Transcription
Help us to improve SIGN guidelines click here to complete our surveySIGN 136 Management of chronic painA national clinical guidelineDecember 2013Evidence
KEY TO EVIDENCE STATEMENTS AND GRADES OF RECOMMENDATIONSLEVELS OF EVIDENCE1 High quality meta-analyses, systematic reviews of RCTs, or RCTs with a very low risk of bias1 Well conducted meta-analyses, systematic reviews, or RCTs with a low risk of bias1-Meta-analyses, systematic reviews, or RCTs with a high risk of bias High quality systematic reviews of case control or cohort studies2 Highquality case control or cohort studies with a very low risk of confounding or bias and a high probability that therelationship is causal2 Well conducted case control or cohort studies with a low risk of confounding or bias and a moderate probability that therelationship is causal2- Case control or cohort studies with a high risk of confounding or bias and a significant risk that the relationship is not causal3Non-analytic studies, eg case reports, case series4Expert opinionGRADES OF RECOMMENDATIONNote: The grade of recommendation relates to the strength of the evidence on which the recommendation is based. It does not reflect theclinical importance of the recommendation.AB t least one meta-analysis, systematic review, or RCT rated as 1 ,Aand directly applicable to the target population; or body of evidence consisting principally of studies rated as 1 ,Adirectly applicable to the target population, and demonstrating overall consistency of resultsA body of evidence including studies rated as 2 ,d irectly applicable to the target population, and demonstrating overall consistency of results; orExtrapolated evidence from studies rated as 1 or 1 CA body of evidence including studies rated as 2 , directly applicable to the target population and demonstrating overall consistency of results; orExtrapolated evidence from studies rated as 2 DEvidence level 3 or 4; orExtrapolated evidence from studies rated as 2 GOOD PRACTICE POINTS Recommended best practice based on the clinical experience of the guideline development groupNHS Evidence has accredited the process used by Scottish Intercollegiate GuidelinesNetwork to produce guidelines. Accreditation is applicable to guidance producedusing the processes described in SIGN 50: a guideline developer’s handbook, 2008edition . More information onaccreditation can be viewed at www.evidence.nhs.ukHealthcare Improvement Scotland (HIS) is committed to equality and diversity and assesses all its publications for likely impact on thesix equality groups defined by age, disability, gender, race, religion/belief and sexual orientation.SIGN guidelines are produced using a standard methodology that has been equality impact assessed to ensure that these equalityaims are addressed in every guideline. This methodology is set out in the current version of SIGN 50, our guideline manual, which canbe found at www.sign.ac.uk/guidelines/fulltext/50/index.html. The EQIA assessment of the manual can be seen atwww.sign.ac.uk/pdf/sign50eqia.pdf. The full report in paper form and/or alternative format is available on request from theHealthcare Improvement Scotland Equality and Diversity Officer.Every care is taken to ensure that this publication is correct in every detail at the time of publication. However, in the event of errorsor omissions corrections will be published in the web version of this document, which is the definitive version at all times. This versioncan be found on our web site www.sign.ac.uk.This document is produced from elemental chlorine-free material and is sourced from sustainable forests.
Scottish Intercollegiate Guidelines NetworkManagement of chronic painA national clinical guidelineDecember 2013
Management of chronic painScottish Intercollegiate Guidelines NetworkGyle Square, 1 South Gyle CrescentEdinburgh EH12 9EBwww.sign.ac.ukFirst published December 2013ISBN 978 1 909103 17 7Citation textScottish Intercollegiate Guidelines Network (SIGN).Management of chronic pain. Edinburgh: SIGN; 2013.(SIGN publication no. 136). [December 2013]. Available from URL: http://www.sign.ac.ukSIGN consents to the photocopying of this guideline for the purposeof implementation in NHSScotland.
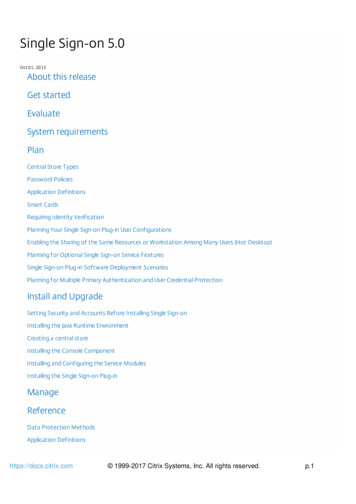
ContentsContents1Introduction.11.1The need for a guideline. 11.2Remit of the guideline. 11.3Definitions. 21.4Reporting in pain trials. 21.5Statement of intent. 32Key recommendations.52.1Assessment and planning of care. 52.2Supported self management. 52.3Pharmacological management. 52.4Psychologically based interventions. 52.5Physical therapies. 53Assessment and planning of care.63.1Assessment tools. 63.2Timing of intervention. 63.3Care management. 73.4Patient-professional interaction. 74Supported self management.85Pharmacological therapies.95.1Introduction. 95.2Non-opioid analgesics (simple and topical). 105.3Opioids. 125.4Anti-epilepsy drugs. 155.5Antidepressants. 175.6Combination therapies. 196Psychologically based interventions.206.1Multidisciplinary pain management programmes. 206.2Unidisciplinary education. 216.3Behavioural therapies. 226.4Cognitive behavioural therapy. 236.5Mindfulness meditation and acceptance and commitment therapy. 247Physical therapies.257.1Manual therapy. 257.2Exercise. 267.3Traction. 287.4Electrotherapy. 288Complementary therapies.298.1Acupuncture. 298.2Herbal medicine. 29
ther therapies. 309Dietary therapies.3110Provision of information.3210.1Sources of further information. 3210.2Checklist for provision of information. 3411Implementing the guideline.3511.1Implementation strategy. 3511.2Resource implications of key recommendations. 3511.3Auditing current practice. 3511.4Additional advice to NHSScotland from Healthcare Improvement Scotland andthe Scottish Medicines Consortium. 3612The evidence base.3712.1Systematic literature review. 3712.2Recommendations for research. 3712.3Review and updating. 3813Development of the guideline.3913.1Introduction. 3913.2The guideline development group. 3913.3Consultation and peer review. 40Abbreviations.42Annex 1.44Annex 2.48Annex 3 .52Annex 4.54Annex 5.58References.59
1 Introduction1Introduction1.1 the need for a guidelineChronic pain is a major clinical challenge: across Europe approximately 18% of the population are currentlyaffected by moderate to severe chronic pain.1 It has a considerable impact on quality of life, resulting insignificant suffering and disability.2-4 While in many cases it is accepted that a cure is unlikely, the impact onquality of life, mood and function can be significantly reduced by appropriate measures. Chronic pain not onlyhas an impact on affected individuals and their families, it also has substantial economic costs. For example,back pain alone was estimated to cost 12 billion per annum in the UK in 1998, and arthritis-associated paincosts around 2.5% of the gross national product of Western nations.5,6While a proportion of patients will require access to specialist secondary and tertiary care pain services, themajority of patients will be managed in the community or primary care. It is vital that general practitioners(GPs) and other healthcare professionals have the best possible resource and support to manage their patientsproperly and have facilities for accessing appropriate specialist services when required. Within Scotland there isevidence of wide variation in clinical practice service and resource provision, with a general lack of knowledgeabout chronic pain and the management options that are available.7A wide range of both pharmacological and non-pharmacological management strategies are available forchronic pain. The challenge is to understand the extensive published evidence for different treatments andto determine when and where to use them for the best long term outcomes for the patient. It is hoped thatthis evidence based guideline will provide the information needed to improve clinical outcomes and qualityof life for patients with chronic pain.1.2REMIT of the guideline1.2.1 overall objectivesThis guideline provides recommendations based on current evidence for best practice in the assessmentand management of adults with chronic non-malignant pain in non-specialist settings.It does not cover:yy interventions which are only delivered in secondary care.yy treatment of patients with headache (see SIGN 107, Diagnosis and management of headache in adults).8yy children. While chronic pain occurs in children, some of their treatment options are different to those ofadults, and evidence on the paediatric population has not been included in this remit.yy underlying conditions. Chronic pain is caused by many underlying conditions. The treatment of theseconditions is not the focus of this guideline so the search strategies were restricted to the treatment ofchronic pain, not specific conditions.Details of the literature review are covered in section 12 and the key questions used to develop the guidelinecan be found in Annex 1. SIGN guidelines on other relevant topics are available on the SIGN website,www.sign.ac.uk.8-121.2.2 target users of the guidelineThis guideline will be of particular interest to all healthcare professionals involved in the assessment andmanagement of patients with chronic pain, including general practitioners, pharmacists, anaesthetists,psychologists, psychiatrists, physiotherapists, rheumatologists, occupational therapists, nurses, patients,carers and voluntary organisations with an interest in chronic pain. 1
Management of chronic pain1.3 definitionsIn this guideline chronic pain is defined as pain that has been present for more than 12 weeks.The non-specialist setting is any setting where the training and infrastructure is not specifically designedfor treating chronic pain. This might include management in the community, primary care or secondarycare.1.4 reporting in pain trialsDifficulties in reporting make the interpretation of the evidence base challenging. Pain is defined by theInternational Association for the Study of Pain as “an unpleasant sensory or emotional experience associatedwith actual or potential tissue damage, or described in terms of such damage”.13 Chronic pain is a complexphenomenon with consequent challenges for its assessment and management both in clinical trials androutine clinical practice. This is further complicated by the fact that even in the same condition there maybe quite different pain mechanisms among patients. While changes in the peripheral pain processing mightpredominate in one patient, central changes may be much more important in the next patient.14-16 While aparticular treatment may work very effectively in one patient, it may not work at all in another patient withthe same condition. In clinical trials, unless there is careful assessment of the chronic pain syndrome in eachpatient, potentially useful treatments may be discarded as being ineffective when the average responseis considered. Even good quality, adequately powered double blind randomised controlled trials may notprovide the best approach for developing a strong evidence base for pain management.17-19These limitations have been recognised internationally, leading to the development of the Initiative onMethods, Measurement and Pain Assessment in Clinical Trials (IMMPACT, www.immpact.org) in 2002.A number of factors need to be considered in order to optimise the design of trials studying chronic pain.These include patient selection (pain diagnosis, duration, intensity) and sample size, different phases withinthe trial (eg enriched enrolment) and duration of study, treatment groups (including active versus inactiveplacebo comparator), dosing strategies (fixed versus flexible) and type of trial (eg parallel, crossover).17,20,21To allow comparison between studies a standardised approach to outcome measures, is recommended byIMMPACT.17 Four key domains are recommended to adequately assess outcomes:1. Pain intensity. A numerical rating scale 0-10 is recommended as the most practical and sensitive.2. Physical functioning. Assessment with validated self report questionnaires such as the MultidimensionalPain Inventory or Brief Pain Inventory interference scales is recommended.3. Emotional functioning. The Beck Depression Inventory and the Profile of Mood States are recommended.4. Patient rating of overall improvement. The Patient Global Impression of Change scale can be used.Side effects and detailed information about patient recruitment and progress through the trial should alsobe recorded.22,23While much of the literature published to date does provide a sound evidence base for this guideline, it ishoped that future studies will follow the IMMPACT recommendations.In addition to the limitations of assessment and trial design, concerns have been raised about how analysismethods may either obscure clinically important positive outcomes, or overestimate treatment effects. Ifthe average response is considered, a treatment may appear ineffective, whereas it could have the potentialto be effective in a particular subgroup of the patients being studied. It may, therefore, be useful to analyseresponders to a particular treatment separately from non-responders.19Another important factor is how patients who drop out before completing the study are dealt with inthe analysis. Using the last-observation-carried-forward (LOCF) for patients who drop out is based on theassumption that in a randomised controlled trial (RCT) drop-outs will occur randomly between the treatmentgroups. The active treatment may be an effective analgesic but if it has an unpleasant side effect profile thendrop-outs are likely to be higher in a non-random manner in this treatment group. Pain scores prior to dropout may therefore demonstrate efficacy, but in clinical practice this treatment is unlikely to be tolerated.2
1 IntroductionThe majority of RCTs use the imputation method of LOCF, and may therefore potentially overestimate thetreatment effect.24While there are a number of good quality systematic reviews and meta-analyses that provide an evidence basefor the management of patients with chronic pain, there are some limitations with the currently publishedliterature. This has been taken into consideration by the guideline development group when appraisingthe evidence and, where there are areas of potential doubt, recommendations have been downgradedaccordingly. Further details of the literature review can be found in section 12.1.5Statement of intentThis guideline is not intended to be construed or to serve as a standard of care. Standards of care aredetermined on the basis of all clinical data available for an individual case and are subject to changeas scientific knowledge and technology advance and patterns of care evolve. Adherence to guidelinerecommendations will not ensure a successful outcome in every case, nor should they be construed asincluding all proper methods of care or excluding other acceptable methods of care aimed at the sameresults. The ultimate judgement must be made by the appropriate healthcare professional(s) responsiblefor clinical decisions regarding a particular clinical procedure or treatment plan. This judgement should onlybe arrived at following discussion of the options with the patient, covering the diagnostic and treatmentchoices available. It is advised, however, that significant departures from the national guideline or any localguidelines derived from it should be fully documented in the patient’s case notes at the time the relevantdecision is taken.1.5.1Patient versionA patient version of this guideline is available from the SIGN website, www.sign.ac.uk1.5.2prescribing oF licensed medicines outwith their marketing authorisationRecommendations within this guideline are based on the best clinical evidence. Some recommendationsmay be for medicines prescribed outwith the marketing authorisation (MA) also known as product licence.This is known as ‘off label’ use.Medicines may be prescribed off label in the following circumstances:yyyyyyyyfor an indication not specified within the marketing authorisationfor administration via a different routefor administration of a different dosefor a different patient population.An unlicensed medicine is a medicine which does not have MA for medicinal use in humans.Generally the off label use of medicines becomes necessary if the clinical need cannot be met by licensedmedicines within the marketing authorisation. Such use should be supported by appropriate evidence andexperience.25“Prescribing medicines outside the conditions of their marketing authorisation alters (and probably increases)the prescribers’ professional responsibility and potential liability”.25The General Medical Council (GMC) recommends that when prescribing a medicine off label, doctors should:yy b e satisfied that such use would better serve the patient’s needs than an authorised alternative (if oneexists).yy be satisfied that there is sufficient evidence/experience of using the medicines to show its safety andefficacy, seeking the necessary information from appropriate sources.yy record in the patient’s clinical notes the medicine prescribed and, when not following common practice,the reasons for the choice.yy take responsibility for prescribing the medicine and for overseeing the patient’s care, including monitoringthe effects of the medicine. 3
Management of chronic painNon-medical prescribers should ensure that they are familiar with the legislative framework and their ownprofessional prescribing standards.Prior to any prescribing, the licensing status of a medication should be checked in the summary of productcharacteristics (SPC).26 The prescriber must be competent, operate within the professional code of ethics oftheir statutory bodies and the prescribing practices of their employers.271.5.3additional advice to nhsscotland from HEALTHCARE improvement scotland and thescottish medicines consortiumHealthcare Improvement Scotland processes multiple technology appraisals (MTAs) for NHSScotland thathave been produced by the National Institute for Health and Care Excellence (NICE) in England and Wales.The Scottish Medicines Consortium (SMC) provides advice to NHS Boards and their Area Drug and TherapeuticsCommittees about the status of all newly licensed medicines and any major new indications for establishedproducts.SMC advice relevant to this guideline is summarised in section 11.4.4
2 Key recommendations2Key recommendationsThe following recommendations were highlighted by the guideline development group as the key clinicalrecommendations that should be prioritised for implementation. The grade of recommendation relates to thestrength of the supporting evidence on which the recommendation is based. It does not reflect the clinicalimportance of the recommendation.2.1 assessment and planning of care concise history, examination and biopsychosocial assessment, identifying pain type (neuropathic/Anociceptive/mixed), severity, functional impact and context should be conducted in all patients withchronic pain. This will inform the selection of treatment options most likely to be effective.2.2 supported self management ealthcare professionals should signpost patients to self help resources, identified and recommendedHby local pain services, as a useful aide at any point throughout the patient journey. Self managementmay be used from an early stage of a pain condition through to u
Scottish Intercollegiate Guidelines Network Gyle Square, 1 South Gyle Crescent Edinburgh EH12 9EB www.sign.ac.uk First published December 2013 ISBN 978 1 909103 17 7 Citation text Scottish Intercollegiate Guidelines Network (SIGN). Management of chronic pain. Edinburgh: SIGN; 2013. (SIGN publication no. 136). [December 2013].