Transcription
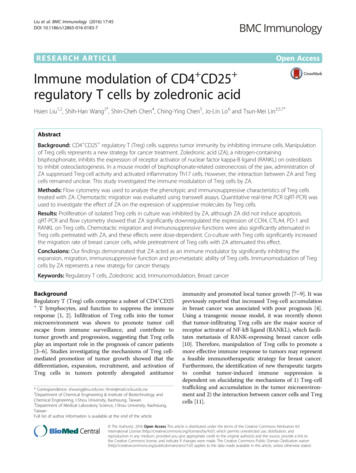
Liu et al. BMC Immunology (2016) 17:45DOI 10.1186/s12865-016-0183-7RESEARCH ARTICLEOpen AccessImmune modulation of CD4 CD25 regulatory T cells by zoledronic acidHsien Liu1,2, Shih-Han Wang2*, Shin-Cheh Chen4, Ching-Ying Chen5, Jo-Lin Lo6 and Tsun-Mei Lin3,5,7*AbstractBackground: CD4 CD25 regulatory T (Treg) cells suppress tumor immunity by inhibiting immune cells. Manipulationof Treg cells represents a new strategy for cancer treatment. Zoledronic acid (ZA), a nitrogen-containingbisphosphonate, inhibits the expression of receptor activator of nuclear factor kappa-B ligand (RANKL) on osteoblaststo inhibit osteoclastogenesis. In a mouse model of bisphosphonate-related osteonecrosis of the jaw, administration ofZA suppressed Treg-cell activity and activated inflammatory Th17 cells. However, the interaction between ZA and Tregcells remained unclear. This study investigated the immune modulation of Treg cells by ZA.Methods: Flow cytometry was used to analyze the phenotypic and immunosuppressive characteristics of Treg cellstreated with ZA. Chemotactic migration was evaluated using transwell assays. Quantitative real-time PCR (qRT-PCR) wasused to investigate the effect of ZA on the expression of suppressive molecules by Treg cells.Results: Proliferation of isolated Treg cells in culture was inhibited by ZA, although ZA did not induce apoptosis.qRT-PCR and flow cytometry showed that ZA significantly downregulated the expression of CCR4, CTLA4, PD-1 andRANKL on Treg cells. Chemotactic migration and immunosuppressive functions were also significantly attenuated inTreg cells pretreated with ZA, and these effects were dose-dependent. Co-culture with Treg cells significantly increasedthe migration rate of breast cancer cells, while pretreatment of Treg cells with ZA attenuated this effect.Conclusions: Our findings demonstrated that ZA acted as an immune modulator by significantly inhibiting theexpansion, migration, immunosuppressive function and pro-metastatic ability of Treg cells. Immunomodulation of Tregcells by ZA represents a new strategy for cancer therapy.Keywords: Regulatory T cells, Zoledronic acid, Immunomodulation, Breast cancerBackgroundRegulatory T (Treg) cells comprise a subset of CD4 CD25 T lymphocytes, and function to suppress the immuneresponse [1, 2]. Infiltration of Treg cells into the tumormicroenvironment was shown to promote tumor cellescape from immune surveillance, and contribute totumor growth and progression, suggesting that Treg cellsplay an important role in the prognosis of cancer patients[3–6]. Studies investigating the mechanisms of Treg cellmediated promotion of tumor growth showed that thedifferentiation, expansion, recruitment, and activation ofTreg cells in tumors potently abrogated antitumor* Correspondence: shwang@isu.edu.tw; ltmei@mail.ncku.edu.tw2Department of Chemical Engineering & Institute of Biotechnology andChemical Engineering, I-Shou University, Kaohsiung, Taiwan3Department of Medical Laboratory Science, I-Shou University, Kaohsiung,TaiwanFull list of author information is available at the end of the articleimmunity and promoted local tumor growth [7–9]. It waspreviously reported that increased Treg-cell accumulationin breast cancer was associated with poor prognosis [4].Using a transgenic mouse model, it was recently shownthat tumor-infiltrating Treg cells are the major source ofreceptor activator of NF-kB ligand (RANKL), which facilitates metastasis of RANK-expressing breast cancer cells[10]. Therefore, manipulation of Treg cells to promote amore effective immune response to tumors may representa feasible immunotherapeutic strategy for breast cancer.Furthermore, the identification of new therapeutic targetsto combat tumor-induced immune suppression isdependent on elucidating the mechanisms of 1) Treg-celltrafficking and accumulation in the tumor microenvironment and 2) the interaction between cancer cells and Tregcells [11]. The Author(s). 2016 Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, andreproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link tothe Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication o/1.0/) applies to the data made available in this article, unless otherwise stated.
Liu et al. BMC Immunology (2016) 17:45Zoledronic acid (ZA) is a third-generation nitrogencontaining bisphosphonate (BP) and is able to suppressosteoclastogenesis via the inhibition of RANKL expression on osteoblasts [12, 13]. Some preclinical and clinicalfindings suggested that ZA also has anti-tumor and antimetastatic properties, and ZA has been reported to inhibit angiogenesis, suppress tumor cell invasion, inducetumor cell apoptosis and induce cytotoxic γδ T cells[14–19]. ZA is currently used as an adjuvant treatmentfor early stage breast cancers. The phase III AustrianBreast and Colorectal Cancer Study Group trial 12(ABCSG-12) recently reported that the addition of ZAto endocrine therapy increased the duration of diseasefree survival in patients with estrogen receptor-positivebreast cancer. ZA was shown to reduce both local regional and distant metastases, suggesting that it mightact directly on micrometastases of breast cancer cells[20]. The Zometa-Femara Adjuvant Synergy Trial (ZOFAST), which was the largest study using ZA, alsoshowed encouraging results when ZA was added to theadjuvant therapy of breast cancer [21]. More recently,data from the Adjuvant Zoledronic acid to reduce recurrence (AZURE) trial also suggested that ZA potentiatedthe activity of adjuvant endocrine therapy in postmenopausal patients [22]. Furthermore, a mouse model ofZA-related osteonecrosis of the jaw showed that ZAinhibited Treg-cell activity [23]. Although the immunomodulatory effect of ZA was proposed as being relatedto Treg cells, the interaction between ZA and Treg cellswas unclear. The aim of this study was to investigatehow ZA affected tumor immunity via Treg cells.MethodsIsolation and expansion of regulatory T cellsPeripheral blood mononuclear cells (PBMCs) were isolated from 100 ml of fresh heparinized peripheral bloodfrom healthy volunteers by Ficoll-Hypaque (GE Healthcare, Uppsala, Sweden) gradient centrifugation. The cellsfrom the interface were washed three times in HBSS andseeded in 6-well microtiter plates in RPMI-1640 medium,and allowed to settle at 37 C in a humidified atmospherewith 5% CO2. After 30 min, the non-adherent cells werecollected as lymphocytes. Treg cells were immediatelypurified from PBMCs by immunomagnetic separationusing the Dynabeads Regulatory CD4 CD25 T Cell Kit(Invitrogen , Oslo, Norway), according to the manufacturer’s instructions. In brief, CD4 cells were isolated bynegative selection after depletion of cells expressing CD8,CD14, CD16, CD19, CD36, CDw123, CD235a and CD56.CD25 cells were then selected by positive selection usingmagnetic beads directly conjugated to an anti-CD25 Ab.The procedure yielded a highly pure preparation ( 95%purity) of regulatory CD4 CD25 T cells, more than 80%of which expressed the intracellular transcription factor,Page 2 of 10Foxp3. The isolated Treg cells were expanded withDynabeads Human Treg Expander (Gibco , Oslo,Norway) containing 100 U/ml rIL2 (Gibco , Carlsbad, CA,USA). The study was approved by the Institutional ReviewCommittee of E-DA Hospital and the volunteers providedwritten informed consent.Chemicals, antibodies and cell lineZoledronic acid (ZA) was provided by Novartis PharmaAG Basel, Switzerland. Monoclonal antibodies againsthuman CD25-PE, CD152 (CTLA-4)-PE, FOXP3-FITC,and CD279 (PD-1)-FITC were purchased fromeBioscience, San Diego, CA, USA. CD194 (CCR4)PerCP-CyTM 5.5, and CD69-FITC were purchased fromBD Biosciences, San Jose, CA, USA. The MDA-MB-231breast cancer cell line was purchased from the AmericanType Culture Collection (Food Industry Research andDevelopment Institute, Taiwan) and was cultured withDMEM medium (Gibco , Grand Island, NY, USA), containing 10% fetal bovine serum (FBS: Biological industries, Kibbutz Beit HaEmek, Israel). Conditioned media(CM) harvested from MDA-MB-231 cells consisted ofDMEM supplemented with 2% FBS in which cells werecultured for 48 h. CM was collected, sterile filtered andstored in aliquots at 80 C.Proliferation assayExpanded Tregs and lymphocytes were labelled with2 μM carboxyflourescein diacetate succinimidyl ester(CFSE) (BD Biosciences, San Jose, CA) at 37 C for15 min. The cells were seeded in 12-well plates at adensity of 2.5 106 cells/well, cultured with culturemedium in 0, 10 and 100 μM ZA, and stimulated withCD3/CD28 micro beads. The culture media was changedevery 3 days and measured. They were analyzed usingthe Cell Quest Pro software (BD Biosciences, San Jose,CA) or WinMDI software.Treg cells apoptosis assaysApoptosis of Treg cells was analyzed by seeding Tregcells at a density of 5 105cells/well, and starving themovernight in serum free DMEM. The cells were thentreated with ZA (0 or 100 μM) for 24 h in DMEM supplemented with 2% FBS. Cells were harvested and incubated with FITC-labeled Annexin V and PropidiumIodide Staining Solution (eBioscience, San Diego, CA,USA). The percentages of apoptotic and necrotic cellswere determined by flow cytometry (FACScalibur; BDBiosciences, San Jose, CA, USA). Five parallel sampleswere measured and 10,000 events were analyzed usingCell Quest Pro software (BD Biosciences, San Jose, CA,USA) or WinMDI software (San Diego, CA, USA). Inaddition, Treg cells were centrifuged onto microscopeslides using a Cytospin2 centrifuge (Shandon Inc.,
Liu et al. BMC Immunology (2016) 17:45Pittsburgh, PA, USA); the slides were stained withWright-Giemsa solution and observed by light microscopy (Olympus, Tokyo, Japan).Treg cells migration assaysMigration assays were performed in 24-well transwellchambers (Corning, New York, NY, USA) using 8-μmpore polycarbonate filters. Treg cells pre-treated for 4 hwith different concentrations of ZA (0, 50 and 100 μM)were added to the inner chamber in serum-free RPMImedium in a final volume of 100 μL. The chemoattractants, including 2% FBS-containing DMEM or CM fromMDA-MB-231 cells, were placed in the bottom chamberof the transwells in a total volume of 650 μL. Transwellchambers were incubated at 37 C for 2 h, and the number of cells in the lower chamber was counted. Thechemotaxis index was calculated by dividing thenumbers of cells migrated in response to CM of MDAMB-231 cells or after pretreatment with ZA by thenumbers of cells migrated in response to medium only.Page 3 of 10RNA mini kit (Viogene, Sunnyvale, CA, USA) accordingto the manufacturer’s instructions. Samples of total RNA(1–2.5 μg) were reverse-transcribed using iScriptTMcDNA Synthesis Kit (Bio-Rad, Foster City, CA, USA) according to the manufacturer’s instructions. Real-timePCR was carried out (iTaqTM Universal SYBR@ GreenSupermix; Bio-Rad, Foster City, CA, USA) with primersspecific for the human gene (Table 1). Fluorescence RTPCR analysis was performed using ABI PRISM 7700Sequence Detection System (Applied Biosystems,Warrington, WA, USA). PCR amplification was performed with 1 cycle of 50 C for 2 min, 1 cycle of 95 Cfor 15 min, and 40 cycles of 95 C for 15 s followed by58 C for 1 min. Analysis of relative gene expression wasperformed using the 2-ΔΔCT method [25]. The CT isthe threshold cycle number that is the minimal cycle forsample detection. The arithmetic formula for the ΔCTmethod is the difference in CT between the detectedgene and the GAPDH housekeeping gene.Statistical analysisWound healing migration assayFor wound healing migration assays, MDA-MB-231 cellswere cultured in 6-cm dishes at a density of 1 106cells/dish until confluent (0 h). A straight scratch wasmade in the center of the plate using a 200 μL pipettetip. The MDA-MB-231 cells were then incubated for12 h with Treg cells, which had been pre-treated withZA (0, 25, 50 or 100 μM) for 24 h. Wound healing wasevaluated by microscopy. The average cell migrationdistances were measured using an inverted phasecontrast microscope (Zeiss, Primovert, Germany).Immunosuppressive function assaysTreg cells were cultured in medium or CM of MDAMB-231 cells for 72 h and treated with different concentrations of ZA for 24 h. Their immunosuppressiveactivity was determined with a Human Regulatory T CellFunction Kit (BD Biosciences, San Jose, CA, USA). Inbrief, the harvested Treg cells (2x105) were co-culturedin 24-well plates with responding effector cells (PBMC4x105) in the presence of T-cell specific stimulated CD3/CD28 beads. FITC-labeled CD69 was present for theentire duration of stimulation in order to analyze thetransiently expressed CD69 on the surface of the effectorcells. After 7 h of activation, the percentage of CD69positive effector T cells was determined by flow cytometry [24]. The percent suppression was calculated by thefollowing formulas: 100–[(% CD69-positive in presenceof Tregs/% CD69-positive in absence of Tregs) 100].Results represent at least 3 independent experiments.Results are presented as mean SD. The statisticalanalysis was performed using Prism version 5.00 software (GraphPad Software, USA). All comparisons weremade between two groups with the two-tailed Student’st-test, among more than three groups with one-wayANOVA. P values of 0.05 were considered statisticallysignificant.ResultsZA inhibits proliferation of Treg cellsExpended Treg cells and freshly isolated lymphocyteswere treated with 10 μM ZA in order to evaluate the effect of ZA on Treg-cell proliferation. CD4 lymphocytesTable 1 Primer sequences used for quantitative RT-PCR formRNA expressionTarget geneOligonucleotide sequences (5′-3′)ForwardReverseFoxp3TGA CCA AGG CTT CATCTG TGGAG GAA CTC TGG GAA TGTGCCCR4CTT CAG TCA CCT GGCTGT CACTC AGC TGA ACC TGG CTACCTGF-βGGA AAC CCA CAA CGAAAT CGCT CTG ATG TGT TGA AGAACRANKLACC AGC ATC AAA ATCCCA AGCCC CAA AGT ATG TTG CATCCCTLA-4CTC AGC TGA ACC TGGCTA CCCCA CTT GCA GAC ACC ATTTGPD-1ATC AAA GAG AGC CTGCGG GGGT GGG CTG TGG GCA CTGAPDHTGA ACG GGA AGC TCACTG GTCC ACC ACC CTG TTG CTGTAQuantitative real-time polymerase chain reaction assayTreg cells were treated with various concentration of ZAfor 6 h, and total RNA was extracted using the total
Liu et al. BMC Immunology (2016) 17:45proliferation demonstrated no difference in the presenceof 10 μM ZA (Additional file 1: Figure S1). In contrast,Treg-cell proliferation was significantly suppressed inthe presence of 10 μM ZA (Fig. 1a). Inhibition of proliferation was observed as early as 6 days after ZA treatment Treatment with 10 μM ZA for 12 days inhibitedproliferation by more than 28% (Fig. 1b). In addition,Treg cells treated with ZA for 24 h exhibited abundantcytoplasmic vacuoles, suggesting survival stress and earlycell injury (Fig. 1c). However, annexin V and PI stainingshowed no evidence of apoptosis even in cells treatedwith 100 μM ZA for 24 h (Additional file 2: Figure S2).Page 4 of 10ZA inhibits chemotactic migration of Treg cellsTranswell assays were used to evaluate the effect of ZAon the chemotactic migration of Treg cells in responseto DMEM supplemented with 2% FBS or CM fromMDA-MB-231 cells. We found that MDA-MB-231 cellCM had a greater (4.12 0.19 folds) increase in Treg-cellchemotaxis compared with DMEM with 2% FBS (p 0.001). ZA pretreatment significantly inhibited migrationof Treg cells in response to CM from MDA-MB-231cells. However, the migration of ZA-pretreated Tregcells was not significantly affected in the presence ofDMEM containing 2% FBS (Fig. 2).Fig. 1 ZA inhibits Treg cells proliferation and induces cell injury. a Expanded Treg cells were labeled with CFSE and cultured in Treg cell mediumwith or without 10 μM ZA. b Treg cell proliferation curves were measured based on the percentage of cells with decreased fluorescence ascompared to non-proliferating cells (0.38% at day 1). Data represent the mean values SEM and results from three independent experiments areshown. Statistical significance (P 0.01) is denoted by **. c The morphology of Treg cells was analyzed by microscopy in 100 oil immersion afterZA treatment for 24 h
Liu et al. BMC Immunology (2016) 17:45Fig. 2 ZA inhibits Treg cells chemotactic migration. Treg cells(5 10 4) were pretreated with 0, 50 or 100 μM ZA for 4 h, andplaced in the upper chambers. Migration of Treg cells into the lowerchambers containing DMEM with 2% FBS or CM from MDA-MB-231cells after 2 h was analyzed. The chemotaxis index shown comparesmigration with the response of control cells to DMEM with 2% FBS.Values are means SEM of results from three independent experimentsin duplicate. *P 0.05, ** p 0.01, ***p 0.001ZA alters the phenotypic expression of Treg cellsThe affinity between chemokine (C-C motif ) ligand 2(CCL2) released by tumor cells and chemokine (C-Cmotif ) receptor 4 (CCR4) expressed on Treg cells hasbeen shown to play a major role in the recruitment ofTreg cells to tumor sites [26, 27]. Cytotoxic T-lymphocyte antigen 4 (CTLA4), a surface protein receptor associated with the transmission of an inhibitory signal to Tcells, is expressed on functional Treg cells [28, 29].Thus, these phenotypic characteristics of Treg cells wereanalyzed by flow cytometry after treatment with ZA. Wefound a significant decrease in the expression of CCR4and CTLA4 on Treg cells after treatment with 100 μMZA (Fig. 3). In addition, 100 μM ZA treatment significantly decreased the mRNA expression of CCR4, butnot Foxp3 (Fig. 4a, b) as determined by qRT-PCR.Transforming growth factor beta (TGF-β) and programmed cell death 1 (PD-1) are negative regulators ofT cell immune responses required for maintainingperipheral tolerance by Treg cells [30–32]. We showedthat Treg cells treated with ZA exhibited a significantdecrease in the expression of PD-1 but not TGF-β(Fig. 4c, d). Therefore, ZA effectively altered thephenotype and function of Treg cells, in vitro.ZA inhibits the ability of Treg cells to sustain breastcancer cell migrationWe investigated whether the ability of Treg cells toenhance the migration of breast cancer cells was modulated by ZA treatment. Wound healing assays performedwith MDA-MB 231 cells showed that co-culture withTreg cells significantly increased the migration rate ofPage 5 of 10breast cancer cells, compared with MDA-MB 231 cellsalone (132.8 9.5%, P 0.05; Fig. 5a, b). However, whenMDA-MB-231 cells were co-cultured with Treg cellspretreated with ZA, there was a significant and dosedependent decrease in their migration compared totumor cells co-cultured with untreated Treg cells (Fig. 5a,b). In particular, Treg cells pretreated with 100 μM ZAshowed pronounced inhibition of MDA-MB-231 cellmigration (Fig. 5b; p 0.05).The metastatic spread of carcinoma cells is related tothe production of RANKL by Treg cells. ZA treatmentwas previously shown to downregulate the expression ofRANKL by osteoblasts [12, 13]. Using qRT-PCR, weshowed that ZA treatment downregulated the expressionof RANKL by Treg cells in a dose-dependent manner(Fig. 5c). These results implied that ZA-mediated downregulation of RANKL by Treg cells might attenuate theability of Treg cells to promote the migration ofMDA-MB-231 cells.ZA inhibits immunosuppressive function of Treg cellsCD69 is an early activation marker on effector T cells,thus we investigated whether isolated Treg cells couldsuppress T cell activation after 7 h in culture. PBMCswere cultured either alone or together with autologousisolated Treg cells at a 2:1 ratio in the presence of antiCD3/CD28–coated microbeads and CD69 expressionwas measured by flow cytometry. The results show thatpretreatment of Treg cells with 100 μM ZA inhibitedtheir immunosuppressive function, as evidenced by increase expression of CD69 (16.9 3.8% vs. 12.0 0.5%)(Fig. 6a), the percentage of Treg suppression was significantly decreased (51.8 4.0% vs. 44.9 5.6%) (Fig. 6c).Interestingly, pretreatment of Treg cells with CM fromMDA-MB-231 cells significantly inhibited CD69 expression on effector T cells (16.3 0.4% vs. 12.1 1.3%; p 0.05), but the suppressed effect was reversed andincreased by ZA treatment in a dose-dependent manner(Fig. 6b). The percent suppression of CM pretreatedTreg cells were significantly attenuated by 100 μM ZAtreatment (Fig. 6d).DiscussionPatients with early-stage breast cancer and multiplemyeloma have been shown to benefit from the additionof ZA to adjuvant endocrine therapy, or to standardchemotherapy, respectively [20, 33]. Previous reportshave also demonstrated the efficacy of ZA therapy inpostmenopausal women, although the underlying mechanism is not fully understood [34, 35]. ZA treatment forosteoporosis is frequently associated with the onset ofan acute phase reaction to the activation of γδ T cells[36]. In contrast, human γδ T cells have been shown todisplay potent cytotoxicity against various tumor cells
Liu et al. BMC Immunology (2016) 17:45Page 6 of 10Fig. 3 ZA influences the expression of markers associated with Treg cells suppressive function. Representative flow cytometry results of (a) CCR4and (b) CTLA4 on Treg cells treated with 100 μM ZA (dotted line) and untreated Treg cells (shaded histogram). The negative control (unstainedTreg cells) is shown as an open histogram. Median fluorescence intensity (MFI) is plotted against the ZA concentration (μM); the results from fourindependent experiments are shown. Significant difference in MFI determined using the one-way ANOZA;*p 0.05after pretreatment with ZA [19]. There is increasingevidence to suggest that Treg cell-mediated immunosuppression plays an important role in the progression andmetastasis of breast cancer, and immune escape bytumor cells is the major challenge to current immunotherapeutic strategies [37]. These studies suggested thatthere is an urgent need to increase the efficacy ofimmunotherapy by exploring therapeutic interventionsthat inhibit the function of Treg cells in tumor-bearinghosts [11]. The effect of ZA on the immune modulatoryfunction of Treg cells was previously not well understood. Previous studies using ZA treatment on othercells (oral keratinocytes and osteosarcoma cells) demonstrated cell cycle arrest in S phase through variousFig. 4 Influence of ZA on mRNA expression by Treg cells. mRNA levels were evaluated by qRT-PCR in Treg cells treated with 0, 50, 100 μM ZA for6 h. The gene expression values were normalized to GAPDH expression. The relative mRNA expression of (a) CCR4, (b) Foxp3, (c) TGFβ and (d)PD-1 was calculated from Treg cells treated with ZA compared with untreated Treg cells. Values shown are means SEM of results from fourindependent experiments performed in duplicate. *p 0.05
Liu et al. BMC Immunology (2016) 17:45Page 7 of 10Fig. 5 Effects of ZA on the ability of Treg cells to enhance MDA-MB-231 cell migration. a Representative pictures of migration (wound closing) ofMDA-MB-231 cells grown as a mono-culture or co-culture with Treg cells at 0 and 12 h after wounding (100 magnification). b Quantification ofthe migration distance as a percentage of the control (MDA-MB-231 cells only). c The relative RANKL mRNA expression was evaluated by qRT-PCRfrom Treg cells treated with 0, 50, or 100 μM ZA for 6 h. The results from three independent experiments are shown. *P 0.05, **p 0.01mechanisms. [38, 39] In this study, we showed that ZAinhibited the proliferation and chemotactic migration ofTreg cells, thereby improving the antitumor immune response. Recently, Ghigo et al. found a similar effect ofZA, which down-regulated indoleamine 1,2 dioxygenaseand enabled the proliferation of T cells and inhibited theexpansion of Treg cells [40].We evaluated the effects of ZA on Treg cells suppressive function and gene expression, in vitro. Treg cells arerecruited to the stroma of developing breast tumors andplay a fundamental role in the pathogenesis of metastasis[10]. In this study, we demonstrated for the first timethat the migration of Treg cells towards cancer cells wassignificantly inhibited by ZA. ZA also inhibited theexpansion and immunosuppressive function of Treg cellsin vitro. Our data suggested that the ZA-mediatedattenuation of immune evasion and tumor progressionwas effected via inhibition of Treg cell recruitment byprimary tumors, and a decrease in the number oftumor-infiltrating Treg cells. Studies on bisphosphonaterelated osteonecrosis of the jaw (BRONJ) has shown thatadministration of ZA and dexamethasone causedBRONJ-like symptoms in mice, and this was attributed,in part, to suppression of Treg cells and activation of theinflammatory T-helper-producing interleukin 17 cells(Th17). They demonstrated systemic infusion with mesenchymal stem cells or thymus-derived Tregs couldprevent and cure BRONJ-like disease via inhibition ofTh17 and increase in Tregs. In addition, Tregs have beenshown in vitro and in vivo to suppress Th17 cells; theBRONJ-like mice model showed that treatment withZol/Dex suppressed both Tregs and the Treg/Th17 ratioin peripheral blood [23]. ZA not only inhibited Treg-cellfunction, but also enhanced cellular immunity via expansion of cytotoxic γδ T cells and MHC-restricted αβ CD8 T cells [41]. These data, along with ours, suggestedthat ZA induced immune modulation to suppress Treg-cell functions. To the best of our knowledge, we are thefirst to demonstrate that treatment with ZA blocked theRANK/RANKL pathway to significantly inhibit cancercell migration induced by Treg cells. Our data wereconsistent with previous studies, which suggested thatstrategies to deplete Treg cells in breast cancer patients[42, 43] may also be beneficial by reducing localimmunosuppression and removing a primary source ofRANKL required for tumor metastasis.The concentrations of ZA used in our experiments(25–100 μM) were much higher than the plasma levelsthat are observed following intravenous administrationof the drug (about 1–2 μM) [44]. Since ZA mainly accumulates in bone tissue and is retained for long periodsof time, it is possible that ZA can reach high concentrations within the bone marrow microenvironment wherelarge numbers of functional Treg cells accumulate [45].
Liu et al. BMC Immunology (2016) 17:45Page 8 of 10Fig. 6 ZA inhibits the immunosuppressive function of Treg cells. a Treg cells were treated with 0, 50, or 100 μM ZA for 24 h, and co-cultured withautologous anti-CD3/CD28-stimulated PBMCs for 7 h. The percentage of CD69 expression on effector T cells was analyzed by flow cytometry. bTreg cells were pretreated with CM from MDA-MB-231 cells for 72 h, followed by 0, 50, 100 μM ZA treatment for 24 h. The Tregs were thenco-cultured with autologous anti-CD3/CD28-stimulated PBMCs for 7 h. The percentage of CD69 expression on effector T cells was analyzed byflow cytometry. c and d The percent suppression of the Tregs on effector T-cell without (c) and with (d) pretreated by CM from MDA-MB-231cells after ZA treatment. The percent suppression was calculated by the following formula: 100–[(% CD69-positive in presence of Tregs/%CD69-positive in absence of Tregs) 100]. Values shown are means SEM of results from four independent experiments performed induplicate. *P 0.05In fact, bone marrow is a reservoir for Treg cells thattraffic through CXCL12/CXCR4 signals [46]. We demonstrated that there may be two different mechanismsunderlying the anti-tumor effect of ZA in breast cancer.Inhibition of Treg-cell migration by ZA could significantly impair the recruitment of Treg cells by breastcancer cells, resulting in reduced progression of micrometastatic foci in soft tissues. Alternatively, ZA couldact on breast cancer micrometastases within the bonemarrow. Although it is possible that ZA in this lattermodel might directly inhibit breast cancer cell growth, itis more likely that ZA-mediated inhibition of factorsproduced by Treg cells, which promote cancer cell migration, significantly hampers the ability of tumor cellsto form distant metastases [10].The level of Foxp3 protein expression in Treg cells iscritical for immune suppression, and knockdown ofFoxp3 was previously shown to result in impaired immune suppression [47]. CTLA4 and PD-1 expression byTreg cells is constitutive and critical to their suppressivefunction [29, 32]. Additionally, the RANK-RANKL signaling pathway is critically involved in regulating thefunction of Treg cells in a mouse model of colitis [48].These studies were all consistent with our data showingthat downregulation of CTLA4 and RANKL resulted ininhibition of Treg cells’ immunosuppressive function.ConclusionsPatients with early-stage breast cancer and multiplemyeloma have been shown to benefit from the additionof ZA to adjuvant endocrine therapy, or to standardchemotherapy. In this study, we demonstrated that ZAinfluenced the suppressive activity of Treg cells and significantly affected the ability of Treg cells to secreteRANKL, which is known to promote breast cancer cellmigration. ZA acted as an immune modulator by significantly inhibiting the expansion, migration, immunosuppressive function and pro-metastatic ability of Treg cells.Our data suggested that immunomodulation of Tregcells by ZA is a novel strategy for cancer therapy.Additional filesAdditional file 1: Figure S1. The effect of ZA on CD4 lymphocyteproliferation. (A) Isolated lymphocytes were labeled with CFSE, cultured inmedium with or without 10 μM ZA and sensitized with anti-CD3 andanti-CD28 antibodies. (B) CD4 lymphocyte proliferation curves weremeasured based on the percentage of cells with decreased fluorescence
Liu et al. BMC Immunology (2016) 17:45as compared to non-proliferating cells (0.4% at day 1). Data represent themean values SEM and results from three independent experiments areshown
RESEARCH ARTICLE Open Access Immune modulation of CD4 CD25 regulatory T cells by zoledronic acid Hsien Liu1,2, Shih-Han Wang2*, Shin-Cheh Chen4, Ching-Ying Chen5, Jo-Lin Lo6 and Tsun-Mei Lin3,5,7* Abstract Background: CD4 CD25 regulatory T (Treg) cells suppress tumor immunity by inhibiting immune cells. Manipulation of Treg cells represents a new strategy for cancer treatment.