CAN ONLY BE BILLED TO THE DME REGIONAL CARRIERRESUBMIT CORRECTION - RETURN TO PROVIDER CODE NOT ALLOWED UNDER OPPS, ALTERNATE MAY BE AVAILABLERESUBMIT CORRECTION - RETURN TO PROVIDER OCCUPATION THERAPY CAN ONLY BE BILLED ON PARTIAL HOSPITALIZA TION CLAIMSRESUBMIT CORRECTION - ERROR DISPOSITION 01 - LINE REJECTION REVENUE CODE NOT RECONGNIZED BY MEDICARERESUBMIT CORRECTION - RETURN TO PROVIDER CA MODIFIER REQUIRES PATIENT STATUS 20RESUBMIT CORRECTION - RETURN TO PROVIDER CLAIM LACKS REQUIRED DEVICE CODERESUBMIT CORRECTION - RETURN TO PROVIDER SERVICE NOT BILLABLE TO FISCAL INTERMEDIARYRESUBMIT CORRECTION - RETURN TO PROVIDER INCORRECT BILLING OF BLOOD AND BLOOD PRODUCTRESUBMIT CORRECTION - REQUEST ITEMIZED BILL AND MEDICAL RECORDS FOR REVIEW TO PROPERLY ADJUDICATE THE CLAIMBPNPIResubmit Billing Provider NPIBTYPECPTCDRESUBMIT CORRECTION - THE BILLE TYPE DOES NOT MATCH BILLED SERVICESRESUBMIT CORRECTION - CPT CODE IS INVALID OR D54D58D59D64DHCAHLIncomplete claim form.Submit appropriate claim formRequires additional information.Requires anesthesia time.Resubmit claim with Medicare EOBResubmit with primary EOBPrimary Diagnosis RequiredIncorrect authorization number.Requires prior authorization.Please resubmit claim with ER report.Resubmit with OP report.Please resubmit claim with physician notes.Please resubmit claim with a copy of the consult report.Resubmit with dialysis reports.Itemized statement required.Need ambulance EMS report.Requires discharge summary.Resubmit to dental plan.RESUBMIT WITH CMS CAH RATE LETTER FOR REASONABLE COST REIMBURSEMENTDIAGNDOSGENDRHCPCRESUBMIT CORRECTION - ICD-9 DIAGNOSIS CODE MISSING OR INVALID FOR PT IN QUESTIONRESUBMIT CORRECTION - DATES OF SERVICE ON CLAIM APPEAR TO BE INCORRECTRESUBMIT CORRECTION - BILLED CPT CODE DOES NOT MATCH PATIENT'S SEXRESUBMIT CORRECTION - OUTDATED OR MISSING HCPC CODE CANNOT ADJUDICATEICDINDRESUBMIT CORRECT ICD INDICATORINPOSINVALINVBLINVMORESUBMIT CORRECTION - PLACE OF SERVICE DOES NOT MATCH BILL TYPERESUBMIT CORRECTION - INVALIED CPT OR REV CODE OR HCPC CODESRESUBMIT CORRECTION - BILLED SERVICES DO NOT MATCH SERVICES AUTHORIZEDRESUBMIT CORRECTION - INVALID MODIFIER FOR CPT CODE IN QUESTIONINVOIM0010M0014M0016M0018INVOICE REQUIREDNo Active Provider ContractNo Contract Term found for ServiceNo Benefit for ServiceInvalid Accommodation Days
M0025M0027M0028M0054M0072M0073M0074Claim Total MismatchPrimary ICD9 Diagnostic Code RequiredDischarge Status Required for Inpatient and SNF ClaimsManually Pended ClaimBenefit Requires Manual ReviewContract Term Requires Manual ReviewProvider on Pay HoldMODIFRESUBMIT CORRECTION - THE PROCODURE CODE IS INCONSISTENT WITH THE MODIFIER USED OR A REQUIRED MODIFIER IS MISSING.MRRNBSIRESUBMIT CLAIM WITH MEDICAL RECORDSResubmit claims under newborns State ID.NCCOBRESUBMIT CORRECTION-REQUIRE COB FROM PATIENT'S PRIMARY INSURANCENCDRGRESUBMIT CORRECTION - RESUBMIT WITH INPATIENT DRG FOR PROPER ADJUDICATION MEDICARE VERSION 25 AND MEDICAID VERSION 24NCREVNCSITSUBIDSVCW-9RESUBMIT CORRECTION - OUTDATED OR INCORRECT REV CODE OR MISSING REV CODERESUBMIT CORRECTION - MISSING OR INVALID CLINIC SITE IDRESUBMIT CORRECTION - CLAIM SUBMITTED WITH INCORRECT SUBSCRIBER ID RESUBMIT WITH CORRECTIONRESUBMIT CORRECTION - SERVICES DO NOT MATCH PROVIDER SPECIALTY TYPERESUBMIT CORRECTION - REQUEST W9 WITH TIN# AND NPI # FOR PROVIDER AND VENDORNOT COVERED REASONS00159220524991Services are InclusiveBenefit Restriction Message{}default message{}CPT codes billed include bundled and unbundled CPTsClaim denied. Requested information not received within 35 days.120DY20VST120 DAYS TIMELY FILINGPT HAS REACHED 20 VISIT BENEFIT MAXIMUM FOR MENTAL HEALTH VISITS240DY240 DAYS TIMELY FILINGBENEFIT USED WITHIN LAST 24 MONTH EV17AAREV18AAREV19AAREV2AAREV3APPEAL DENIED CLAIM RECEIVED AFTER 45 DAY LIMITSPlan Restriction MessagePrior authorization is awaiting medical review.Authorization Amount overrides Contract AmountAuthorization Line Manually DeniedAuthorization Line Manually PendedAuthorization Status Manually SetRemit Non PCP claim with PCP changeREMIT Qualifying claim not finalized – reversed determining claimREMIT finalized qualifying claim – reversed determining claimREMIT Claim with Enrollment Status ChangeREMIT Claim with External Enrollment Coverage Type ChangeREMIT LOI Records Added or ChangedREMIT E/R Claim reversed due to receipt of inpatient claim.This history claim was adjusted to pay/deny as recommended by ClaimCheckREMIT Claim was opened or adjusted based on request by NxPBAREMIT Claim was reversed or voided by Post Connect AdjustNon Clean ClaimRemit PCP claim with PCP changeREMIT retro term enrollment
VADPRMALMANALMCDALPRVANMODREMIT denied claim with valid enrollmentREMIT retro auth changeREMIT contract changeREMIT contract term changeREMIT retro termed Pre-XTHIS IS AN ADJUSTMENT TO A PREVIOUS CLAIMADJUSTED PER PROVIDER REQUEST (Cancellation/Void)COB MEMBER HAS PRIMARY COVERAGEOVERAGE PROJECT ADJUSTMENTTAKEBACK OTHER CARRIER PRIMARYNO RATE AVAILABLE/MANUAL PRICEPAYMENT BASED ON MEDICAID FEE SCHEDULEPROVIDER INELIGIBLE ON DATE OF SERVICEINVALID PRIMARY ANESTHESIA 069ERROR DISPOSITION 03 - SUSPENSION MEDICARE AS SECONDARY PAYER ALERTERROR DISPOSITION 02 - LINE DENIAL NON-COVERED SERVICEERROR DISPOSITION 06 - CLAIM DENIAL NON-COVERED SERVICE SUBMITTED FOR VERIFICATION OF DENIAL (CO NDITION CODE 21)ERROR DISPOSITION 03 - SUSPENSION NON-COVERED SERVICE SUBMITTED FOR REVIEW (CONDITION CODE 20)ERROR DISPOSITION 03 - SUSPENSION RETURN TO PROVIDER QUESTIONABLE COVERED SERVICEERROR DISPOSITION 01 - LINE REJECTION ADDITIONAL PAYMENT FOR SERVICES NOT PROVIDED BY MEDICAREERROR DISPOSITION 01 - LINE REJECTION MUTUALLY EXCLUSIVE PROCEDURE NOT ALLOWEDERROR DISPOSITION 01 - LINE REJECTION COMPONENT OF COMPREHENSIVE PROCEDURE NOT ALLOWEDERROR DISPOSITION 01 - LINE REJECTION CODE NOT RECOGNIZED BY MEDICARE; ALTERNATE CODE FOR SAME SER VICE MAY BEAVAILABLEERROR DISPOSITION 03 - SUSPENSION PARTIAL HOSPITALIZATION ON SAME DAY AS ELECTOCONVULSIVE THER APY (ECT) OR SIGNIFICANTPROCEDURE (TYPE T)ERROR DISPOSITION 03 - SUSPENSION PARTIAL HOSPITALIZATION WHICH SPANS THREE OR LESS DAYS AND H AS INSUFFICIENT SERVICESOR HAS SIGNIFICANT PROCEDURE (TYPE T) ON AT LEAST ONE OF THE DAYSERROR DISPOSITION 03 - SUSPENSION PARTIAL HOSPITALIZATION CLAIM SPANS MORE THAN THREE DAYS, IN SUFFICIENT DAYS WITHMENTAL HEALTH SERVICESERROR DISPOSITION 03 - SUSPENSION PARTIAL HOSPITALIZATION CLAIM SPANS MORE THAN THREE DAYS WIT H INSUFFICIENT NUMBER OFDAYS MEETING PARTIAL HOSPITALIZATION CRITERIAERROR DISPOSITION 03 - SUSPENSION EXTENSIVE MENTAL HEALTH SERVICES ON DAY OF ELECTROCONVULSIVE THERAPY OR SIGNIFICANTPROCEDUREERROR DISPOSITION 01 - LINE REJECTIONERROR DISPOSITION 01 - LINE REJECTION SERVICE IS NOT SEPARATELY PAYABLEERROR DISPOSITION 02 - LINE DENIAL SERVICE IS ON SAME DATE AS INPATIENT PROCEDUREERROR DISPOSITION 01 - LINE REJECTION NON-COVERED BY STATUTORY EXCLUSIONERROR DISPOSITION 01 - LINE REJECTION OBSERVATION SERVICE CODE ONLY ALLOWED WITH BILL TYPE 13XERROR DISPOSITION 03 - CLAIM SUSPENSION OBSERVATION SERVICE E&M REQUIREMENTS NOT MET, SERVICE DATE 01/01ERROR DISPOSITION 01 - LINE REJECTION ACTIVITY THERAPY NOT PAYABLE OUTSIDE THE PARTIAL HOSPITALIZA TION PROGRAMERROR DISPOSITION 03 - CLAIM SUSPENSION CODE REQUIRES MANUAL PRICINGERROR DISPOSITION 01 - LINE REJECTION SERVICE PROVIDED PRIOR TO FDA APPROVALERROR DISPOSITION 01 - LINE REJECTION SERVICE PROVIDED PRIOR TO DATE OF NATIONAL COVERAGE DETERMIN ATIONERROR DISPOSITION 01 - LINE REJECTION SERVICE PROVIDED OUTSIDE LIMITED APPROVAL PERIODAP074AUREQUNITS ONE FOR BILATERAL PROC BILLED W/MODIFIER 50AUTHORIZATION IS REQUIRED FOR SERVICESAUTHDAUTHORIZATION DENIEDAUTHNMPROCEDURES / SERVICES AUTHORIZED DO NOT MATCH CLAIMAUVISBHOAUTHORIZATION VISITS EXCEEDEDSERVICES NOT COVERED UNDER MEDICAL PLAN BILL BHOAP028AP031AP032AP033AP034AP036
BILLCBILLEBUNDREFUND DUE TO BILLING CORRECTION FROM PROVIDERPROVIDER BILLING ERRORBundled ServiceCHIROALL CHIRO CLAIMS NEED TO BE SUBMITTED THROUGH COLUMBINE CHIROPRACTICE SERVICESCM302Only one family planning visit allowed per date of service.COFINSUBMIT CLAIMS THROUGH COFINITY EDI PAYER #38335.CON510CONTRPer contract clinic visit billed with a revenue code 510 code is not payable. Member not liablePaid at contracted rateCRATECOFINITY NEGOTATED CASE RATE INCLUDES WELL BABY DISCHARGED 4D37D39D40D41D42D43D45D46SERVICE RESPONSIBILITY OF LAB CORP ONLYNew Member LetterRequires manual processing.Billed amount exceeds UCR.Co-Surgeon Not CoveredTeam Surgeon Not CoveredMedical review denial.Triage only - not life threatening.Requires authorized referral.Member not enrolled on DOS.Member was not enrolled with this Medical Group on DOS .Patient not enrolled with Plan.Service not a plan benefit.Included in other procedure.Limited service exceeded.Assistant surgeon not covered.Incorrect Plan ID code.Incorrect AHCCCS ID code.Unauthorized provider.Duplicate Claim (Provider/Member/DOS)Claim submit time exceeded.Procedure code not on file.Diagnosis code not on file.Member ID number invalid.Category of service invalid.Stat charges are not covered.Service a part of lab contract.Service a part of Rx contract.Included in capitation.Submitted to plan in error.Services exceed Psych benefit.Plan not notified in time.Member responsible for charges.W/O contractual agreement.Reduce to urgent care.No stat order.Adjust to authorized level of care.No response to COB inquiry.
8D79D80D81D82D83D84D85D86D87D88D89Requires H&P.Included in OB package.Split billing required.Authorization number invalid for DOS.Revenue code missing / invalid.DOS incorrect.Claim has been denied. At DOS, assigned to other PCP.The Provider is not a member of the UHC PPO Network.DME rental costs have exceeded purchase price.Patient not enrolled with plan.CPT code terminated.Denied: Workmens Compensation.N/C. Routine well baby.Non-emergent services. Medical review denial.Plan not advised in 72 hrs. Medical review denial.Claim Doesn't have any Service LinesElectronic Claim has COBDuplicate Line on Same ClaimPrior authorization is closed.Prior authorization services do not match claim.Prior authorization is denied.Prior authorization cost estimate exceeded.Prior authorization not for same member.Prior authorization is not for same provider.Provider's specialty does not match authorized specialtyProvider's group does not match authorized groupProvider's network does not match authorized networkProvider's participation status does not match authorizedProvider type does not match authorized provider typePlace of service does not match authorizedPrior authorization is pended.Prior authorization not found.Prior authorization has no units available.Prior authorization has insufficient units remainingCPT codes billed include bundled and unbundledInvalid ICD9 Procedure CodeInvalid ICD-9 Diagnosis CodeDiagnosis not valid for BenefitTeam Surgeon not coveredCo-Surgeon not CoveredClaim line exceeds available bed days on auth.Authorization line item denied.DELIVMEDICAID REQUIREMENTS IF MOM & BABY ARE DISCHARGED SAME DAY CHARGES MUST BE COMBINED.DELTADENYDH450DH541BILL TO DELTA DENTALNOT COVEREDEmergency services paid on new additional claim.TIMELY FILING
LTDHTWTDHVALDHVFCDHWINDIALDKTVDNADBADJUSTMENT FOR CONTRACT FEE SCHEDULE CORRECTIONERROR ADJUSTMENTCORRECTED CLAIM ADJUSTMENTThis is an adjustment to previous claim.INCORRECT PROVIDEROUT OF POCKET ADJUSTMENTThis claim is considered part of global contract agreement. No additional payment will be madeCHECK VOIDED INCORRECT PROVIDERNO FACTOR IN THE FEE SCHEDULE.CLAIM LINE OVERLAPS CONTRACT AFFILIATION TERM DATEPAID PER CMS CAH RATE LETTERCapped rental period reached. No further rental payments may be made.Medicaid cost-to-charge allowableINVALID CLAIM FORM TYPEPaid per % CHP Plus fee scheduleINVALID CONDITION CODE ON DOSADJUSTED PER PROVIDER REQUESTCLAIM LINE OVERLAPS CONTRACT TERM TERMINATION DATE.DIAGNOSIS POINTER REQUIRED ON SERVICE LINE FOR DIAGNOSIS CODESEAPG PRICING APPLIEDINPATIENT CLAIM / UM EXISTS FOR SAME DOS AS ER CLAIMIncluded in dialysis composite rate.CLAIM LINE OVERLAPS FEE TABLE VALUE TERMINATION DATE.Rebill with correct ICD-10 CodeREQUIRE ITEMIZED BILLMULTIPLE SURGERIES - CLAIM SUBMITTED MISSING MODIFIER 51INVALID MEDICARE COB AMOUNTINVALID MODIFIER CODE ON DOSInvalid/Missing NDC CodeInvalid NDC and J Code Combination.New born not covered under the Med Adv ProgramINVALID OCCURRENCE CODE ON DOSINVALID OCCURRENCE SPAN CODEINVALID POA INDICATOR ON DIAGNOSIS CODE.DIAGNOSIS CODE REQUIRES POA INDICATORINVALID PLACE OF SERVICE CODEClaim must be split with ICD-9 codes prior to 10/1/15 and ICD-10 codes for 10/1/15 and laterHT AND WT REQD TO CALC DIALYSIS PAYMENTINVALID VALUE CODE ON DOSVACCINE IS SUPPLIED THROUGH THE VFC PROGRAMCLAIM LINE SUBMISSION WINDOW OVERLAPOccurrence Code of Date of last Kt/V reading missingAUTH DENIED - BENEFIT EXCEEDEDHEMATOCRIT VALUE REQDDNMCADNPRIPRIMARY INSURANCE ALLOWED MEDICAID ALLOWABLE - IT IS A CONTRACTUAL ADJUSTMENT.PRIMARY PMT IS GREATER THAN ALLOWABLE CHARGE BALANCE IS A CONTRACTUAL ADJUSTMENT.DUPOCDuplicate of an original claim already in process
DUPPDDUPLICATE OF A PREVIOUSLY PAID CLAIMDV49VALUE CODE A8 OVER 500KG DIALYSISEQUIPEQUIPMENT INCLUDED WITH RENTAL/PURCHASEESRDPayment based on 2014 ESRD Pricer.EXCEDSERVICES EXCEEDED PLAN BENEFIT LIMITEXCLEXCOTRTHESE SERVICES ARE NOT COVERED UNDER THE PLANCoverage terminated for non-payment of PremiumEXCVISERVICES EXCEEDED PLAN VISIT LIMITEXHTEXMBEXMREXNCEXUVREQ MED RECS FOR DIALYSIS QTYTHESE SERVICES ARE NOT COVERED UNDER THE PLAN. MEMBER MAY BE LIABLE.DIALYSIS CLM OVER QTY FOR REV CODE 634THESE SERVICES ARE NOT COVERED UNDER THE PLAN FOR OUT OF NETWORK.VALUE CODE A9 OVER 300CM DIALYSISFM178COLORADO MEDICAL ASSISTANCE PROGRAM STERILIZATION CONSENT FORM MED 178 IS REQUIRED IN ORDER TO PROPERLY ADJUDICATETHE CLAIM.FWAGLOB1FRAUD WASTE AND ABUSEService included in payment for surgical procedure.GLOBLTHIS SERVICE IS COVERED UNDER GLOBAL PERIODGRACEH1H2GRACE DAYCredit applied for prior RAP paymentTherapy Threshold not metINGLOLIFETSERVICES INCLUDED WITH NEGOTIATED OR GLOBAL RATESERVICES EXCEEDED PLAN LIFETIME 037M0038M0039M0040M0041M0042Provider Not Active for Plan on DOSInvalid Approved Provider Service for ProviderReferral Required by ContractIncorrect age for Nursery chargesBenefit Requires Prior AuthorizationBenefit Visit Limit ExceededBenefit Dollar Limit ExceededBenefit Applies to PCP OnlyAdmit Date Required for Inpatient ClaimAttending Physician Required for Inpatient ClaimsInvalid Bill TypeInterim Claim with no Initial ClaimDuplicate Claim Line(Member/DOS/CPT(Rev))Invalid CPT ModifierInvalid CPT/HCPCSInvalid Revenue CodeModifier required for CPT/HCPCSRevenue Code Requires HCPCSPhysicians Assistant requires Modifier 80 or 27CRNA requires Modifier AAInvalid Line Date of ServiceInvalid Start DateInvalid End DateInvalid Discharge StatusInvalid Revenue Code for Bill Type
0M11M12M14M16M2M3Invalid HCPCS for Revenue CodeClaim Tiers Do Not Match ReferralMissing Primary DiagnosisAdmit Type RequiredDischarge Status RequiredInvalid For MaleInvalid For FemaleNo EnrollmentDuplicate Claim (Member/DOS)Coverage Period Insufficient for Benefit CoverageMember has no active enrollment on DOSProvider is not part of Network required for BenefitService is capitated to PCP or IPANo Attending Physician ID (Outpatient)Provider is Not CredentialedClaim amount exceeds maximum allowed during Mass AdjudicationNegative charge on claim lineProvider has Alert/MemosProvider Watch flag has been set for reviewClaim amount exceeds Maximum allowedProvider does not match required typeProvider requires a specialty codeClaim denied manuallyElectronic claim has COBBenefit has age restrictionsProvider type does not match termPCP is solely responsible for servicesPrice UB by CPT billed yes/noInvalid Admit HourAnnual Benefit Amount ExceededInvalid Discharge HourClaim Doesn't have any Service LinesGenerate 1500 From EPSDT FormClaim payment amt exceeds max allowed for mass adjudicationClaim payment amount exceeds maximum allowedClaim payment amt exceeds max allowed for mass adjudicationEARLY INTERVENTION SERVICES (EIS) ARE DENIED, PROVIDERS MUST BILL FOR EIS THRU THE EIS TRUST FUNDMEMBER IS DECEASED PRIOR TO DATE OF SERVICE ON CLAIMProvider not revalidated per Colorado MedicaidThe hospital has by contract agreed to accept as payment inServices are not eligible with diagnosis provided by physiciService is not related to direct treatment of an illness orService appears to be experimental and is not covered by theIf you have any questions concerning this claim, please callThe payment amount has been reduced by the amount paid by thThe amount shown as eligible is the maximum amount allowableThis is a duplicate of a claim that has been previously proc
M345M389M4M5M6M7M8M9Out-of-Area Claim - Pay at 80%Non-Participating Differential Contract Pricing AppliedBenefits for the above charges are subject to a reduction bePayment has been made at 85% of the eligible amount. The amPayment has been made at 100% of the eligible amount. The aWell child care is not eligible under the plan.Annual/routine physicals, or routine lab or x-rays are not eRoutine eye exams are not eligible under the plan.MAX20 2000 MAXIMUM BENEFIT EXCEEDEDMBRINMEMBER INELIGIBLE ON DATE OF SERVICEMCMAXMEMBER HAS MET THEIR MEDICARE LIFETIME MAX BENEFITMCRHOSMP001MP005MP006MP007The member has elected Hospice. Please submit claims to Medicare for PaymentWhen multiple procedures are performed on the same day, payment is made based on the highest amount allowed.Payment for this procedure is included with the payment made for medical treatment rendered on the same day by a different provider.Payment for prenatal and postnatal care is included in the payment for the obstetrical procedure. No additional payment can be made.If prenatal care and OB procedure is on paid history within 270 days, same provider, related or unrelated diag, claim is rejected.If postnatal and an OB proc. are on same claim or paid history, and postnatal care is within 45 days of post ob proc., same prov, related or unrelated diag,claim is denied.Payment for this procedure is included with the payment made for the surgical procedure.Payment for this consultation is included in the payment for anesthesia. No separate payment can be made.A payment cannot be made for more than three physical therapy procedures.If major surgery is performed same day as major/minor surgery, same POS, already paid on history and prov are same or different. Claim is pendedIf assistant surgery is performed on the same day as another asst surgery, on the same claim or paid history, same POS and the prov are different. Pendclaim.If anesthesia is performed on the same day, same POS as anesthesia no the same claim and the prov are the same or different, pay 100% of time and baseunit allowance for greater procedure and 100% of time for each lesser procedure. Pend claim.Medical necessity not established for services rendered.MAX VISITS DIALYSIS PER MONTH EXCEEDEDMAX DIALYSIS VISITS PER WEEK EXCEEDEDThis service cannot be billed separately.Payment adjusted based on x-ray radiograph on XPWKN390N775NCACSNCARQNCBMCAUTHORIZATION CLOSEDAUTHORIZATION REQUIREDNCBMDNOT COVERED BY MEDICARENOT COVERED BY MEDICAIDNCCOBNCLTKEOB FROM PRIMARY CARRIER NEEDED TO ADJUDICATE CLAIMSUBMIT CLAIMS TO LIFE TRAC FOR RE-PRICINGNCOPTNCPCASUBMIT CLAIM TO OPTUM HEALTH CARENot covered per contracted agreementNCWRPNELIGNOAUTNOCLMNOFACWRAPAROUND BENEFIT - BILL MEDICAID FEE FOR SERVICEMEMBER NOT ELIGIBLE ON DATE OF SERVICESERVICES WERE NOT AUTHORIZEDDENVER HEALTH MEDICAL PLAN DOES NOT PROCESS CLAIMS FOR THIS LINE OF BUSINESS - CLAIM DENIEDNO FACTOR IN RBRVS CANNOT CALCULATE PRICEOCE001OCE002OCE003OCE005Invalid diagnosis code.Invalid diagnosis based on patient ageInvalid diagnosis based on patient sexE- Diagnosis code can not be used as principal.
54OCE055OCE056OCE057OCE058OCE059Invalid procedure code.Invalid procedure based on patient age.Invalid procedure based on patient sexNon-covered for reason other than statuteServices submitted for FI review condition code 21Separate payment for service is not provided by the plan.Code indicates a site of services not included in OPPSInvalid/incomplete/incorrect unitsMultiple bilateral procedures without modifier 50Inappropriate specification of bilateral procedureInpatient procedure.Mutually exclusive procedure that is not allowed by NCCI even if appropriate modifier is present.Code 2 of a code pair that is not allowed by NCCI even if appropriate modifier is present.Medical visit on same day as type T or S procedure without modifier 25.Invalid modifierInvalid dateDate out of OCE rangeInvalid ageInvalid sexOnly incidental services reported.Code not recognized by Medicare; Alternate code for same service may be available.Partial hospitalization services for non-mental health diagnosis.Insufficient services on day of partial hospitalizationOnly Mental Health education and training services providedTerminated bilateral procedure or terminated procedure with units greater than one.Inconsistency between implanted device or administered substance and implantation or associated procedure.Mutually exclusive procedure that would be allowed by NCCI if appropriate modifier were present.Code 2 of a code pair that would be allowed by NCCI if appropriate modifier were present.Invalid Revenue CodeMultiple medical visits on same day with same revenue code without condition code G0Transfusion or blood product exchange without specification of blood product.Observation revenue code on line item with non-observation HCPCS codeInpatient separate procedures not paid.Partial hospitalization condition code 41 not approved for type of bill.Service is not separately payable.Revenue center requires HCPCSService on same day as inpatient procedure.Non-covered based on statutory exclusion.Multiple observations overlap in time.Observation does not meet minimum hours, qualifying diagnoses, and or T procedure conditionsCodes G0378 and G0379 only allowed with Bill Type 13xMultiple codes for the same services.Non-reportable for site of servicesEM condition not met and line item date for OBS code G0244 is not 12-31 or 01-01.EM Condition not met for separately payable observation and line item date for code G0378 is 01-01G0379 only allowed with G0378Clinical trial requires diagnosis code V707 as other than primary diagnosis.
CE87OCE88OCE89OCE90OCE91OCE92Use of modifier CA with more than one procedure not allowedCode not recognized by OPPS; alternate code for same service may be availableThis code only billed on partial hospitalization claimsAT service not payable outside the partial hospitalization.Revenue code not recognized by MedicareService provided prior to FDA approvalService provided prior to date of National Coverage Determination (NCD) approvalService provided outside approval periodCA modifier requires patient status code 20Claim lacks required device or procedure codeService not billable to Fiscal IntermediaryIncorrect billing of blood productsUnits greater than one for bilateral procedure billed with modifier 50Trauma response critical care code without revenue code 068x and CPT 99291Claim lacks allowed procedure codeClaim lacks required radiolabeled productIncorrect billing of revenue code with HCPCS codeMental health code not approved for partial hospitalization programMental health service not payable outside the partial hospitalization programCharge exceeds token charge ( 1.01Service provided on or after effective date of NCD non-coverageClaim lacks required primary codeClaim lacks required device or procedure codeOne or more lines on the claim has returned an OCE error with a Return to Provider dispositionModifier PN is reported for an item or service that is considered to be non-excepted for an off-campus provider-based hospital outpatient departmentunder Section 603Manifestation code not allowed as principal diagnosisSkin substitute application procedure without appropriate skin substitute product codeFQHC payment code not reported for FQHC claimFQHC claim lacks required qualifying visit codeIncorrect revenue code reported for FQHC payment codeItem or service not covered under FQHC PPSDevice-dependent procedure reported without device codeOFFICOOAOFFICE VISIT IS NOT PAYABLE SAME DAY A
D080 Co-Surgeon Not Covered D081 Team Surgeon Not Covered D10 Medical review denial. D11 Triage only - not life threatening. D12 Requires authorized referral. D15 Member not enrolled on DOS. D15A Member was not enrolled with this Medical Group on DOS . D16 Patient not enrolled with Plan. D17 Service not a plan benefit. D18 Included in other .