Transcription
Journal of Hospital Infection (2007) 67, y five moments for hand hygiene’:a user-centred design approach to understand,train, monitor and report hand hygieneH. Sax a,b, B. Allegranzi b, I. Uçkay a, E. Larson b,c, J. Boyce b,d,D. Pittet a,b,*aInfection Control Programme, University of Geneva Hospitals, Geneva, SwitzerlandGlobal Patient Safety Challenge, World Alliance for Patient Safety, World Health Organization,Geneva, SwitzerlandcSchool of Nursing, Mailman School of Public Health, Columbia University, New York, NY, USAdHospital of Saint Raphael, New Haven, CT, USAbAvailable online 27 August 2007KEYWORDSHand hygiene;Healthcare-associatedinfections; Patientsafety; HealthcareworkersSummary Hand hygiene is a core element of patient safety for the prevention of healthcare-associated infections and the spread of antimicrobialresistance. Its promotion represents a challenge that requires a multimodal strategy using a clear, robust and simple conceptual framework.The World Health Organization First Global Patient Safety Challenge ‘CleanCare is Safer Care’ has expanded educational and promotional tools developed initially for the Swiss national hand hygiene campaign for worldwideuse. Development methodology involved a user-centred design approachincorporating strategies of human factors engineering, cognitive behaviourscience and elements of social marketing, followed by an iterative prototype test phase within the target population. This research resulted ina concept called ‘My five moments for hand hygiene’. It describes the fundamental reference points for healthcare workers (HCWs) in a timeespaceframework and designates the moments when hand hygiene is required toeffectively interrupt microbial transmission during the care sequence. Theconcept applies to a wide range of patient care activities and healthcaresettings. It proposes a unified vision for trainers, observers and HCWs thatshould facilitate education, minimize inter-individual variation and resource use, and increase adherence. ‘My five moments for hand hygiene’* Corresponding author. Address: Infection Control Programme, University of Geneva Hospitals, 24 Rue Micheli-du-Crest, 1211Geneva 14, Switzerland. Tel.: þ41 22 372 9828; fax: þ41 22 372 3987.E-mail address: didier.pittet@hcuge.ch0195-6701/ - see front matter ª 2007 The Hospital Infection Society. Published by Elsevier Ltd. All rights reserved.doi:10.1016/j.jhin.2007.06.004
10H. Sax et al.bridges the gap between scientific evidence and daily health practice andprovides a solid basis to understand, teach, monitor and report hand hygiene practices.ª 2007 The Hospital Infection Society. Published by Elsevier Ltd. All rightsreserved.IntroductionHealthcare-associated infections (HCAIs) represent a major risk to patient safety and contributetowards suffering, prolongation of hospital stay,cost and mortality.1,2 Hand hygiene is the coreelement to protect patients against HCAIs and colonisation with multi-resistant micro-organisms.3Cleansing hands with alcohol-based hand rub isa simple and undemanding procedure that requiresonly a few seconds.4,5 If hand rub is easily available at each point of care, hand hygiene can alsoeasily be integrated in the natural workflow eeven in high-density care settings.6e8 However,most healthcare workers (HCWs) practice handhygiene less than half as often as they should.9,10Reasons for neglecting hand hygiene have beeninvestigated and include forgetfulness, fear of skindamage, lack of time due to other patient carepriorities, and scarce or inconvenient access tohand rub and sinks.11,12 However, one essential element is frequently overlooked: the quality of theinformation and training dispensed to HCWs to explain why, when and how to apply hand hygieneduring routine care activity. Yet, there is accumulating evidence that failure to comply with goodpractice is often due to poor design, whether itbe device-related, humanemachine interfaces or,importantly, process design.13e15 This includesmisleading language, complicated descriptions,or poor definition of target outcomes.16Several disciplines such as human factors engineering and ergonomics, social marketing, pedagogy, and communication science have been foundto be helpful in bridging the gap between scientificliterature and user-centred, error-proof productsand processes.17e20 When measured against thesestandards, the concept of hand hygiene has beenpoorly assessed from these perspectives untilnow. Even infection control experts have difficulties in reaching a consensus on the relative risklevels of different care activities and how to bestdefine key moments for hand hygiene action.Building on the longstanding experience at theUniversity of Geneva Hospitals and work on tooldevelopment in the framework of the Swiss national hand hygiene campaign and the WHO GlobalPatient Safety Challenge ‘Clean Care is SaferCare’, we developed a user-centred concept forrecognising when hand hygiene should be done, aswell as training, performance assessment andreporting.6e8,11,21e32 We describe here the designprocess of the concept, the rationale for elementsincluded, and its potential practical use.Requirements and developmentRequirement specifications for auser-centred hand hygiene conceptThe main specifications for the concept are givenin Table I. Importantly, it must result in a minimalcomplexity and density of hand hygiene actions,integrate well into a natural workflow, but still attain a maximum preventive effect. For applicability across a wide range of care settings andhealthcare professions, it must also create a unified approach without losing the necessary detailto produce meaningful data for risk analysis andfeedback.The concept should be absolutely congruent indesign and meaning to trainers, observers and theobserved HCWs. This has the dual purpose ofavoiding any lack of clarity by an expertelayperson gap and to cut down on training timerequirement and expenditure. Moreover, thesharing of a unified vision should lead to a strongsense of ownership.33 Additionally, concept robustness is equally instrumental both to avoid interobserver variation and to guarantee intra-hospital,Table I Requirement specifications for a usercentred hand hygiene application conceptConsistent with evidence-based risk assessment ofhealthcare-associated infections and spread of multiresistant micro-organismsStealth integration into a natural care workflowEasy to learnLogical clarity of the conceptApplicable in a wide range of healthcare settingsMinimising the density of the need for hand hygieneMaximal concept congruence between trainers,observers, and healthcare workers
‘My five moments for hand hygiene’inter-hospital and international comparisons andcommunication.Finally, characteristics known to neuroscience toincrease learning and facilitate uptake such aslimited number of items, clustering of items, symmetry, rhythm, plain and meaningful terminology,colour codes, clarity and logic, high signal-to-noiseratio, and correspondence to pre-existing conceptsin the concerned population were applied duringthe design process whenever possible.34e3611In addition to patient colonisation and/or infection, two additional negative outcomes are targetedby hand hygiene: infection in HCWs with pathogenscontained in body fluids and cross-colonisation ofinanimate objects in the healthcare environmentand colonisation of HCWs by patient flora.In summary, four negative outcomes constitutethe prevention target for hand hygiene: (i) crosscolonisation of patients; (ii) endogenous and exogenous infection in patients; (iii) infection inHCWs; and (iv) cross-colonisation of the healthcareenvironment including HCWs.Healthcare-associated colonisation andinfection: the negative outcome targetsThe core element of hand transmissionFor conceptual clarity, it is useful to revisit twodistinct outcomes of transmission pathways. Colonisation denotes the presence of micro-organisms onbody sites without invading the tissue and withouttriggering a symptomatic host defence reaction;infection denotes tissue invasion of micro-organismstriggering an inflammatory host response.37Transmission of micro-organisms from the healthcare environment (e.g. furniture, equipment, walls,doors, documents, neighbouring patients, etc.) toa patient most often results in cross-colonisation andnot in infection.38,39 Cross-colonisation with multiresistant micro-organisms represents an importanttarget for prevention because it contributes to increasing antimicrobial resistance and the reservoirof potential pathogens.40,41With respect to cross-colonisation, it is important to recognise three facts: first, colonised orinfected patients represent the main reservoir forhealthcare-associated micro-organisms; second,the environment in the healthcare facility containsa wide variety of different healthcare-associatedmicro-organisms and represents a secondarysource for transmission; and third, the immediatepatient environment becomes colonised by thepatient flora.42e47 Cross-transmission can resultin exogenous HCAI, in particular if the patient’sdefence against the implicated micro-organism islow or if it is directly introduced into a vulnerablebody site, or mucous membrane.48Most HCAIs, however, are of an endogenousnature, and due to micro-organisms already colonising the patient before the onset of infection.39,49 This implies that hands may play a rolein this process by transferring micro-organismsfrom a colonised body site to a ‘clean’ one in thesame patient, e.g. from the perineum to a trachealtube, or from the leg skin to a catheter hub.3 Careinduced breaks of physical and biological defencemechanisms by invasive procedures and devicesrepresent risk factors for infection.During daily practice, HCWs’ hands typically toucha continuous sequence of surfaces and substancesincluding inanimate objects, patients’ intact ornon-intact skin, mucous membranes, food, waste,body fluids and the HCW’s own body. The totalnumber of hand exposures in a healthcare facilitymight reach as many as several tens of thousands perday. With each hand-to-surface exposure a bidirectional exchange of micro-organisms between handsand the touched object occurs and the transienthand-carried flora is thus continuously changing. Inthis way, micro-organisms can spread throughouta healthcare environment within a few hours.50,51An evidence-based hand transmission model hasbeen described elsewhere.3,27 In brief, we illustrate the core elements stripped down to theirsimplest level in Figure 1. Effective hand cleansingcan prevent transmission of micro-organisms fromsurface A to surface B if applied at any momentduring hand transition between the two surfaces.Typically, surface A could be a door handle colonised by meticillin-resistant Staphylococcus aureus(MRSA) and surface B the skin of a patient. If transmission of micro-organisms between A and B wouldresult in one of the four negative outcomes detailed above, the corresponding hand transitiontime between the surfaces is usually calleda ‘hand hygiene opportunity’. If avoidable, nottouching A or B or both would be another very effective way of preventing cross-contamination andinfection. Touching twice in a row surface B wouldequally not generate a need for hand hygiene.Hence, it follows clearly that the necessity forhand hygiene is defined by a core element ofhand transmission consisting in a donor surface,a receptor surface and hand transition from thefirst to the second. Merely describing a hand hygiene opportunity as a moment before executinga certain care task is an oversimplification andwill be discussed in a further section.
12H. Sax et al.Figure 1 Core element of hand transmission. (1) Donor surface ‘A’ contains micro-organisms ‘a’; receptor surface‘B’ micro-organisms ‘b’. (2) A hand picks up a micro-organism ‘a’ from donor surface ‘A’ and carries it over to receptorsurface ‘B’, no hand hygiene action performed. (3) Receptor surface ‘B’ is now cross-contaminated with microorganism ‘a’ in addition to original flora ‘b’. The arrow marks the opportunity for hand hygiene, e.g. the time periodand geographical dislocation within which hand hygiene will prevent cross-transmission; the indications for handhygiene are determined by the need to protect surface ‘B’ against colonisation with ‘a’ e the preventable negativeoutcome in this example.Conceptualisation of the risk: two zones,two critical sitesTo achieve the objective of creating a user-centredconcept, we opted for a direct translation of theevidence-based hand transmission model describedabove to a practical description of hand hygieneindications. The terms ‘zone’ and ‘critical sites’were introduced to allow a ‘geographical’ visualisation of key moments for hand hygiene (Figure 2A).Focusing on a single patient, the healthcaresetting is divided into two virtual geographicalareas, the patient zone and the healthcare zone(Figure 2A and B).The patient zone contains the patient X and his/her immediate surroundings. This typically includes the intact skin of the patient and allinanimate surfaces that are touched by or in directphysical contact with the patient such as the bedrails, bedside table, bed linen and infusion tubingand other medical equipment. It further containssurfaces frequently touched by HCWs while caringfor the patient such as monitors, knobs andbuttons, and other ‘high frequency’ touch surfaceswithin the patient zone. The model assumes thatthe patient flora rapidly contaminates the entirepatient zone, but that it is being cleaned betweenpatient admissions.The healthcare zone contains all surfaces outsidethe patient zone of patient X, i.e. all other patientsand their patient zones and the healthcare facilityenvironment. Conceptually, the healthcare zone iscontaminated with micro-organisms that might beforeign and potentially harmful to patient X, eitherbecause they are multi-resistant or because theirtransmission might result in exogenous infection.
‘My five moments for hand hygiene’13APATIENT ZONEClean SiteBody Fluid SiteHEALTHCARE ZONEB2BEFORE ASEPTICTASKBEFOREAFTER1 PATIENT4 PATIENTCONTACTCONTACT3AFTER BODY FLUIDEXPOSUREAFTERCONTACTS WITH5 PATIENTSURROUNDINGSFigure 2 Unified visuals for ‘My five moments for hand hygiene’. Patient zone defined as the patient’s intact skinand his/her immediate surroundings colonised by the patient flora and healthcare zone containing all other surfaces.(A) Symbols for clean site and body fluid site, two critical sites for hand hygiene within the patient zone. (B) Zones andsites with inserted timeespace representation of ‘My five moments for hand hygiene’.
14Within the patient zone, two critical sites shouldbe distinguished (Figure 2A): clean sites corresponding to body sites or medical devices thathave to be protected against micro-organisms potentially leading to HCAIs, and body fluid sites leading to hand exposure to body fluids and blood-bornepathogens. Critical sites may co-exist: drawingblood for example would result in a clean site anda body fluid site at the same time at the site ofneedle perforation of the skin. The added valueof critical sites lies in their potential use in visualmaterial and training: risk-prone tasks becomegeographically located and hence more palpable.The concept and its practicalapplication‘My five moments for hand hygiene’explainedThe geographical representation of the two zonesand the two critical sites (Figure 2A) is useful to introduce the five moments for hand hygiene. Thecorrelation between these five moments and theindications for hand hygiene according to WHOGuidelines on Hand Hygiene in Healthcare27 isgiven in Table II. To further facilitate ease of recalland expand the ergonomic dimension, the five moments for hand hygiene are numbered according tothe habitual care workflow (Figure 2B).Moment 1: Before patient contactFrom the two-zone concept, a major moment forhand hygiene is naturally deduced. It occursbetween the last hand-to-surface contact with anobject belonging to the healthcare zone and thefirst within the patient zone e best visualised bycrossing the virtual line between the two zones.Hand hygiene at this moment will mainly preventcross-colonisation of the patient and, occasionally,exogenous infection. A concrete example would bethe temporal period between touching the doorhandle and shaking the patient’s hand: the doorhandle belongs to the healthcare zone and thepatient’s hand to the patient zone.H. Sax et al.Importantly, hand hygiene required at this momentaims at preventing colonisation and HCAI. In linewith the predominantly endogenous aetiology ofthese infections, hand hygiene is taking placebetween the last exposure to a surface, evenwithin the patient zone and immediately beforeaccess to a clean site. This is important becauseHCWs customarily touch another surface within thepatient zone before contact with a clean site.For some tasks on clean sites, e.g. lumbarpuncture, surgical procedures, tracheal suctioning, etc., the use of gloves is standard procedure.In this case, hand hygiene is required beforedonning gloves because gloves alone may notprevent contamination entirely.25,52e54Moment 3: After body fluid exposure riskAfter a care task associated with a risk to exposehands to body fluids, e.g. after accessing a bodyfluid site, hand hygiene is required instantly andmust take place before any hand-to-surface exposure, even within the same patient zone. This hasa double objective. First and most importantly, itreduces the risk of colonisation or infection ofHCWs with infectious agents which can occur evenin the absence of visible soiling. Second, it reducesthe risk of a transmission of micro-organisms froma ‘colonised’ to a ‘clean’ body site within the samepatient.3,27 This routine moment for hand hygieneconcerns all care actions associated with a risk ofbody fluid exposure and is not identical to thehopefully very rare case of accidental visible soiling calling for immediate handwashing.27 Often,clean sites coincide with body fluid sites (Table II).Disposable gloves are meant to be used asa ‘second skin’ to prevent exposure of hands tobody fluids. However, hands are not sufficientlyprotected by gloves and hand hygiene is stronglyrecommended after glove removal.27 Even if gloveremoval represents a strong cue to hand hygiene action, the concept chooses to identify this momentfor hand hygiene with the associated risk (e.g. exposure to body fluids) rather than with the additional protective action (e.g. glove use). This hasthe double advantage of being more consistentwith the risk-driven logic of the overall conceptand to cover all times when gloves are not worn.55Moment 2: Before an aseptic taskMoment 4: After patient contactOnce within the patient zone, usually after a handexposure to the patient’s intact skin, clothes or anyother object, the HCW might engage in an aseptictask on a clean site such as opening a venous accessline, giving an injection, or performing wound care.After a care sequence, when leaving the patientzone and before touching an object in the healthcare zone, hand hygiene action substantially reduces contamination of HCWs’ hands with the flora
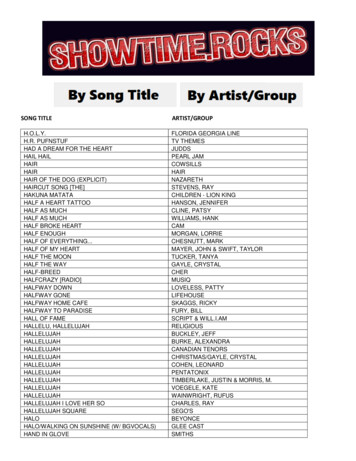
‘My five moments for hand hygiene’: explanations and link to evidence-based recommendationsMomentEndpoints of nk to WHO Guidelines for Hand Hygiene in Health Care27WHO recommendation(ranking for onor surface: anysurface in thehealthcare zone.Receptor surface:any surface in thepatient zonePatient crosscolonisation;rarely exogenousinfectionShaking hands, helping a patient Before and after touchingpatients (IB)to move around, gettingwashed, taking pulse, bloodpressure, chest auscultation,abdominal palpationThe two moments before and aftertouching a patient were separatedbecause of their specific sequentialoccurrence in routine care andunequal negative outcome in caseof failure to adhere, and usualadherence level.2BeforeaseptictaskDonor surface: anyother surfaceReceptor surface:clean sitePatientendogenousinfection; rarelyexogenousinfectionOral/dental care, secretionaspiration, skin lesion care,wound dressing, subcutaneousinjection; catheter insertion,opening a vascular accesssystem; preparation of food,medication, dressing setsBefore handling aninvasive device for patientcare, regardless ofwhether or not gloves areused (IB)This concept was enlarged to coverall transfer of micro-organisms tovulnerable body sites potentiallyresulting in infection.If moving from acontaminated body site toa clean body site duringpatient care (IB)Since it is not possible to determinethese body sites objectively, thisindication was not retained as aseparate item, but covered bywithin-patient-zone moments.After removing gloves (IB)‘After body fluid exposure risk’covers this recommendation; seetext for further comments.After contact with bodyfluids or excretions,mucous membranes, nonintact skin, or wounddressings (IA)This risk was generalised to includeall tasks that can potentially resultin hand exposure to body fluids. Aparadox of body fluid exposure wasresolved by including the notion ofexposure risk instead of actualexposure.3After bodyfluidexposureriskDonor surface: bodyfluid siteReceptor surface:any other surfaceHealthcareworker infectionOral/dental care, secretionaspiration; skin lesion care,wound dressing, subcutaneousinjection; drawing andmanipulating any fluid sample,opening draining system,endotracheal tube insertion andremoval; clearing up urines,faeces, vomit, handling waste(bandages, napkin, incontinencepads), cleaning of contaminatedand visibly soiled material orareas (lavatories, medicalinstruments)‘My five moments for hand hygiene’Table IISee comment (2) ‘Before asepticIf moving froma contaminated body site task’to a clean body site duringpatient care (IB)15(continued on next page)
16Table II (continued )MomentEndpoints of nk to WHO Guidelines for Hand Hygiene in Health Care27WHO recommendation(ranking for scientificevidencea)4After patientcontactDonor surface: anysurface in thepatient zone withtouching a patient.Receptor surface:any surface in thehealthcare zoneHealthcareworker crosscolonisation;environmentcontaminationShaking hands, helping a patient Before and after touchingpatients (IB)to move around, gettingwashed, taking pulse, bloodpressure, chest auscultation,abdominal palpation5After contactwith patientsurroundingsDonor surface: anysurface in thepatient zonewithout touchingthe patient.Receptor surface:any surface in thehealthcare zoneHealthcareworker crosscolonisation;environmentcontaminationChanging bed linen, perfusionspeed adjustment, monitoringalarm, holding a bed rail,clearing the bedside tableAfter contact withinanimate objects(including medicalequipment) in theimmediate vicinity of thepatient (IB)CommentsSee comment (1) ‘Before patientcontact’Retained to cover all situationswhere the patient’s immediate andpotentially contaminatedenvironment is touched but not thepatientaRanking system for evidence according to WHO guidelines27: category IA, strongly recommended for implementation and strongly supported by well-designed experimental, clinical,or epidemiological studies; category IB, strongly recommended for implementation and supported by some experimental, clinical, or epidemiological studies and a strong theoreticalrationale.H. Sax et al.
‘My five moments for hand hygiene’17from patient X, minimises the risk of disseminationto the healthcare environment, and protects theHCWs themselves. It is noteworthy that HCWsusually touch an object within the patient zoneand not the patient before leaving. Hence, theterm ‘after patient contact’ is somewhat misleading and should be understood as ‘after contact withthe patient or his/her immediate surroundings’.of a unified visual to represent the point of careof any type of patient. The zones, critical sitesand moments for hand hygiene action are arrangedaround this patient to depict the infectious risksand the corresponding moments for hand hygieneaction in time and space.Moment 5: After contact with patientsurroundingsThere are important interpersonal differences inthe most effective learning styles. Some individuals respond better to conceptual grouping andwill respond well to the risk-based construct ofzones and critical sites and the five moments forhand hygiene. For most, however, the rationalbackground of a concept is a strong motivator. It isthus helpful to make very clear the reason for eachof the five moments for hand hygiene (Table II).Others respond better to circumstantial cues andit is useful to list the most frequent examples occurring in the specific care setting. The approachalso offers many possibilities for the developmentof training tools, including on-site accompaniedlearning kits, computer-assisted learning, andoff-site simulators.The fifth moment for hand hygiene is a variant ofmoment 4. It occurs after hand exposure to anysurface in the patient zone but without touchingthe patient. This typically extends to objectscontaminated by the patient flora that are extracted from the patient zone to be decontaminated or discarded. Because hand exposure topatient objects without physical contact with thepatients is associated with hand contamination,hand hygiene is required.Coincidence of two moments for handhygieneTwo moments for hand hygiene may sometimes falltogether. Typically this occurs when going fromone patient to another without touching anysurface outside the corresponding patient zones.Naturally, a single hand hygiene action will coverthe two moments for hand hygiene.Practical applications of the modelA multi-modal approach to hand hygiene promotion has been found to be the most efficienttechnique to increase patient safety in a sustainedway.8,21,27,56,57 A robust description of the criticalmoments for hand hygiene is important for thevarious elements of a multi-modal strategy including training, workplace reminders, ergonomiclocalisation of hand rub at the point of care, performance assessment by direct observations, andreporting.Understanding and visualsA critical feature to facilitate the understandingand communication of ‘My five moments for handhygiene’ lies in its strong visual message (Figure 2).The objective was to represent the ever-changingsituations of care into pictograms that could servea wide array of purposes and healthcare settings.The model depicts a single patient in the centreTrainingMonitoringDirect observation is the gold standard to monitorcompliance with optimal hand hygiene practice.27The five-moments model can be instrumental inseveral ways. Many care activities do not followa standard operating procedure. Thus, it is difficultto define the crucial moment for hand hygiene.The concept lays a reference grid over these activities and minimises inter-observer variation. OnceHCWs are proficient in the concept, they are ableto become observers with minimal additionaleffort, thus cutting down on training costs.58Furthermore, the concept solves the typical problems of clearly defining the denominator as anopportunity and the numerator as a hand hygieneaction.ReportingReporting results of hand hygiene observation toHCWs is an essential element of multi-modalstrategies to improve hand hygiene practices.21,27,59 Therefore, reporting details on riskspecific hand hygiene performance may increasethe impact of any feedback and make it possibleto monitor progress in a meaningful way thatfully corresponds to training and promotionalmaterial.
18DiscussionHand hygiene as it is understood today requiresthree to 30 applications of hand rub per hourduring patient care which translates to one handrub application up to every 2 min during intensivecare activities.3,4,6e8,11,21,27,59 The reality, however, is that unobserved HCWs only perform veryfew hand hygiene actions during their work day.The magnitude of the task of fixing this substandard quality of care has challenged infection control professionals worldwide for many years.60,61Various indications for hand hygiene during carehave been described in the scientific literature but,to date, there are few studies which focus in detailon practical issues within the framework of observation.62,63 We describe a new model for handhygiene that is intended to meet the needs fortraining, observation, and performance reportingacross all healthcare settings worldwide. Themodel ‘My five moments for hand hygiene’ was created to bridge the gap between the results of scientific studies and evidence-based guidelines and thenecessity to provide user-centred, practical tools.It is based on available evidence in the fields of microbiology and infectious diseases, a long-standingpractical experience in hand hygiene research andpromotion, and several years of a trial-and-errorprocess.21 Principles and recent insight in the threeoverlapping domains of human factors engineering,behaviour science and social marketing were usedto craft the concept for optimal performance atminimal cost.The importance of human factors design andergonomics for patient safety is increasingly beingrecognized.64e66 What has led to a 100-fold decrease in aeroplane crashes is now being progressively implemented in healthcare: a deliberatedesign process to avoid human error by streamlining processes and work environment to intuitivehuman understanding, behaviour and limitations.Building on this understanding, we provide a concept that applies to the complex and unpredictabletask of healthcare delivery and serves as a solid basis for the engineering of the necessary implementation tools.Behavioural science is used in human factorsengineering. According to cognitive behaviourmodels, intention to perform any action is motivatedby positive outcome evaluation, social pressure, andthe perception of being i
REVIEW 'My five moments for hand hygiene': a user-centred design approach to understand, train, monitor and report hand hygiene H. Saxa,b, B. Allegranzib,I.Uc kay a, E. Larsonb,c, J. Boyceb,d, D. Pitteta,b,* a Infection Control Programme, University of Geneva Hospitals, Geneva, Switzerland b Global Patient Safety Challenge, World Alliance for Patient Safety, World Health Organization,