Transcription
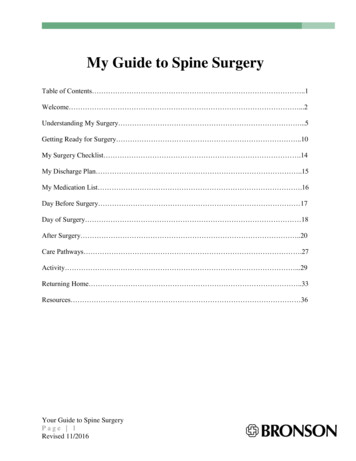
My Guide to Spine SurgeryTable of Contents .1Welcome .2Understanding My Surgery .5Getting Ready for Surgery .10My Surgery Checklist .14My Discharge Plan .15My Medication List .16Day Before Surgery 17Day of Surgery 18After Surgery .20Care Pathways .27Activity .29Returning Home .33Resources 36Your Guide to Spine SurgeryPage 1Revised 11/2016
Welcome!Thank you for choosing Bronson for yourspine surgery. When you or a loved onesuffers from pain, numbness, or weaknesssimple daily activities can be hard to do.Bronson’s approach to spine care is focusedon you, the patient. We will partner with youand your family to set and meet realistic goalsand get you on the way to recovery.Use this book as a guide to help get ready foryour surgery and healing after surgery. Thisbook covers many different types of back orspine problems. Talk to your surgeon or officestaff person if you have any questions aboutyour condition.Your Guide to Spine SurgeryPage 2Revised 11/2016
Below are some questions that will help you better understand your surgery and recoveryprocess. Talk about these questions with your surgeon and healthcare team before your surgeryso you can best prepare for your recovery.1. What surgery am I having?2. What goals does my doctor have with this surgery (relieve pinched nerve, stop abnormalmotion)?3. What goals do I have after surgery (play golf, walk with less pain)?4. How many days (if any) will I be in the hospital?5. How long will it be before I can return to my normal activities (work, hobbies, driving,etc.)?6. What can I do to help with my recovery (weight loss, exercise, quit smoking, etc.)?7. What other questions do I have before surgery?Your Guide to Spine SurgeryPage 3Revised 11/2016
Recovery is a journey. You will face manynew challenges in the days and weeks ahead.We hope this book will be helpful to you.Bring it with you to your office appointmentsand to the hospital. If you have any questionsalong the way, feel free to ask anyone on yourhealthcare team.Bronson Neuroscience Center(269) 341-7500Dr. Alain FabiDr. Chris SlofferDr. Daryl WarderDr. Greg WigginsBronson Spine & Scoliosis Specialists(269) 488-8355Dr. Josh EllwitzDr. Michael KastenWMed Orthopaedics(269) 337-6200Dr. Karen BovidYour Guide to Spine SurgeryPage 4Revised 11/2016
Understanding my surgeryParts of the spineYour spine is made up of vertebrae (bones),discs (shock absorbers), nerves and the spinalcord. Your muscles, ligaments and tendonssupport these structures. They give your spineits normal curve. This allows you to bend androtate. It is important that you understandwhich area of your spine is causing youtrouble. Your surgery is being done to helpyour problem.Images used with permission from Mosby’s NursingConsult and Access Medicine 2013.Your Guide to Spine SurgeryPage 5Revised 11/2016
The normal spine can move in six ways Flexion – forward bending Extension – backward bending Side Bending – bending to the left and right Rotation – twisting left and rightYour Guide to Spine SurgeryPage 6Revised 11/2016
Problems with the curve ofthe spineThe spine has a normal curve. The picture to theright is a side view of a normal spine curve.Sometimes an abnormal curve develops that cancause problems. You might have troublestanding up straight. You may not be stablewhen standing. You may have pain. It can alsocause problems with breathing and digestion.Surgery with the use of rods and screws canhelp to return the spine to a more normal curve.Complete correction may not be possible in allcases. One of the most common abnormalcurves of the spine is scoliosis.Your Guide to Spine SurgeryPage 7Revised 11/2016
Problems with bonesBones in the spine can break(fracture) due to accidents, thindown over time or form cancer ofthe bones. Some fractures cancause weakness within the spineand pain. Surgery can help tostrengthen your spine. This maylessen your pain.FracturedVertebral BodyYour Guide to Spine SurgeryPage 8Revised 11/2016
Problems with discsBulging or herniated discs can cause pain,numbness, tingling or weakness because thedisc pushes on the nerves leaving the spine.Surgery can remove the part of the disc that ispushing on the nerve, which may help relievethese problems.Degenerative disc disease can causediscomfort. As the discs in your spine weardown over time, they lose their “shockabsorbing” function. Sometimes this causesthe bones to over grow (bone spurs). As thespace between the bones becomes smaller,this may cause nerves to be pinched.Your Guide to Spine SurgeryPage 9Revised 11/2016
Getting Ready for SurgeryWe want you to have the best outcome after your surgery. This begins now. Preparing your mind,your home and your body will make your recovery a smoother one. Spine CampYour doctor wants you to attend thislive, pre-surgery education class. Classis offered every week. A registerednurse and occupational therapist willguide you through the surgery processand answer your questions. Bring afamily member or support person withyou to class. Light refreshments areprovided. Choose a CoachSpine surgery is a journey and havingsomeone to support you during this time isvery important. Your coach can be anyoneyou choose that will encourage you, help you,and be your cheerleader. Your coach shouldbe someone who is available to assist youafter you leave the hospital.Your Guide to Spine SurgeryPage 10Revised 11/2016
Directions to Spine Camp:1. Park in the Vine Street Parking Ramp.2. Enter Bronson Methodist Hospital. Insidethe entrance, take the elevator to your rightto the 1st floor (if you’re not already on thefirst floor).3. As you exit the elevator, turn right andreport to the front entrance of the BronsonNeuroscience Center. Check in at thereception desk.Your Guide to Spine SurgeryPage 11Revised 11/2016If you are asked to go to Outpatient Testingafter Spine Camp:4. Exit the Conference Room from the backentrance and walk toward the GardenAtrium.5. With the Gift Shop at your left and tops ofthe trees below on your right, OutpatientTesting will be straight ahead.6. Outpatient Testing entrance.
Pre-Surgery Testing and AppointmentsWe want to make sure you are as healthy as possible before surgery. We require patients to havetests completed. These typically include a blood and urine sample and electrocardiogram (EKG).Depending on your medical history, risk factors and type of surgery we may schedule anappointment with Bronson’s Internal Medicine Hospital Specialists. If necessary, we can alsoschedule appointments with heart and lung doctors. In rare cases, for your safety, your surgerymay need to be rescheduled or canceled due to a medical reason. If this happens, your healthcareteam will work with you to explore other options.Your Guide to Spine SurgeryPage 12Revised 11/2016
Positive AttitudeNo matter how long you’ve had pain ornumbness, it can affect the way you deal withevery day stress. Your pain may have kept youfrom doing the things you enjoy in life. Youmay have gone through weeks of physicaltherapy or pain injections and still have norelief. You may feel hopeless and willing to tryanything. You may say: “Will I ever getbetter?” or “It’s not fair!” All of these feelings are normal. Now you may be thinking: “Is this going to work?” Spine surgery is not a magic cure. Your doctor will be very honest with you on hisexpectations of your surgery. The road ahead is going to be challenging. Recovery will take a lot of hard work. Little bylittle you will see improvements. Try to set small goals (i.e., walking ½ mile). Once you reach that goal, set another. Follow the recommendations of doctor (i.e., quit smoking, lose weight, etc.). Never underestimate the power of a positive outlook! You can do this!Your Guide to Spine SurgeryPage 13Revised 11/2016
My Surgery Checklist Labwork and testing complete Medical clearance appointment date/time: Specialist appointment (cardiology, pulmonology, etc.)date/time: Spine Camp attendance date: I will receive a call from a Bronson Pre-AdmissionCenter nurse (269) 341-7940 I will receive a call from Bronson Registration. Discuss Advanced Directives, Power of Attorney, and/or Living Will options with my family. Discuss my Discharge Plan with my family and friends (see next page). QUIT SMOKING! Smoking is known to cause problems healing after surgery. For the bestoutcome after surgery and my overall health, I must quit smoking! Surgery date/time: Arrive at: am/pmYour Guide to Spine SurgeryPage 14Revised 11/2016
My Discharge PlanName of my coach: Name of the person giving me a ride home from surgery: Purchase groceries and prepare meals in advance for my return Arrange help with childcare, adults I care for, and/or pets Arrange for assistance with driving, errands, and heavyhousehold chores Remove any trip hazards around my home (rugs, cords) and moveitems to places I can easily reach them (If I work) Notify my employer and complete any FMLA or short-term disability paperwork Am I worried about leaving the hospital safely?BEFORE SURGERY please call Bronson Spine Nurse Navigator (269) 341-7142 or CaseManagement (269) 341-7943 for assistance planning your discharge.Your Guide to Spine SurgeryPage 15Revised 11/2016
My MedicationsUse this page to list all of the medicines you are currently taking, including over-the-counter. Alsoinclude vitamins, supplements and herbal medicines. A nurse from Bronson’s Preadmission Centerwill call you to review this list and your medical history about one to two weeks before surgery.MedicineDoseHow often?What is it for?OK to takemorning ofsurgery?Stop thismedicine?My allergies:Your Guide to Spine SurgeryPage 16Revised 11/2016
The Day Before SurgeryIt is important to follow these directions. They are for your safetyand can help you have a better result after surgery. No food after midnight the night before surgery. If yourstomach is not empty you may vomit when we put in thebreathing tube. The vomit could get into your lungs. Thismay cause pneumonia or death. No smoking 24 hours before surgery. Smoking makes itharder for you to heal. Call your doctor if you have a sore throat, fever or cold. Sleep in fresh, clean sheets. Do not sleep with your pet. Take a shower the night before surgery, but DO NOTshave the area of your surgery. This helps preventinfection.Your Guide to Spine SurgeryPage 17Revised 11/2016
Day of Surgery Plan to leave your home with plenty of time to get to the hospital on time. Typically youwill be asked to arrive between 2 and 2 ½ hours before your scheduled surgery time. You may have clear liquids AS INSTRUCTED before your surgery. Clear liquids areliquids you can see through (black coffee, tea, juice, sports drinks, etc). The staff will tellyou when to stop drinking clear liquids before surgery. Wear comfortable, loose fitting clothing. Do not wear makeup or nail polish. Leave money, jewelry and valuables at home. Bring a photo ID and insurance card. Bring eyeglasses and/or denture case. Bring your continuous positive airway pressure (CPAP) machine, if you use one. Bring a copy of your Advanced Directives. If you bring an overnight bag, please leave it in your car until you are taken to yourinpatient room.Your Guide to Spine SurgeryPage 18Revised 11/2016
Arriving for surgeryPlease report to the Inpatient Surgery on the second floor of the West Pavilion. When you check in at the desk, you mayreceive a pager. Staff will use the pager tocommunicate with you and yourfamily/coach. A staff member will bring you back to thepre-op room. This is where you will changeinto a patient gown. You will meet with the anesthesiologist.He/she will talk with you and answer anyquestions you may have about anesthesia. A nurse will start your IV and you mayreceive medicine to make you morecomfortable before surgery. Once you are prepared for surgery, yourfamily may join you in your room until it istime for your surgeryYour Guide to Spine SurgeryPage 19Revised 11/2016
After SurgeryAfter your surgery, your doctor will talk with the family and coach about your surgery. You willgo to the Post Anesthesia Care Unit (PACU) torecover. During this critical time, you will beclosely monitored until you wake up and your heartrate, blood pressure and breathing are normal.When you are ready, we will ask your family to joinyou. You will have an intravenous line (IV) inyour arm so you can receive fluids andmedicine. You may have oxygen delivered thru a tube in your nose or a mask. You will have a monitor on your finger to check your oxygen levels. You may have a tube from your surgery site to drain away excess fluid. You will have elastic stockings on your legs to help with circulation. Your doctor will check on you in the recovery room. Due to the medicine used in surgery,you may not remember. The nurses will continue to check on youfrequently and ask you about your pain. If you are discharged from the PACU, youwill be given self-care instructions by aspine surgery team member and the PACUnursing staff. These instructions start onpage 33.Your Guide to Spine SurgeryPage 20Revised 11/2016
Staying in the hospitalAfter you have recovered well enough in the PACU, you will be taken to your room. Your family,coach or visitors can meet you in your hospital room on the Neurovascular Unit (NVU) – 3 West.In some cases, you may need more frequent checks and care after surgery. If this happens, youmay be admitted to an intensive care unit (ICU) such as Surgical Intensive Care Unit (SICU) on 1East or Neurocritical Care Unit (NCCU) on 3 West. Talk to your doctor about his or herexpectations for after surgery.Your Guide to Spine SurgeryPage 21Revised 11/2016
My Care TeamYou have an entire team of healthcare providers dedicated to your recovery: Your surgeon, resident doctors, physicianassistants (PAs) and nurse practitioners (NPs)direct your medical care and will make dailyrounds to check on your recovery progress. Registered nurses (RNs) and patient careassistants (PCAs) will assess you at the bedside,give you medicine, and provide education. Physical therapists are available to evaluate yourneeds and make recommendations for safe mobilityequipment, if needed. Occupational therapists are available if necessaryto evaluate your needs and make recommendationsfor assistive devices for self-care activities, ifneeded.Your Guide to Spine SurgeryPage 22Revised 11/2016
Medical Social Workers can link you and your family to community resources, providefinancial counseling and emotional support. Case Managers will help you put your discharge plan into action. They can assist withordering equipment, outpatient referrals,rehabilitation facility placement anddiscussing your progress with your insurancecompany. Spine Nurse Navigator can visit and helpyou make connections as you transition tooutpatient care. This may include makingappointments or talking with your primarycare doctor and surgeon. The Spine NurseNavigator will also help you and your doctor set reachable goals. She is available by phone andemail to help you and your family navigate recovery after surgery.Your Guide to Spine SurgeryPage 23Revised 11/2016
Managing Pain at the HospitalAs your healthcare team, we want you torecover as quickly as possible. When your painis kept at a reasonable level, you are better ableto perform your daily activities. This helps yourecover faster. Let us know how much pain youare feeling, and ask for pain medicine when youneed it.Setting GoalsThink about your expectations for pain afteryour surgery. You may still have some pain,but the goal should be a level of pain whereyou are able to participate in activities. Beingable to participate in activities speeds yourrecovery.Your Guide to Spine SurgeryPage 24Revised 11/2016
Pain MedicineYour doctor will prescribe different types of pain medicine depending on your pain level, the typeof pain you have and your medical history. Your nurse will give these to you through yourintravenous line (IV) or in pill form. You may also have muscle spasms and cramps after surgeryas the muscles heal. Your doctor may prescribe medicine that can help relax those muscles andmake you more comfortable.Our goal as your healthcare team is to help you meetyour expectations. We want you to be able to enjoygreater comfort while you heal, get enough rest andreturn to your normal level of health as quickly aspossible. Be sure to take your pain medicine at leasta half hour before your therapy session. Treatmentsthat may be used in addition to medicine are:Your Guide to Spine SurgeryPage 25Revised 11/2016 Ice Rest Activity (therapy) Position changes Relaxation and breathing
Preventing Falls in the HospitalFalls can happen anywhere. Please follow theserecommendations to keep yourself safe. Call or ask for help when getting up to go to thebathroom. Wait until someone comes to help you.Getting up the first few times after lying in bed ortaking medicine may cause you to feel dizzy orlightheaded. Get up slowly from the bed or chair to help preventdizziness. Use a walker, crutches, cane or wheelchairif needed. Grasp grab bars in the bathroom. Holdonto handrails in the hall. Keep personal items within easy reach, such aseyeglasses, phone, tissue, water or call button.Use your call button when you need help,especially when you can’t reach things youwant. Wear non-skid socks or slippers. If you do nothave any, ask your nurse for a pair.Your Guide to Spine SurgeryPage 26Revised 11/2016
Example of your Care PathwayThis is an example of what to expect in the days after your surgery:Day of SurgeryFirst Day after SurgeryFollowing DaysI will:I will:I will:Post Use the incentive spirometer Sit in the chair for all meals.Operativeevery hour I am awake taking Use the incentive spirometer every hour I am awake taking in 10Surgicalin 10 breaths each time.breaths each time.Care Do ankle pumps after I use Do ankle pumps after I use my incentive spirometer.my incentive spirometer. Put ice on my incision as needed. Put ice on my incision asneeded.ActivitywithPhysicalTherapyandNursing Get help from staff to sit onthe edge of the bed or get intoa chair. I may walk a short distanceand begin exercises withPhysical Therapy. Avoid BLT as instructed bymy doctor. Participate with PhysicalTherapy. Walk with help and use awalker if needed. Wear clothes from home. Get out of bed or up to thechair with help. Review Spine Camp video inmy room.Diet Start with liquids. If I amtolerating liquids, I willchange to my usual diet. Restart home medicines. Mynurse will give these to me. Receive antibiotics throughmy IV. Begin taking pain medicinesfrom nurses. Have an IV for fluids. Eat my usual diet. Include fresh fruits and vegetables, and foodsmade from whole grains to help prevent constipation. Drink plenty offluids. Set a goal of 6 to 8 cups per day. Continue home medicines Discuss which medications I willgiven to me by my nurses.continue when I leave the hospital. Start to manage my painwith oral pain pills. Start to use an oral stoolsoftener. My IV fluids will be IV will be removed.stopped. The IV may remainin place if needed formedicines. My foley catheter will be Be walking to the bathroom.removed. I will use a bedside Be aware that pain medicines maycommode or walk to thecause constipation and will takebathroom.stool softeners as needed.MedicinesIVBathroom I may have a foley catheter todrain my bladder.Bandageand BloodDrain Have a bandage over my incision(s). I mayhave a tube to drain fluid from my surgery site.DischargePlanning Meet with Case Manager to discuss dischargeneeds, including equipment, medicines, andpossible physical therapy needs.Your Guide to Spine SurgeryPage 27Revised 11/2016 Continue exercises and increasewalking. Practice skills needed for homesuch as stairs, log rolling, and cartransfers. Graduate from Physical Therapy. My bandage and drain will be removed. I may havea new bandage applied. Plan to have someone take me home when I amdischarged.
Patient and Family Activity TrackerUse this tool to track your daily progress as you heal.Day of SurgeryFirst Day After SurgeryFollowing DaysUp to chair or edge of bed with helpUp to chair for mealsUp to chair for mealsWalk (Short distance with nurse orWalksWalksIncentive Spirometer (every hour)Incentive Spirometer (every hour)Incentive Spirometer (every hour)Ankle PumpsAnkle PumpsAnkle PumpsPT)Your Guide to Spine SurgeryPage 28Revised 11/2016
ActivityIn the days following your surgery, you maybe evaluated by the therapy team in thehospital. The physical and occupationaltherapists will focus on safe movements andkeeping you as active as possible within thelimits of your surgery. Log roll in bed Sitting on edge of bed Edge of bed to chair Chair to standing Walking Climbing stairs Dressing yourself Self-care (brushing your teeth,combing your hair) ToiletingDepending on your surgery, your doctor and therapy team may have other recommendations foryou.Your Guide to Spine SurgeryPage 29Revised 11/2016
Log RollThe log-roll is a way to get yourself safely inand out of bed. To get into bed, sit at the edge of thebed. Scoot back as far as you can.Lower yourself onto your side usingyour arms to help guide and controlyour body to avoid twisting. At thesame time, bend your knees and pullyour legs onto the bed. Lower yourself onto your side usingyour arms to help guide and controlyour body (see picture at right). At thesame time, bend your knees and pullyour legs onto the bed. To get out of bed, reverse the process.Log roll to one side, keepingshoulders, hips and knees lined up.Bend your knees and use your arms topush yourself into a seated position.Your Guide to Spine SurgeryPage 30Revised 11/2016
BLT: Bending, Lifting, TwistingYour doctor may ask that you avoid certain movements after your surgery: bending, lifting, andtwisting. The length of time for these restrictions varies depending on your surgery. Ask yourhealthcare team how long you should avoid these movements. NO – Bending at the waist. YES – Use your knees and hips (squat) toreach objects on the floor. about 8 pounds NO – Lifting greater than 10 pounds. NO – Twisting your body (for example, vacuuming) YES – Move your whole body as a unitYour Guide to Spine SurgeryPage 31Revised 11/2016
Leaving the HospitalYour doctor will discharge you from the hospital when you have met certain goals: You can move safely and steadily (with a walker if necessary). Your pain is controlled with medicine you can take by mouth. You do not have any medical problems that will make it hard for you to leave the hospital.If you need help getting stronger before goinghome safely or have a medical condition thatrequires further care, you may still receive carefrom: Inpatient Rehabilitation Skilled Nursing Facility (SNF) Home Health CareThe options available to you depend on yoursurgery, therapy recommendations andinsurance coverage. Ask your Case Manager orNurse Navigator for more information.Your Guide to Spine SurgeryPage 32Revised 11/2016
Returning HomeYou have taken the next step in your journey to recovery by returning home. With goodpreparation and support from your family and coach, you can focus on getting stronger andhealing. It is normal to feel anxious andwell-balanced diet and drinking plentyuncertain about returning home afterof fluids.spine surgery. It’s OK to ask for helpfrom family, friends, and your coachas you recover. Keep active! Use the Patient andFamily Activity Tracker on page 27 tomonitor your activity. Listen to your body! It’s normal to besore, but do not over-do youractivities. Make sure you areobserving the restrictions by yourdoctor. It’s normal to have ups and downswith your pain. As the nerves heal,they may be very irritated and painful.It can take several weeks or months forthis pain to go away. Keep an eye on your food and fluidintake. Make sure you are eating aYour Guide to Spine SurgeryPage 33Revised 11/2016 Help prevent constipation byincreasing fiber and fluids in your diet.You can take an over-the-counter stoolsoftener. Medicines for pain can slowdown your digestive system.
Frequently Asked QuestionsQ:What can I do after surgery?A:Walking is encouraged. Limit sitting to 30 minutes at a time, or as tolerated. Follow theactivity limits given to you by your doctor and therapy team.Q:Can I drive?A:We do not recommend driving for at least 2 weeks after your surgery. Medicine makes youslower to react and pain can distract you from the road.Q:How should I take care of my incision?A:Sutures that do not absorb and staples will typically be removed by a Medical Assistant inthe office 2 weeks after surgery. Paper tapes (steri-strips) will fall off by themselves over1-2 weeks. Please do not apply creams or lotions to your incision until healed.Q:Can I shower?A:You may shower 2 days after surgery, taking care not to scrub or soak the incision. Pat drywith a clean towel. Wash your hands frequently and do not allow others to touch yourincision.Your Guide to Spine SurgeryPage 34Revised 11/2016
When to call:CALL MY SURGEON IF: There is redness, swelling, or increasing pain in the wound (incision). There is drainage from the wound lasting longer than one day. I have an unexplained oral temperature above 100.4 (38 C). I notice a bad smell or pus coming from the wound or dressing. My wound separates or breaks open after the stitches have been removed. I develop new symptoms of weakness, numbness or pain that does not go away. I develop a rash or itching from my medications. I have been taking stool softeners and have not had a bowel movement in 4 days.CALL MY PRIMARY CARE DOCTOR IF: I develop dizzy episodes or fainting while standing. I develop nausea and vomiting that will not go away. I have problems with controlling my blood sugar or blood pressure after surgery.SEEK IMMEDIATE ATTENTION / CALL 911 IF: I have chest pain or difficulty breathing. I have sudden weakness on one side of my body, facial drooping and/or slurred speech.Your Guide to Spine SurgeryPage 35Revised 11/2016
ResourcesUseful Phone NumbersBronson Methodist Hospital operator . .(269) 341-7654Bronson HealthAnswers . (269) 341-7723 or (800) 451-6310Bronson Pre-Admission Center . .(269) 341-7940Bronson Case Management . .(269) 341-7943Bronson Rehabilitation Services – Van Buren County . (269) 657-1490Bronson Rehabilitation Services – Kalamazoo County .(289) 544-3230, ext 1- Vicksburg, Kalamazoo (John St), Kalamazoo (BMH), Kalamazoo (LIRC/BAC)Bronson Rehabilitation Services – Centre Ave .(269) 488-3240Bronson Rehabilitation Services – Turwill Lane . .(269) 488-7380Bronson Rehabilitation Services – West Main St. . .(269) 488-8360Bronson Rehabilitation Services – Calhoun County . (269) 245-8125Office numbers and addresses:Dr. Alain FabiBronson Neuroscience Center – NeurosurgeryDr. Chris Sloffer601 John Street, Suite M-124, Kalamazoo, MI 49007Dr. Daryl WarderPhone (269) 341-7500 Fax (269) 341-7540Dr. Greg WigginsDr. Josh EllwitzBronson HealthCare Midwest Spine and Scoliosis CenterDr. Michael Kasten601 John Street, Suite M-206A, Kalamazoo, MI 49007Phone (269) 488-8355 Fax (269) 488-8356Dr. Karen BovidWMed Orthopaedic Clinic1000 Oakland Drive, Kalamazoo, MI 49007Phone (269) 337-6200 Fax (269) 337-6222Your Guide to Spine SurgeryPage 36Revised 11/2016
Useful websites:General Information:Senior Services of Kalamazoo can link you toWatch educational videos, learn about yourcommunity resources:surgery, and view the resources Bronson haswww.seniorservices1.orgto offer:918 Jasper Streetwww.bronsonhealth.comKalamazoo, MI 49001(269) 382-0515Spine Health can give you information aboutneck and back rican Occupation Therapy Association:Lending Hands can provide free medicalwww.aota.orgequipment (walkers, raised toilet seats, showerchairs):www.lendinghandsmi.orgAmerican Physical Therapy Association:www.apta.org5350 Ivanhoe CourtPortage, MI 49002(269) 567-4381Physician Associations:American Academy of Orthopaedic Surgeons:Some medical supplies may be purchased atthese locations:Bronson Outpatient Pharmacy & Gift Shop,First floorwww.aaos.orgAmerican Association of NeurologicalSurgeons:www.aans.org(269) 341-7207Congress of Neurosurgeons:www.neurosurgeon.orgNorth American Spine Society:www.spine.orgYour Guide to Spine SurgeryPage 37Revised 11/2016
Your Guide to Spine Surgery P a g e 8 Revised 11/2016 Problems with bones Bones in the spine can break (fracture) due to accidents, thin down over time or form cancer of the bones. Some fractures can cause weakness within the spine and pain. Surgery can help to strengthen your spine. This may lessen your pain. Vertebral Body Fractured