Transcription
Research ArticleTrends in Deep Vein ThrombosisProphylaxis and Deep VeinThrombosis Rates After Total Hipand Knee ArthroplastyAbstractHarpreet Bawa, MDJack W. Weick, MDDouglas R. Dirschl, MDHue H. Luu, MDFrom the Department of OrthopaedicSurgery and Rehabilitation Medicine,University of Chicago Medicine andBiological Sciences, University ofChicago Medical Center, Chicago, IL.Correspondence to Dr. Bawa:harpreetbawa@gmail.comDr. Dirschl or an immediate familymember serves as a paid consultantto Bone Support and Stryker andserves as a board member, owner,officer, or committee member of theAmerican Orthopaedic Association,the Foundation for OrthopaedicTrauma, and the Orthopaedic TraumaAssociation. Dr. Luu or an immediatefamily member serves as a paidconsultant to DePuy Synthes andStryker and serves as a boardmember, owner, officer, or committeemember of the American OrthopaedicAssociation and the MusculoskeletalTumor Society. Neither of thefollowing authors nor any immediatefamily member has received anythingof value from or has stock or stockoptions held in a commercial companyor institution related directly orindirectly to the subject of this article:Dr. Bawa and Dr. Weick.J Am Acad Orthop Surg 2018;26:698-705DOI: 10.5435/JAAOS-D-17-00235Copyright 2018 by the AmericanAcademy of Orthopaedic Surgeons.698Introduction: Patients undergoing total hip arthroplasty (THA) andtotal knee arthroplasty (TKA) are at high risk of deep vein thrombosis(DVT) postoperatively, necessitating the use of prophylaxismedications. This investigation used a large claims database toevaluate trends in postoperative DVT prophylaxis and rates of DVTwithin 6 months after THA or TKA.Methods: Truven Health MarketScan Commercial Claims andEncounters and Medicare Supplemental and Coordination of Benefitsdatabases were reviewed from 2004 to 2013 for patients whounderwent THA or TKA. Data were collected on patient age, sex,Charlson Comorbidity Index, and hypercoagulability diagnoses.Postoperative medication claims were reviewed for prescribed aspirin,warfarin, enoxaparin, fondaparinux, rivaroxaban, and dabigatran.Results: A total of 369,483 patients were included in the analysis, ofwhich 239,949 patients had prescription medication claims. Warfarinwas the most commonly prescribed anticoagulant. Patients with ahypercoagulable diagnosis had markedly more DVTs within 6 monthsafter THA or TKA. More patients with a hypercoagulable diagnosiswere treated with warfarin or lovenox than other types ofanticoagulants. A multivariate regression analysis was performed,showing that patients prescribed aspirin, fondaparinux, andrivaroxaban were markedly less likely than those prescribed warfarinor enoxaparin to have a DVT within 6 months after THA or TKA.Conclusion: After THA and TKA, warfarin is the most commonlyprescribed prophylaxis. Patients with hypercoagulability diagnosesare at a higher risk of postoperative DVT. The likelihood of DVT within6 months of THA and TKA was markedly higher in patients treated withwarfarin and lovenox and markedly lower in those treated with aspirin,fondaparinux, and rivaroxaban.Level of Evidence: Level IIIMore than 1 million total hiparthroplasty (THA) and totalknee arthroplasty (TKA) proceduresare performed in the United Stateseach year.1 Patients undergoing theseprocedures are at an increased riskof thromboembolic complications.2–4The most common complication isdeep vein thrombosis (DVT) becausepatients are placed at a higher riskas a result of venous stasis withleg positioning, increased risk ofJournal of the American Academy of Orthopaedic SurgeonsCopyright ª the American Academy of Orthopaedic Surgeons. Unauthorized reproduction of this article is prohibited.
Harpreet Bawa, MD, et alendothelial injury, and aberrant activation of the clotting cascade.4,5Prophylaxis after THA and TKA isrecommended by both the AmericanAcademy of Orthopaedic Surgeonsand American College of Chest Physicians; however, no consensus exists onthe optimal prophylactic regimen.6Anticoagulation after THA or TKAcan pose unique challenges becauseanticoagulation medications must balance the reduction in blood clot formation, with the risk of postoperativebleeding, hematoma formation, revision surgery, and infection.7-10 Thevitamin K antagonist warfarin has beenshown to be effective in reducing therate of proximal DVTs and pulmonaryembolisms.11,12 The major advantageof warfarin is that it can be reversedif bleeding complications arise orif patients require urgent surgicalintervention.13,14 Warfarin’s mostnotable disadvantage is that it is onlyeffective within a narrow therapeuticwindow, necessitating frequent laboratory monitoring and dose adjustments. These drawbacks have ledto the use of alternative methods ofchemoprophylaxis.Recent studies have demonstrated theeffectiveness of aspirin prophylaxisafter TKA or THA. In a trial of 13,356patients undergoing THA, low-doseaspirin reduced the rate of DVT by29%, PE by 43%, and fatal pulmonary embolism by 58% comparedwith placebo.15 Low-molecular-weightheparin agents, such as enoxaparin,have also been shown to be effective;however, they must be administeredthrough subcutaneous injection.16Other therapies such as factor Xaand direct thrombin inhibitors areappealing because they can be delivered orally, do not require monitoring, and have constant dosing formost patients. Unfortunately, thisgroup of medications is costly andrequires fresh frozen plasma forreversal.5,17,18Although DVT prophylaxis afterTHA and TKA is assumed to be theFigure 1Flowchart showing the cohort selection. TKA total knee arthroplasty, THA totalhip arthroplastystandard of care, given the high likelihood of thromboembolic eventswithout prophylaxis, a paucity ofdata exists on surgeon practice patterns and changes over time. Inaddition, few studies have evaluatedpostoperative DVT rates by anticoagulants at a large-scale population level. The purpose of thisinvestigation was to use a large claimsdatabase to evaluate trends over timein national practice patterns of postoperative DVT prophylaxis and ratesof DVT within 6 months after THAor TKA procedures.MethodsData SourceA retrospective review was conductedusing the Truven Health MarketScanCommercial Claims and Encounters(commercial insurance) and MedicareSupplemental and Coordination ofBenefits (Medicare with commercialsupplement) databases (Truven HealthAnalytics). The databases containdeidentified, integrated, person-specificclaims data for approximately 17 to 51million individuals per year. The commercial insurance database includeshealthcare claims for individuals withinsurance through a commercial provider or a self-insuring employer underfee-for-service, fully capitated, or partially capitated health plans. TheMedicare with commercial supplementdatabase includes claims informationfor individuals who have both Medicare and commercial employersponsored coverage. All claimsfrom the Medicare with commercialsupplement database reflect the coordination of benefits between the commercial insurer and Medicare such thatall payments made by either entity arecaptured within the database. Theage distribution in the Medicare withcommercial supplement database isrepresentative of the overall Medicarepopulation. These databases, whencombined, constitute approximately20% of the overall insurance market.International Classification of Disease(ICD-9) diagnoses codes and CurrentProcedure Terminology (CPT) codescan be identified in individual claims.The data include claims made fromboth inpatient and outpatient clinicalencounters and prescription medications. National Drug Codes (NDCs)are used to organize prescriptionmedication claims. The NDCs specifyOctober 1, 2018, Vol 26, No 19Copyright ª the American Academy of Orthopaedic Surgeons. Unauthorized reproduction of this article is prohibited.699
Trends in Deep Vein Thrombosis ProphylaxisTable 1Demographics of Patient Deep Vein Thrombosis Prophylaxis After Total Hip Arthroplasty or Total KneeArthroplasty ionClaimAge61.964.962.561.861.370.266.0% .50.9% HypercoagulabilitydiagnosisCCI0.043Percent of totalpopulation .08935.1CCI Charlson Comorbidity IndexTable 2Postoperative Deep Vein Thrombosis Prophylaxis Trends by Drug TypePostoperative MedicationPrescription 0.25%1.39%1.25%1.05%both the type and dosage of the medication prescribed.Study SampleThe databases were reviewed from2004 to 2013 for subjects with a CPTcode for THA (CPT 27,130) or TKA(CPT 27,447). Patients wererequired to be enrolled in the databasecontinuously for 6 months before and6 months immediately after the THAor TKA procedure. Data were collected on patient age and sex. Weidentified a group of patients whowere hypercoagulable, defined assubjects with a previous DVT (ie,ICD-9 code 453.40) or who had anICD-9 code for primary hypercoagulable state (ie, ICD-9 289.81, 289.82,286.53, and 795.79), which includesdiagnoses of factor V leiden, antiphospholipid antibody, lupus antico-700agulant, and protein C/S deficiency.Prescription medication claim information was collected based on NDCson prescribed aspirin, warfarin, enoxaparin, fondaparinux, rivaroxaban,and dabigatran. Patients were excluded if they were on any prescription anticoagulation medications.2 months before the THA or TKAprocedure. In addition, patients withno claims for a prescription anticoagulant are presented as a separategroup. Data were gathered on allanticoagulation prescription claims inthe 6-month period after THA andTKAprocedures. PostoperativeDVTs were identified in the 6 monthsafter THA and TKA procedures usingthe ICD-9 code for DVT (453.40).We excluded any anticoagulationprescription claims that occurredafter a DVT. Charlson ComorbidityIndex (CCI) scores were calculatedfor each subject using ICD-9 codesfor comorbidities, as described inprevious studies.19Statistical AnalysisMean age, percent female, percent ofpopulation with the hypercoagulablegroup, and CCI were calculated foreach type of anticoagulant studied.Trends of utilization by year for eachanticoagulant were compared. Ratesof DVT in the 6-month period afterTHA and TKA were calculated byeach type of prescription anticoagulant using the ICD-9 code for DVT(ie, 453.40). DVT rates by year werealso calculated over the course of thestudy period to analyze trends inDVT rates over time. A best fit linewas used to calculate the R2 valueand statistical significance of theyearly trend.Journal of the American Academy of Orthopaedic SurgeonsCopyright ª the American Academy of Orthopaedic Surgeons. Unauthorized reproduction of this article is prohibited.
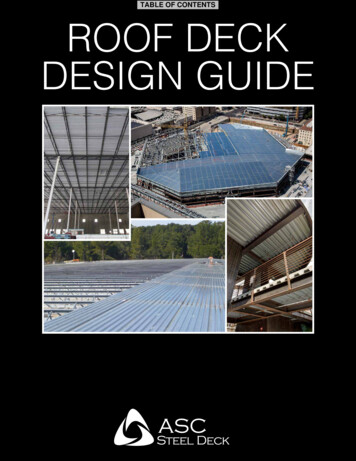
Harpreet Bawa, MD, et alFigure 2Graph showing yearly trends in deep vein thrombosis prophylaxis after total hip arthroplasty and total knee arthroplasty procedures.DVT rates were compared in patients in the hypercoagulable groupversus patients not in the hypercoagulable group using chi-squared tests.All statistical analysis were performedwith SAS software, version 9.3 (SAS).Table 3Deep Vein Thrombosis Rates Within 6 Months of Total Hip Arthroplasty orTotal Knee Arthroplasty Procedures by Drug TypePostoperative AnticoagulationPercent w/DVTPrescription aspirin2.20Warfarin4.74Comparison of Deep VeinThrombosis Rates roxaban1.86Further analysis was conducted toattempt to compare the rate of DVTobserved within 6 months after THA orTKA procedures by the anticoagulanttype after controlling for confoundingvariables. Multivariate logistic regression analysis was performed controllingfor the effects of age, sex, hypercoagulability, and CCI. Odds ratios .1.0signified the increased risk of DVT inrelation to the other forms of prescription anticoagulation studied.Dabigatran3.83No anticoagulation claim2.16ResultsA total of 369,483 patients wereincluded in the analysis, of which239,949 patients had prescriptionanticoagulant information. A flowchart of patient selection is presentedDVT deep vein thrombosisin Figure 1. The average age of thecohort was 66.7 years, 58.7% werefemale, 1.8% were in the hypercoagulable group, 28.3% underwentTHA, and 71.7% underwent TKA.Demographics by anticoagulanttype and for patients without anticoagulation claims are presentedin Table 1. Warfarin was the mostcommonly prescribed anticoagulantwithin the cohort at a rate of 58.44%.At the beginning of the study periodin 2004, 0.03% of patients had claimsfor prescribed aspirin, 75.02% warfa-rin, 25.26% enoxaparin, 2.72% fondaparinux, zero rivaroxaban, and zerodabigatran. Throughout the studyperiod, the most notable changesincluded a decrease in warfarin claimsand increase in rivaroxaban claims.In 2013, 2.19% of patients had claimsfor prescribed aspirin, 41.17% warfarin, 24.63% enoxaparin, 2.15% fondaparinux, 33.58% rivaroxaban, and1.05% dabigatran. The prescriptionmedication claims per year are presented in Table 2. Figure 2 demonstrates the change in postoperativeOctober 1, 2018, Vol 26, No 19Copyright ª the American Academy of Orthopaedic Surgeons. Unauthorized reproduction of this article is prohibited.701
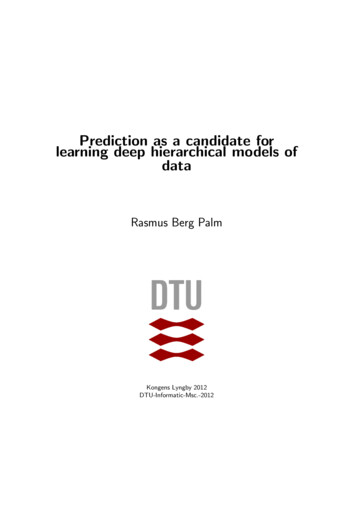
Trends in Deep Vein Thrombosis ProphylaxisTable 4Deep Vein Thrombosis Rate Within 6 Months After Total Hip Arthroplasty or Total Knee Arthroplasty Procedures by nual DVT .21%DVT deep vein thrombosisFigure 3Graph showing the annual rate of deep vein thrombosis within 6 months aftertotal hip arthroplasty and total knee arthroplasty procedures.Table 5Deep Vein Thrombosis Rates Within 6 Months of Total Hip Arthroplasty orTotal Knee Arthroplasty Procedures Based on Hypercoagulable DiagnosisPostoperativeAnticoagulationPrescription aspirinHypercoagulableDiagnosis*No abigatran0.47%0.32%0.05No anticoagulation claim18.54%35.35%,0.001Overall DVT rate24.30%2.50%,0.001DVT deep vein thrombosis*Hypercoagulable Dx: history of factor V Leiden, antiphospholipid antibody, lupus anticoagulant,hypercoagulable state, or previous DVT in database.DVT prophylaxis drug prescriptionsover the study period time.DVT rates in patients within6 months after THA or TKA procedures were calculated and are presented in Table 3. DVTs were recordedin 2.20% of patients with claims forprescribed aspirin, 4.74% for warfa-702rin, 3.73% for enoxaparin, 2.69% forfondaparinux, 1.86% for rivaroxaban, 3.83% for dabigatran, and2.17% for those patients with nopostoperative anticoagulation claims.DVT rates within 6 months after THAor TKA for each year during the studyperiod were calculated (Table 4).Figure 3 is a graph demonstrating thatno significant change in DVT rateswas observed over the study period(P 0.07; r2 0.41).A subanalysis was performedcomparing postoperative DVT rateswithin 6 months after THA or TKAprocedures in the hypercoagulablegroup versus the remainder of thecohort. Patients in the hypercoagulable group had significantly moreDVTs within 6 months after THA orTKA procedures compared with theremainder of the cohort (24.30%versus 2.5%; P , 0.001) (Table 5). Inaddition, a significantly greaterproportion of patients in the hypercoagulable group were treated withwarfarin (64.3% in the hypercoagulable group versus 37.5% in theremainder of the cohort, P , 0.001)or lovenox (34.8% in the hypercoagulable group versus 20.6% in theremainder of the cohort, P , 0.001).A multivariate regression analysiswas performed, adjusting for age, sex,hypercoagulability, and CCI, comparing each type of anticoagulation to theothers (Table 6). The adjusted analysisshowed patients on prescribed aspirin(odds ratio: 0.69, 95% confidenceinterval, 0.49–0.96), fondaparinux(odds ratio: 0.85, 95% confidenceinterval, 0.76–0.95), and rivaroxaban(odds ratio: 0.57, 95% confidenceinterval, 0.51–0.63) were markedlyless likely to have a DVT within6 months after THA or TKA procedures when compared individually topatients who were treated with allother types of DVT prophylaxis. Patients on warfarin (odds ratio: 3.60,95% confidence interval, 3.38–3.84)and enoxaparin (odds ratio: 1.14,Journal of the American Academy of Orthopaedic SurgeonsCopyright ª the American Academy of Orthopaedic Surgeons. Unauthorized reproduction of this article is prohibited.
Harpreet Bawa, MD, et al95% confidence interval, 1.09–1.20)were markedly more likely to have aDVT when compared individually toall other forms of anticoagulationduring the 6 months after THA orTKA procedures (Table 6).Table 6Odds Ratio of Deep Vein Thrombosis Within 6 Months of Total HipArthroplasty or Total Knee Arthroplasty Procedure by Anticoagulant TypeAdjusted for Age, Sex, Hypercoagulability Diagnosis, and CharlsonComorbidity IndexOdds Ratio95% ConfidenceInterval (Lower, Upper)Prescription aspirin0.690.49, 0.96Warfarin3.603.38, 3.84Enoxaparin1.141.09, 1.20Fondaparinux0.850.76, 0.95Rivaroxaban0.570.51, 0.63Dabigatran1.090.80, 1.47Postoperative MedicationConclusionPatients are in a hypercoagulable stateafter THA and TKA procedures.2-4,20DVT after an elective procedure suchas a THA or TKA can have seriousramifications including pulmonaryembolism and, in extreme situations,death. Variation exists in the AmericanAcademy of Orthopaedic Surgeonsand American College of ChestPhysicians recommendations on optimal postoperative anticoagulationmanagement of these patients.6 Consequently, physician preference andclinical decision making are theprimary determinants of a patient’spostoperative anticoagulant selection.This investigation demonstrated thechanges between year 2004 and year2013 in surgeon preference for postoperative DVT prophylaxis in patients undergoing THA and TKAprocedures. Limiting the study to thisperiod allowed this investigation toobtain a large sample size and observethe changes in practice patterns seenwith the introduction of novel postoperative DVT prophylaxis agents.During the study period, a notabledecrease was observed in patients prescribed warfarin and an increase seenin patients prescribed rivaroxaban.During the same period, no statisticallysignificant change was noted in theoverall DVT rates in the 6 months afterTHA or TKA. Patients with a hypercoagulable diagnosis had markedlyhigher rates of DVT within 6 monthsof a THA or TKA procedure comparedwith those patients without hypercoagulable diagnosis. No other clinicallysignificant risk factors were identifiedto distinguish patients at a high risk ofDVT. Furthermore, a greater portionof patients with hypercoagulable diagnosis were treated with warfarin andlovenox (Table 5).Vitamin K antagonists such as warfarin pose a variety of challenges,which have likely contributed to itsdecreasing popularity. Patients mustbe closely monitored to ensure thattheir international normalized ratio(INR) is within the therapeutic range.If the INR is above or below thetherapeutic range, patients will haveto adjust their doses accordingly. Inaddition, dietary changes can influence the metabolism of the drugsubsequently affecting the overalleffectiveness and influence on theINR.14,21 Warfarin has been classically considered to be relatively lowcost; however, after taking intoaccount the cost of laboratory monitoring, the overall cost of warfarinprophylaxis has been shown to actually be greater than prophylaxiswith low-molecular-weight heparin.22 However, warfarin providesthe greatest advantage over othertypes of anticoagulant because it canbe readily reversed if bleeding oranticoagulation-relatedcomplications arise. Newer medications, suchas factor Xa inhibitors and directthrombin inhibitors are attractivesolutions because they can be administered orally, do not requirelaboratory monitoring, and havepredictable pharmacokinetics irre-spective of body mass or diet.23,24Downsides of these medicationsinclude cost and the only option toreverse the drug with fresh frozenplasma if bleeding complicationsarise; however, studies have shownno increase in wound complicationand thromboembolic rates in factorXa inhibitors compared with otherforms of anticoagulation.25Aspirin is appealing because of itslow cost, oral administration, predictable pharmacokinetics, and easyaccess over the counter. A recent metaanalysis showed that patients undergoing THA or TKA did not have anydifference in proximal DVT risk whencomparing aspirin versus other anticoagulants.26 However, this analysisincluded studies, which performedscreening for DVT on all patients; thispractice is neither practical nor recommended.5,6,11 In this investigation,information was collected on prescribed aspirin claims. The number ofpatients taking aspirin as the primaryprophylaxis after TKA and THAmay be higher than reported in thisinvestigation because this drug is alsoavailable without a prescription. Ina subanalysis, we included data on129,505 patients who did not haveany prescription anticoagulant. Thiscohort did not have markedly higherDVT rates within 6 months ofTHA or TKA procedures comparedwith prescription anticoagulants. ItOctober 1, 2018, Vol 26, No 19Copyright ª the American Academy of Orthopaedic Surgeons. Unauthorized reproduction of this article is prohibited.703
Trends in Deep Vein Thrombosis Prophylaxisis possible that these patientswere taking over-the-counter anticoagulants; however, this cannot beconfirmed with the available data.The study found markedly increasedDVT rates in the 6 months after THAand TKA procedures in patients treatedwith warfarin (odds ratio: 3.60, 95%confidence interval, 3.38–3.84) andenoxaparin (odds ratio: 1.14, 95%confidence interval, 1.09–1.20). Theexact reason for the increased DVTrate in this subgroup cannot bedetermined from this study andbeyond the scope of this investigation.This study focused on claims information and did not have anyinformation on INR levels or patientcompliance. Studies have demonstrated that patients are within thetherapeutic range only 45.9% of thetime postoperatively.27 Enoxaparinis administered subcutaneously andprovides challenges inherent to people hesitant to administer the drugon themselves; however, this hasnot been shown to prevent compliance.28 It is unclear whether the increased rate of DVT observed is dueto failure of patient compliance oranother confounding variable unaccounted for in the regression model.Importantly, the results in thisstudy represent the actual observedpopulation-level rates over a decadeof time with the use of various prophylactic regimens. Consequently,these findings are informative toboth surgeons and patients as to theexpected population rates of DVT.This study has limitations inherentto any retrospective review. Thedatabase is likely to represent a representative sample of the overall population but does not include patientswithout insurance or on Medicaid.The information in the database islimited to the specified time; however,this provides the benefit of a largesample size. Patients who did not havemedication claims data were alsoexcluded from this analysis. Medications that were obtained over the704counter were also not captured by thedatabase. Patient compliance withmedications could not be determinedfrom our data because the usualcourse of anticoagulants prescribedafter a THA or TKA is too briefto calculate medication possessionratios.Overall, this investigation demonstrates, at a population level, recenttrends in DVT prophylaxis afterTHA and TKA procedures. Althoughwarfarin is still the most commonlyprescribed prophylaxis after THAand TKA procedures, use of thisagent is decreasing. Patients with ahistory of DVT or hypercoagulabilityare at a higher risk of postoperativeDVT, regardless of the type ofprophylaxis prescribed. After adjusting for age, sex, and hypercoagulability diagnosis, the likelihoodof DVT within 6 months of THAand TKA procedures was markedlyincreased in patients treated withwarfarin and lovenox and markedlydecreased in those treated with aspirin, fondaparinux, and rivaroxaban.Given the sample size of the dataover a prolonged period in the actualobserved clinical setting, this information is useful for surgeons whencounseling their patients on the different types of anticoagulants available before undergoing THA or TKAprocedures.ReferencesReferences printed in bold type arethose published within the past 5 years.1. Maradit Kremers H, Larson DR, Crowson CS,et al: Prevalence of total hip and kneereplacement in the United States. J Bone JointSurg Am 2015;97:1386-1397.2. Visuri T, Pulkkinen P, Paavolainen P,Koskenvuo M, Turula KB: Causes of deathafter hip arthroplasty in primary arthrosis.J Arthroplasty 1997;12:397-402.3. Harris WH, Sledge CB: Total hip and totalknee replacement. N Engl J Med 1990;323:801-807.4. Sculco T, Colwell C, Pellegrini V, Westrich G,Bottner F: Prophylaxis against venousthromboembolic disease in patients having atotal hip or knee arthroplasty. J Bone JointSurg 2002;84:466-477.5. Falck-Ytter Y, Francis CW, Johanson NA,et al: Prevention of VTE in orthopedicsurgery patients: Antithrombotic Therapyand Prevention of Thrombosis, 9th ed:American College of Chest PhysiciansEvidence-Based Clinical PracticeGuidelines. Chest 2012;141:e278S-e325S.6. Eikelboom JW, Karthikeyan G, Fagel N,Hirsh J: American Association ofOrthopedic Surgeons and AmericanCollege of Chest Physicians guidelines forvenous thromboembolism prevention in hipand knee arthroplasty differ: What are theimplications for clinicians and patients?Chest 2009;135:513-520.7. Barrack RL: Current guidelines for totaljoint VTE prophylaxis: Dawn of a new day.J Bone Joint Surg Br 2012;94:3-7.8. McDougall CJ, Gray HS, Simpson PM,Whitehouse SL, Crawford RW, Donnelly WJ:Complications related to therapeuticanticoagulation in total hip arthroplasty.J Arthroplasty 2013;28:187-192.9. Parvizi J, Ghanem E, Joshi A, Sharkey PF,Hozack WJ, Rothman RH: Does“excessive” anticoagulation predispose toperiprosthetic infection? J Arthroplasty2007;22:24-28.10. Pulido L, Ghanem E, Joshi A, Purtill JJ,Parvizi J: Periprosthetic joint infection: Theincidence, timing, and predisposing factors.Clin Orthop Relat Res 2008;466:1710-1715.11. Johanson NA, Lachiewicz PF, Lieberman JR,et al: American Academy of OrthopaedicSurgeons Clinical Practice guideline on:Prevention of symptomatic pulmonaryembolism in patients undergoing total hip orknee arthroplasty. J Bone Joint Surg Am2009;91:1756-1757.12. Francis CW, Pellegrini VD Jr, Marder VJ,et al: Comparison of warfarin and externalpneumatic compression in preventionof venous thrombosis after total hipreplacement. JAMA 1992;267:2911-2915.13. Nam D, Sadhu A, Hirsh J, Keeney JA,Nunley RM, Barrack RL: The use ofwarfarin for DVT prophylaxis followinghip and knee arthroplasty: How often arepatients within their target INR range? JArthroplast 2015;30:315-319.14. Aynardi M, Brown PB, Post Z, Orozco F,Ong A: Warfarin for thromboprophylaxisfollowing total joint arthroplasty: Arepatients safely anti-coagulated? JArthroplasty 2013;28:1251-1253.15. Prevention of pulmonary embolismand deep vein thrombosis with lowdose aspirin: Pulmonary embolismprevention (PEP) trial. Lancet 2015;355:1295-1302.Journal of the American Academy of Orthopaedic SurgeonsCopyright ª the American Academy of Orthopaedic Surgeons. Unauthorized reproduction of this article is prohibited.
Harpreet Bawa, MD, et al16. Colwell CW, Hardwick ME: Rationale forlow-molecular-weight heparin prophylaxisafter total knee arthroplasty. Clin OrthopRelat Res 2006;452:181-185.17. Stewart DW, Freshour JE: Aspirin for theprophylaxis of venous thromboembolicevents in orthopedic surgery patients: Acomparison of the AAOS and ACCPguidelines with review of the evidence. AnnPharmacother 2013;47:63-74.18. Colwell CW: Managing thromboembolicrisk in hip and knee arthroplasty: State ofthe art. Orthopedics 2003;26:S231-S236.19. Quan H, Sundararajan V, Halfon P,et al: Coding algorithms for definingcomorbidities in ICD-9-CM and ICD-10administrative data. Med Care 2005;43:1130-1139.20. Warwick D, Williams MH, Bannister GC:Death and thromboembolic disease aftertotal hip replacement: A series of 1162 caseswith no routine chemical prophylaxis. JBone Joint Surg Br 1995;77:6-10.21. Asnis PD. Gardner MJ, Ranawat A,Leitzes AH, Peterson MGE, Bass AR: Theeffectiveness of warfarin dosing from anomogram compared with house staffdosing. J Arthroplasty 2007;22:213-218.22. Caprini JA, Botteman MF, Stephens JM,et al: Economic burden of long-termcomplications of deep vein thrombosis aftertotal hip replacement surgery in the UnitedStates. Value Health 2003;6:59-74.23. Sobieraj DM, Coleman CI, Tongbram V,et al: Comparative effectiveness of lowmolecular-weight heparins versus otheranticoagulants in major orthopedic surgery:A systematic review and meta-analysis.Bone 2012;51:376-382.24. Kinov P, Tanchev PP, Ellis M, Volpin G:Antithrombotic prophylaxis in majororthopaedic surgery: An historical overviewand update of current recommendations.Int Orthop 2014;38:169-175.25. Kim SM, Moon YW, Lim SJ, Kim DW,Park YS: Effect of oral factor Xa inhibitorand low-molecular-weight heparin onsurgical complications following total hiparthroplasty. Thromb Haemost 2016;115:600-607.26. Drescher FS, Sirovich BE, Lee A,Morrison DH, Chiang WH, Larson RJ:Aspirin versus anticoagulation forprevention of venous thromboembolismmajor lower extremity orthopedicsurgery: A systematic review andmeta-analysis. J
medications. This investigation used a large claims database to evaluate trends in postoperative DVT prophylaxis and rates of DVT within 6 months after THA or TKA. Methods: Truven Health MarketScan Commercial Claims and Encounters and Medicare Supplemental and Coordination of Benefits databases were reviewed from 2004 to 2013 for patients who