Transcription
Ohio’s strategy to enroll primary carepractices in the federal ComprehensivePrimary Care Plus (CPC ) ProgramGreg Moody, DirectorGovernor’s Office of Health TransformationWebinar for Primary Care PracticesJune 10, 2016www.HealthTransformation.Ohio.gov
1. Review core elements of the Ohio PCMH model2. Provide a comparison to CPC 3. Review the CPC practice application
Ohio’s State Innovation Model (SIM) partners
Overview of Ohio’s Patient-Centered Medical Home (PCMH)care delivery and payment model There is one Patient-Centered Medical Home (PCMH) modelin which all practices participate, no matter how close to anideal PCMH they are today. The program is designed toencourage practices to improve how they deliver care to theirpatients over time. The Ohio PCMH model is designed to be inclusive: all Medicaidmembers are attributed or assigned to a provider. In order to join the program, practices will have to submit anapplication and meet enrollment requirements. Model scheduled to launch with an early entry cohort inJanuary 2017 then open to any primary care practice thatmeets model requirements in January 2018 and beyond.
Ohio’s vision for PCMH is to promote high-quality,individualized, continuous and comprehensive care
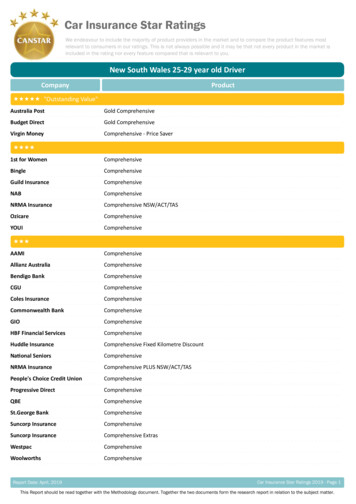
Ohio’s PCMH Requirements and Payment Streams 1 8 activityRequirements2 5 Efficiencyrequirements PaymentStreams Same-day appointments24/7 access to careRisk stratificationPopulation managementTeam-based caremanagementFollow up after hospitaldischargeTracking of follow up testsand specialist referralsPatient s ED visitsInpatient admissions forambulatory sensitiveconditionsGeneric dispensing rate ofselect classesBehavioral health relatedinpatient admitsEpisodes-linked metricMustpass 30%All requiredSharedSavingsAll requiredTBD for select practices3 20 Clinical Measures4 Total Costof CareClinical measures aligned withCMS/AHIP core standards forPCMHMustpass 50%Enhanced payments wouldbegin January 1, 2018 forany PCP that meets therequirementsBased on selfimprovement &performancerelative to peers
Ohio PCMH Model Practice Eligibility(January 1, 2018 and beyond)Required Eligible provider type and specialty Minimum size: 500 attributed/ assigned Medicaid eligible members within acontracted entity Commitment– To sharing data with payers/ the state1– To participating in learning activitiesNot required– To meeting activity requirements in 6 monthsNot required Accreditation: (e.g., NCQA or URAC) Planning (e.g., develop budget, plan for care delivery improvements, etc.) Tools (e.g., e-prescribing capabilities, EHR, etc.)1 Examples include sharing best practices with other PCMHs, working with existing organizations toimprove operating model, participating in state led PCMH program education at kickoff
Ohio’s Comprehensive Primary Care (CPC) Timeline2015CPC“Classic”CPCStatewideCPC 2016Year 3 2017Year 4Ohio’s SIMsponsoredPCMH modelDesignMedicare-sponsoredPayers apply by regionPractices applywithin regionsEarly Entry into the Ohio CPC Model CPC practices with 500 Medicaid members Practices with 500 Medicaid members withclaims-only attribution AND NCQA III Practices with 5,000 Medicaid members andnational accreditation 201820202019Southwest Ohio’s federally-sponsored,multi-payer PCMH modelYear 1Year 2Year 3 (early entry)(open entry)(open entry)Year 1Year 2Year 3 5(CMS-selected)(CMS-selected)(CMS-selected)Ongoing Enrollment into the Ohio CPC Model Any practice with 500 Medicaid membersthat meets Ohio CPC activity, efficiency andclinical quality requirements
1. Review core elements of the Ohio PCMH model2. Provide a comparison to CPC 3. Review the CPC practice application
Overview of the Federal Comprehensive PrimaryCare Plus (CPC ) Payment ModelCPC is a new payment model that rewards value in primary care forMedicare beneficiaries and encourages multi-payer collaboration Partners sought include: Medicaid FFS, Medicare Advantage,Medicaid managed care, and commercial insurers (ASO and full risk) Practices can apply to one of two tracks dependent on level ofreadiness to assume financial risk (assessed based on EHR readiness) Non-financial benefits include learning program and data sharingCMS intends to select 5,000 practices across 20 regions nationwide
Alignment of CPC model with Ohio PCMH designOhio PCMHCare modelEligible practices Care Model based on key principles of access,coordination, care management, patientengagement, population health management Similar principles Open provider enrollment and inclusive ofmost primary care practice types Application process and excludespediatrics and FQHCsDefinition of practice Group based on tax ID numberPMPMPaymentstreams Risk-adjusted PMPM based on patient status Defined as site rather than group Track 1 vs. 2 have different PMPMsIncentive Shared savings based on quality / efficiency Pay for performance bonusAlt. to FFS Episode-based payment model Track 2 includes partial capitationEHRProgramRequirementsCPC EHR not requiredActivities 8 specific activity requirementsClinicalquality 20 specific clinical quality measuresEfficiency 5 specific efficiency measures EHR required Similar activity requirements 7 of 20 metrics are the same Information not yet released
Application Process for CPC PayerApplicationsCMS SelectsRegionsPracticeApplicationsCMS SelectsPracticesApril 15 – June 8Payers submitapplicationsJune 8 – July 1520 RegionsSelectedJuly 15 – Sept. 1Practices submitapplicationsSept. 1 – Dec. 315,000 practicesselectedPreference given to CPCi and MAPCPparticipants, andMedicaid SIM statesCMS evaluatespayers and selectsregions based onpayer footprint States may need additional waivers/SPAs to apply State created atemplate for payersto apply 20 regions to beselected – intent toaward to the 7current CPCi regionsplus 13 new regionsRegional size andboundaries to bedetermined Practices in selected regions eligible toapplyEvaluation based onpractice diversity(e.g., size, location) Application includes program integritycheck, questionsregarding caremodel, and letters ofsupport includingfrom IT vendorCMS-selectedpractices eligible forCPC Medicarepayments beginningJanuary 1, 2017 State will create atemplate forpractices to apply
All of Ohio’s State Innovation Model (SIM) partnerssubmitted payer applications for CPC
Ohio application of CPC payment streams by line of businessOhio MedicaidFFSOhio MedicaidManaged CareMedicareFFSODMMCP2CMS500 (across allMedicaid members)500 (across allMedicaid members)150 MedicareFFS membersDetermined by planTrack 11 3-5 average 3-5 average 15 averageDetermined by planTrack 21 3-5 average 3-5 average 28 averageDetermined by planTrack 150% gain-sharingrate on TCOC350% gain-sharingrate on TCOC3 2.50 PMPM payfor performanceDetermined by planTrack 265% gain-sharingrate on TCOC65% gain-sharingrate on TCOC 4.00 PMPM payfor performanceDetermined by planTrack 2OnlyEpisodes onlyEpisodes onlyPartial capitationDetermined by planPayerMinimum panel iveto FFS1 Single payment reflects both CPC and PCMH; in no instance would there be double payment2 MCP administers payment in all cases; PMPM payment would be supported through ODM3 Practices would have potential opportunity to earn the higher gain-sharing rate due to highestperformance on TCOC in baseline yearCommercial /Medicare AdvantagePlan
1. Review core elements of the Ohio PCMH model2. Provide a comparison to CPC 3. Review the CPC practice application
Core Elements of the CPC practice applicationA Preliminary questionsB Practice structure and ownershipC Model participationD Practitioner and staff informationE Practice activitiesF Health information technologyG Patient demographicsH Practice revenue and budgetI Care deliveryJ AccessK Quality improvement 43 questions within the 11chapters (detail follows) Accompanying letters of supportalso required from clinicalleadership, owner of parentorganization, and IT vendors
CMS Provider Resources for CPC Model -modeloverviewslides.pdf Frequently asked s-faqs.pdf Program plus-practicecaredlvreqs.pdf Request for plus-rfa.pdf
CPC Model Frequently Asked QuestionsQuestion Would participation in CPC support eligibility for MedicareAccess and CHIP ReauthorizationAct (MACRA) AlternativePayment Model (APM) track?Some indications from CMS forparticipation to support APM, albeiton a long-term timeline Can providers participate in CPC and Medicare Shared SavingsProgram (MSSP)?Confirmation from CMS that MSSPparticipants eligible for CPC model Would dual-eligible Ohioans be included in the CPC model?Yes – dual eligible Ohioans areincluded in the CPC model, with theexception of those in ademonstration project. Dual eligibleOhioans are not included in PCMH What are the core elements ofthe practice application?MACRAMSSPDual eligiblemembersPracticeapplicationResponse Any other questions?Detail follows
Preliminary pre-decisional working draft; subject to changeCPC practice application components (1/4)HIGHLY PRELIMINARY1. For which Track is your practice applying (1 / 2)2. If you are a Track 2 applicant but are not eligible for Track 2, would you like your applicationconsidered for Track 1? (Y/N)APreliminaryQuestions3. Is your practice a concierge practice, a Rural Health Clinic, or a Federally Qualified Health Clinic(Y/N) [Disqualifier]4. Is your practice currently participating in any of the Medicare initiatives that follow? Please check allthat apply– TCPi, Pioneer ACO, Next Generation ACO, MSSP ACO, another Medicare ACO, AccountableHealth Communities, None, participates but plans to withdraw5. Practice identification questions (e.g., name, ownership, belonging to larger system, satellite office)PracticeStructureBandOwnership6. Does practice share a TIN for billing with other practices in the same health system7. Does practice use more than one billing TIN?8. What billing TIN will practice use?9. Who owns the practice [physicians, other practitioners, another physician organization, hospital,health plan, medical school, other]10. Has practice participated in CPCi (Y/N)? If so, what was practice ID?ModelC Participation11. Has practice participated in MPAPCP (Y/N)? If so, what was practice ID?12. Primary contract information13. Secondary contact information14. HIT contactSource: CPC RFAConfidential and Proprietary 19
Preliminary pre-decisional working draft; subject to changeCPC practice application components (2/4)HIGHLY PRELIMINARYPractitionerD and staffinformation15. To the best of your knowledge, has your practice or anyone employed in your practice had a finaladverse legal action (Y/N)?16. What is the total number of individual physicians, nurse practitioners, physician assistants, andclinical nurse specialists who provide patient care?17. Of the total individual practitioners that provider care at your patient site, how many are primary carepractitioners?18. Are all of the PCPs applying to be a part of CPC in the same physical address?19. For each PCP in your office, please provide the following identifying information20. Please describe the current Meaningful Use attestation progress including: total Medicare andMedicaid eligible practitioners (EPs); total number of Medicare and Medicaid EPs who plan to attestto MU Stage 2Practiceactivities21. Which statement best characterizes your practice: single-specialty primary care; multi-specialtypractice; other LOBs (e.g,. urgent care)22. Is this practice engaged in training future practitioners and staff (Y/N). Please briefly describe theengagement23. The practice is recognized as a “medical home” by: NCQA, TJC, AAAHC, URAC, State-based, Planbased, Other, NoneEHealthF InformationTechnologySource: CPC RFA24. Is your practice able to complete HIT requirements indicated for the track for which it is applying?(Y/N)25. Please provide the following information regarding the primary certified EHR system used by yourpractice site (Vendor Name / Product Name / Version)26. Please provide the most up-to-date CMS EHR certification ID for your practice’s certified products27. Please list any other health IT tools or services your practice currently uses (e.g., PHM tools, caremanagement tools, data analytics, services provided by an HIE or data registry) including:(Vendor Name/Product Name/Version/Function)28. Does your practice currently have plans to purchase a new EHR in 2017 or a subsequent year?(Yes/No/Unknown)Confidential and Proprietary 20
Preliminary pre-decisional working draft; subject to changeCPC practice application components (3/4)HIGHLY PRELIMINARYPatientG demographics29. Percent of patients of Hispanic, Spanish, or Latino origin30. Percentage of patients by race (6 races given)31. Percent of patients by preferred language (i.e, English, non-English). If not English, what is the mostcommon languagePracticeH revenue andbudgetPlease list all revenue (insurance and co-pays) generated by services provided to patients covered bythe following payers in 2015. Exclude any bonus payments. Please use your billing system or billingvendor to generate this information.32. Total revenue for 2015 from all LOBs33. Total revenue for 2015 by LOB (options given)34. Percentage of patients by insurance typeICaredeliverySource: CPC RFALevel to which each of the statements below is true [scale of four options provided]35. Patients: Are assigned to specific practitioner panels and panel assignments are routinely used by thepractice for scheduling purposes and are continuously monitored to balance supply and demand36. Non-physician practice team members: Perform key clinical service roles that match their abilities andcredentials37. Track 2 only: Care plans: Are developed collaboratively, include self-management and clinicalmanagement goals, are routinely recorded, and guide care at every subsequent point of service38. Track 2 only: A standard tool or method to stratify patients by risk level is available, consistently usedto stratify all patients, and is integrated into all aspects of care delivery39. Follow up by the primary care practice with patients seen in the ED or hospital is done routinelybecause the primary care practice has arrangements in place with the ED and hospital to both trackthese patients and ensure that follow-up is completed within a few days40. Track 2 only: Linking patients to supportive community-based resources is accomplished throughactive coordination between the health system, community service agencies, and patients andaccomplished by a dedicated staff personConfidential and Proprietary 21
Preliminary pre-decisional working draft; subject to changeCPC practice application components (4/4)HIGHLY PRELIMINARYLevel to which each of the statements below is true [scale of four options provided]J AccessQualityK improvement41. Patient after-hours service (24 hours, 7 days a week) to a physican, PA/NP, or nurse: Is available viathe patient’s choice of e-mail or phone directly with the practice team or a practitioner who has realtime access to the practice’s EMR42. Quality improvement activities: Are based on a proven improvement strategy and used continuouslyin meeting organizational goals43. Staff, resources, and time for quality improvement activities: Are all fully available in the pracitce1. Clinical leadershipLetters ofsupportSource: CPC RFA2. Parent of owner organization3. Support from HIT vendor (Track 2 only)Confidential and Proprietary 22
Next StepsOhio Department of Medicaid: Communicate status of statewide payer CPC application andannounce whether CMS selects Ohio as a CPC region in late July Share Ohio-specific provider application template Assist in answering questions regarding the application asnecessary, and communicate questions/concerns to CMSMonica.Juenger@governor.ohio.govPrimary Care Practices: Begin soliciting letters of support Become familiar with the application so you are ready to applywhen it is announced that Ohio is a CPC region
CPC Year 1 (CMS-selected) Year 2 (CMS-selected) Year 3 5 (CMS-selected) Year 1 (early entry) Design Ohio's SIM-sponsored PCMH model Ongoing Enrollment into the Ohio CPC Model Any practice with 500 Medicaid members that meets Ohio CPC activity, efficiency and clinical quality requirements Medicare-sponsored Payers apply .