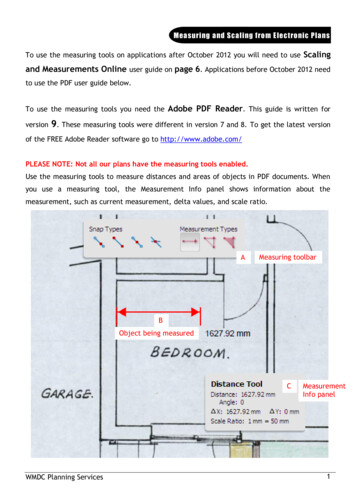
Transcription
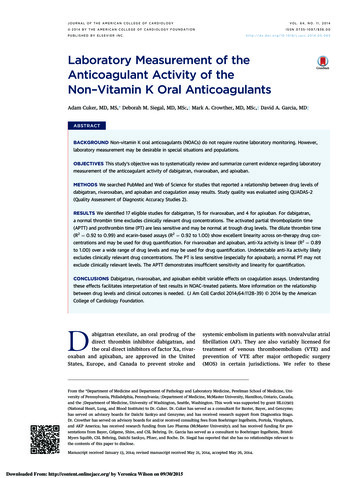
JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGYVOL. 64, NO. 11, 2014ª 2014 BY THE AMERICAN COLLEGE OF CARDIOLOGY FOUNDATIONISSN 0735-1097/ 36.00PUBLISHED BY ELSEVIER boratory Measurement of theAnticoagulant Activity of theNon–Vitamin K Oral AnticoagulantsAdam Cuker, MD, MS,* Deborah M. Siegal, MD, MSC,y Mark A. Crowther, MD, MSC,y David A. Garcia, MDzABSTRACTBACKGROUND Non–vitamin K oral anticoagulants (NOACs) do not require routine laboratory monitoring. However,laboratory measurement may be desirable in special situations and populations.OBJECTIVES This study’s objective was to systematically review and summarize current evidence regarding laboratorymeasurement of the anticoagulant activity of dabigatran, rivaroxaban, and apixaban.METHODS We searched PubMed and Web of Science for studies that reported a relationship between drug levels ofdabigatran, rivaroxaban, and apixaban and coagulation assay results. Study quality was evaluated using QUADAS-2(Quality Assessment of Diagnostic Accuracy Studies 2).RESULTS We identified 17 eligible studies for dabigatran, 15 for rivaroxaban, and 4 for apixaban. For dabigatran,a normal thrombin time excludes clinically relevant drug concentrations. The activated partial thromboplastin time(APTT) and prothrombin time (PT) are less sensitive and may be normal at trough drug levels. The dilute thrombin time(R2 ¼ 0.92 to 0.99) and ecarin-based assays (R2 ¼ 0.92 to 1.00) show excellent linearity across on-therapy drug concentrations and may be used for drug quantification. For rivaroxaban and apixaban, anti-Xa activity is linear (R2 ¼ 0.89to 1.00) over a wide range of drug levels and may be used for drug quantification. Undetectable anti-Xa activity likelyexcludes clinically relevant drug concentrations. The PT is less sensitive (especially for apixaban); a normal PT may notexclude clinically relevant levels. The APTT demonstrates insufficient sensitivity and linearity for quantification.CONCLUSIONS Dabigatran, rivaroxaban, and apixaban exhibit variable effects on coagulation assays. Understandingthese effects facilitates interpretation of test results in NOAC-treated patients. More information on the relationshipbetween drug levels and clinical outcomes is needed. (J Am Coll Cardiol 2014;64:1128–39) 2014 by the AmericanCollege of Cardiology Foundation.Dabigatran etexilate, an oral prodrug of thesystemic embolism in patients with nonvalvular atrialdirect thrombin inhibitor dabigatran, andfibrillation (AF). They are also variably licensed forthe oral direct inhibitors of factor Xa, rivar-treatment of venous thromboembolism (VTE) andoxaban and apixaban, are approved in the Unitedprevention of VTE after major orthopedic surgeryStates, Europe, and Canada to prevent stroke and(MOS) in certain jurisdictions. We refer to theseFrom the *Department of Medicine and Department of Pathology and Laboratory Medicine, Perelman School of Medicine, University of Pennsylvania, Philadelphia, Pennsylvania; yDepartment of Medicine, McMaster University, Hamilton, Ontario, Canada;and the zDepartment of Medicine, University of Washington, Seattle, Washington. This work was supported by grant HL112903(National Heart, Lung, and Blood Institute) to Dr. Cuker. Dr. Cuker has served as a consultant for Baxter, Bayer, and Genzyme;has served on advisory boards for Daiichi Sankyo and Genzyme; and has received research support from Diagnostica Stago.Dr. Crowther has served on advisory boards for and/or received consulting fees from Boehringer Ingelheim, Portola, Viropharm,and AKP America; has received research funding from Leo Pharma (McMaster University); and has received funding for presentations from Bayer, Celgene, Shire, and CSL Behring. Dr. Garcia has served as a consultant to Boehringer Ingelheim, BristolMyers Squibb, CSL Behring, Daiichi Sankyo, Pfizer, and Roche. Dr. Siegal has reported that she has no relationships relevant tothe contents of this paper to disclose.Manuscript received January 13, 2014; revised manuscript received May 21, 2014, accepted May 26, 2014.Downloaded From: http://content.onlinejacc.org/ by Veronica Wilson on 09/30/2015
Cuker et al.JACC VOL. 64, NO. 11, 2014SEPTEMBER 16, 2014:1128–391129Laboratory Testing of Anticoagulantsagents collectively as non–vitamin K oral anticoagu-calibration standards and 1 or more clinicalABBREVIATIONSlants (NOACs) in this paper. Synonymous termscoagulation assays, were eligible for inclu-AND ACRONYMSpreferred by other researchers include direct-actingsion. We excluded animal studies, abstractsoral anticoagulant agents and new, novel, or target-only, and non–English language publications.ACT activated clotting timeAF atrial fibrillationspecific oral anticoagulant agents (1).Unlike warfarin and other vitamin K antagonists(VKAs), the NOACs are administered in fixed doses anddo not require routine laboratory monitoring (2–4).However, measurement of their anticoagulant activity may be desirable in special clinical settings suchas bleeding; the pre-operative state; breakthroughthrombosis; and suspected overdose, noncompliance, or drug interactions and in certain populations,including those with extremes in body weight andin the elderly and patients with renal insufficiencyin whom there is a risk of drug accumulation.Assessment of anticoagulant effect may also beimportant in patients with AF presenting with acuteischemic stroke before administration of thrombolytic therapy (5).DATA EXTRACTION. We extracted key char-acteristics from eligible studies and recordedAPTT activated partialthromboplastin timethem in an evidence table. These includedECA ecarin chromogenicauthor, year of publication, setting, NOACassay(i.e., dabigatran, rivaroxaban, or apixaban),ECT ecarin clotting timereference method for measurement of drugNOAC non–vitamin K orallevels, range of drug concentrations studied,anticoagulanttest material (i.e., ex vivo patient plasma,PiCT prothrombinase-ex vivo healthy control plasma, or spikednormal plasma), dose (for studies usingex vivo plasma only), indication (for studiesusing ex vivo patient plasma only), numberof samples (for studies using individual[i.e., unpooled] plasma only), coagulationinduced clotting timePOC point of carePT/INR prothrombin time/international normalized ratioTT thrombin timeVKA vitamin K antagonistassays and reagents, and descriptors of the relationship between drug level and coagulation assay (e.g.,R2 values, range of linearity).SEE PAGE 1140QUALITY ASSESSMENT. Study quality was evaluatedNumerous studies on use of coagulation assays forusing QUADAS-2 (Quality Assessment of Diagnosticmeasurement of NOAC activity have been publishedAccuracy Studies 2), a standardized tool for qualityrecently, although a systematic review has not beenassessment of studies of diagnostic accuracy. The toolundertaken. The objective of our analysis was tocomprises 4 domains: patient selection, index test,summarize current evidence regarding laboratoryreference standard, and flow and timing. Risk of biasmeasurement of NOAC anticoagulant activity and tois assessed across all domains; the first 3 domains areprovide evidence-based guidance to practicing car-also assessed with respect to applicability to clinicaldiologists on the interpretation of coagulation tests inpractice (7).NOAC-treated patients.RESULTSMETHODSDABIGATRAN. Dabigatran etexilate, an oral non-LITERATURE SEARCH. We performed a systematicpeptide prodrug, is rapidly converted to the activereview of the literature to examine current evi-drug dabigatran by ubiquitous esterases. Dabigatrandence for laboratory measurement of the NOACs.directly inhibits both free and clot-bound thrombin.A search of PubMed and Web of Science from incep-It has relatively poor bioavailability (approximatelytion through December 1, 2013, was undertaken6.5%) and is eliminated predominantly by the kidneysseparately(80%). In individuals with normal renal function, thefordabigatran,rivaroxaban,andapixaban using the following key words: “name ofdrug” AND ((laboratory measurement) OR (laboratoryhalf-life of dabigatran is 12 to 14 h. Prolonged clearance and bioaccumulation are observed in patientsmonitoring)).with renal insufficiency (8). In patients with non-STUDY SELECTION. Articles were examined, first byvalvular AF and normal kidney function, the dose istitle and abstract and then by review of the complete150 mg twice daily, which is reduced in patients withpaper as indicated. Additional articles were sought byrenal insufficiency.reviewing bibliographies. Liquid chromatography/Peak levels of dabigatran occur 2 to 3 h aftertandem mass spectrometry (LC-MS/MS) is the refer-ingestion. Steady-state peak and trough concentra-ence method for measurement of the plasma con-tions in patients with AF and normal renal functioncentration of NOACs (6). Studies that reported thetaking dabigatran 150 mg twice daily are shown inrelationship between drug (or active metabolite)Table 1 (8). Substantial interindividual variability inlevels in human plasma, as measured directly usingdrug exposure is observed. In the PETRO (Preven-LC-MS/MS or indirectly using LC-MS/MS–validatedtion of Embolic and Thrombotic Events in PatientsDownloaded From: http://content.onlinejacc.org/ by Veronica Wilson on 09/30/2015
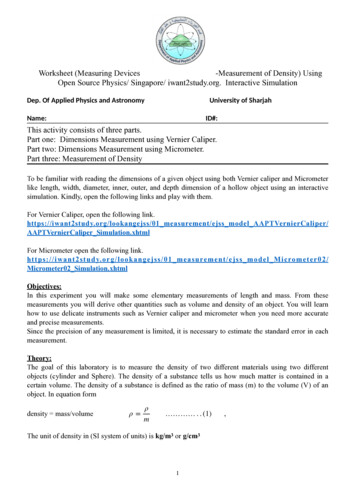
1130Cuker et al.JACC VOL. 64, NO. 11, 2014SEPTEMBER 16, 2014:1128–39Laboratory Testing of AnticoagulantsS t u d y s e l e c t i o n . Our literature search yielded 160T A B L E 1 Expected Steady-State Peak and Trough Concentrationsof Dabigatran, Rivaroxaban, and Apixaban Derived Fromarticles. Nine additional references were identifiedPharmacokinetic Studiesfrom bibliographies. A total of 152 articles wereDrugDabigatranStudyPopulationDose150 mg bid Patients with AFexcluded: 135 did not report an original researchPeak, Trough,ng/ml ng/mlRef. #study, 14 did not report drug levels measured by184*90*(9,10)LC-MS/MS, and 3 were published as abstracts only.Rivaroxaban 20 mg qdPatients with AF274†30†(33)The remaining 17 articles (11–27) met eligibilityApixabanHealthy malevolunteers129‡50‡(52)criteria (Figure 1). Eligible studies were collectively5 mg bidconducted in 9 different countries across a range ofdabigatran concentrations from 0 to 1,886 ng/ml.Only standard doses approved for AF are shown. *Median. †Median estimated bymathematical modeling. ‡Mean.Only 4 studies used ex vivo plasma from dabigatran-AF ¼ atrial fibrillation; bid ¼ twice daily; qd ¼ once daily.treated patients; the remainder involved ex vivohealthy volunteer plasma or normal plasma spikedinvitrowithdabigatranasthetestmaterial(Table 2).With Persistent Atrial Fibrillation) study, the rangeA c t i v a t e d p a r t i a l t h r o m b o p l a s t i n t i m e . Twelvecentrations in patients taking 150 mg twice dailyeligible studies reported a relationship betweenwas 64 to 443 ng/ml and 31 to 225 ng/ml, respec-the activated partial thromboplastin time (APTT)tively (9,10).and dabigatran levels. Three used ex vivo patientIdentification(5th to 95th percentile) in peak and trough con-Dabigatran160 articlesidentified bydatabasesearch9 articlesidentified bybibliographyreviewRivaroxaban134 articlesidentified bydatabasesearchScreening169 articles screened135 excluded: Review (n 114) Case report (n 9) Guideline (n 7) Editorial (n 5)IncludedEligibility34 articles reviewedby full-text17 excluded: Abstract only (n 3) Relationship withreference methodnot reported (n 14)17 articles includedin analysis2 articlesidentified bybibliographyreview136 articles screened108 excluded: Review (n 98) Case report (n 2) Guideline (n 4) Editorial (n 1) Other (n 3)28 articles reviewedby full-text13 excluded: Abstract only (n 1) Relationship withreference methodnot reported (n 12)15 articles includedin analysisApixaban70 articlesidentified bydatabasesearch3 articlesidentified bybibliographyreview73 articles screened68 excluded: Review (n 55) Guideline (n 2) Editorial (n 7) Other (n 4)5 articles reviewedby full-text1 excluded: Abstract only (n 1)4 articles includedin analysisF I G U R E 1 PRISMA DiagramThis PRISMA (Preferred Reporting Items of Systematic Reviews and Meta-Analyses) flow diagram illustrates dabigatran, rivaroxaban, andapixaban literature searches.Downloaded From: http://content.onlinejacc.org/ by Veronica Wilson on 09/30/2015
Cuker et al.JACC VOL. 64, NO. 11, 2014SEPTEMBER 16, 2014:1128–39Laboratory Testing of AnticoagulantsT A B L E 2 Characteristics of Eligible Dabigatran StudiesRef. #SettingRange of DrugConcentrations,ng/mlTest MaterialIndication (n)Dose, mg(10)GermanyNREx vivo patient plasmaMOS (287)12.5–300 bid;150–300 qd(11)GermanyNREx vivo healthy volunteer plasmaNA (80)10–400 SD;50–400 tid(12)GermanyNREx vivo healthy volunteer plasmaNA (35)150 bid(13)Sweden0–1,000Spiked normal pooled plasmaNA (NA)(14)United States0–500Spiked normal pooled plasma(15)United States,United ��0.850.60–0.86APTTECTNRNRNAAPTTPT/INRNRNRNA (NA)NAAPTTDilute TTTT0.95*0.98NRSpiked normal pooled plasmaNA (NA)NAAPTTPT/INRTT0.960.99NR4.7–943Spiked normal pooled plasmaNA (NA)NAAPTTDilute PTDilute TTECAECTPiCTPT/INRTTAustria0–480Spiked normal pooled plasmaNA (NA)NAAPTTPT/INRNRNR(18)Germany0–1,000Spiked normal pooled plasmaNA (NA)NAAPTTECTPT/INRNRNRNR(19)New 2)Sweden(23)United States0–500(24)United States18–487(25)Sweden(26)Finland30–960 00NRNRNRSpiked normal pooled plasmaNA (NA)NADilute TTNRSpiked normal pooled plasmaNA (NA)NADilute TT0.99Spiked healthy volunteer plasmaNA (4)NAPOC-INRPT/INRNRNREx vivo patient plasmaAF (70)NRAPTTDilute TTECAPT/INR0.580.970.960.48Ex vivo patient plasmaSpiked normal pooled plasmaAF (NR)VTE (NR)NA (NA)150 bidNADilute TTECA0.96–0.970.99Ex vivo patient plasmaAF (29)VTE (6)NRACTAPTTDilute 0.60–0.860.75–0.97Spiked normal pooled plasmaNA (NA)NAPT/INRNRSpiked normal pooled plasmaNA (NA)NAAPTTPT/INRTTNRNRNR*Relationship described by second-order polynomial regression.ACT ¼ activated clotting time; APTT ¼ activated partial thromboplastin time; ECA ¼ ecarin chromogenic assay; ECT ¼ ecarin clotting time; INR ¼ international normalized ratio; MOS ¼ majororthopedic surgery; NA ¼ not applicable; NR ¼ not reported; PiCT ¼ prothrombinase-induced clotting time; POC ¼ point of care; PT ¼ prothrombin time; SD ¼ single dose; tid ¼ 3 times daily;TT ¼ thrombin time; VTE ¼ venous thromboembolism; other abbreviations as in Table 1.plasma, 2 ex vivo healthy volunteer plasma, and 7up to a concentration of 200 to 300 ng/ml and thennormal plasma spiked with dabigatran in vitroflattened out at higher drug levels (17,28). This(Table 2). Dabigatran prolonged the APTT in acurvilinear relationship did not permit quantitativeconcentration-dependent manner in both ex vivoassessment of dabigatran levels, particularly atand in vitro studies. The dose response was linearhigher concentrations.Downloaded From: http://content.onlinejacc.org/ by Veronica Wilson on 09/30/20151131
1132Cuker et al.JACC VOL. 64, NO. 11, 2014SEPTEMBER 16, 2014:1128–39Laboratory Testing of AnticoagulantsCommercial APTT reagents differ widely in theirT h r o m b i n t i m e . Six studies reported a relationshipsensitivity to dabigatran. The APTT of plasma spikedbetween thrombin time (TT) and dabigatran levelswith dabigatran 120 ng/ml ranged from 26.0 to(Table 2). The TT (in unmodified form) was inordi-91.9 s in a cross-validation study of 9 different APTTnately sensitive in both ex vivo and in vitro studies.methods (27). These findings suggest that coagulationDepending on the reagent, dabigatran concentrationslaboratories should perform dose-response studiesof as little as 25 and up to 150 ng/ml exceeded theusing calibration standards to determine the sensi-limits of detection (15–17,28).tivity of their particular APTT method to dabigatranD i l u t e T T . In the dilute TT assay, the excessiveand communicate the results to clinicians. The leastsensitivity of the TT is overcome by diluting thesensitive reagents required a dabigatran concentra-plasma sample (21). Seven studies reported a rela-tion of approximately 400 ng/ml to produce a 2-foldtionship between the dilute TT and dabigatran con-prolongation in the APTT over control (19). Thecentration (Table 2). Two studies used an in-houseAPTT may not be prolonged in the presence ofmodification of the TT (15,20); 5 used the HEMO-typical on-therapy trough levels (Table 1), particularlyCLOT thrombin inhibitor assay (HYPHEN BioMed,if a relatively insensitive reagent is used. In a studyNeuvillesur-Oise, France), a commercially availableof ex vivo plasma from patients taking dabigatrandilute TT test (17,21,23–25). Dabigatran prolonged the150 mg twice daily, 18% of participants had a normalassay in a concentration-dependent manner. TheAPTT at trough (25). In another study of patients withrelationship showed a high degree of linearity, withAF, some samples had an APTT within the normalR 2 values ranging between 0.92 and 0.99 in bothrange despite dabigatran concentrations as high asin vitro and ex vivo studies. The lower limit of60 ng/ml (23).detection according to the manufacturer is 50 ng/mlnormalized(21). Two studies determined the assay to be lessr a t i o . Eleven studies reported a relationship be-accurate and more variable at concentrations belowtween dabigatran levels and the prothrombin time/50 to 100 ng/ml (15,21). The dilute TT is currently notinternational normalized ratio (PT/INR). Eight usedwidely available; in a recent survey in Australia andspiked plasma, 2 ex vivo patient plasma, and 1 ex vivoNew Zealand, only 9 of 592 laboratories reportedProthrombintime/internationalplasma from healthy volunteers (Table 2). Dabigatranusing it (29).prolonged the PT in a concentration-dependentE c a r i n - b a s e d a s s a y s . Ecarin is a snake venom thatmanner, as defined by an exponential (i.e., non-cleaves prothrombin to form meizothrombin, an un-linear) relationship (17). The PT/INR was less sensi-stable intermediate of thrombin. Dabigatran inhibitstive to dabigatran than the APTT. In an ex vivothe thrombin-like activity of meizothrombin (24).study of patients with AF, an INR of 1.2 or greaterTwo assays use ecarin as an activator: the ecarinwas only observed with dabigatran concentrationsclotting time (ECT) and ecarin chromogenic assayin excess of 400 ng/ml (23).(ECA).As with APTT, commercial PT reagents differ inSix studies reported a relationship between ECTtheir sensitivity to dabigatran. In a survey of 71and dabigatran levels (Table 2). Both in vitro andcoagulation laboratories, the PT of plasma spiked to aex vivo studies demonstrated a high degree of line-concentration of 300 ng/ml ranged from 15.7 to 50.2 s,arity, with R2 values ranging between 0.92 and 1.00.depending on the reagent (27). PT may be measuredLoss of linearity was observed in 2 studies at dabiga-using 2 assay types. The Quick method is influencedtran levels in excess of 470 to 500 ng/ml (17,19). Aby the entire extrinsic and common pathways ofrelationship between ECA and drug levels was re-coagulation, whereas the Owren method is affectedported in 4 studies (Table 2). The relationship wasonly by factors II, VII, and X. In studies of spikedlinear, with R 2 values of 0.94 to 0.99 in in vitro andplasma, Quick PT reagents were more sensitive toex vivo samples. One study identified greater vari-dabigatran than Owren reagents (14,27).ability at dabigatran concentrations 50 ng/ml (23).Point-of-care devices are available for measuringThe ECT and ECA are hampered by lack of standardi-the INR (POC-INR) in whole blood in VKA-treatedzation, variability in sensitivity to dabigatran amongpatients. In one study assessing the relationshipdifferent lots of ecarin, and limited availability (17,20).between dabigatran levels and a single POC-INROthersystem, the POC system yielded INR values 2- tolevel and the dilute PT, prothrombinase-induced4-fold higher than those obtained using a laboratoryclotting time (PiCT), and activated clotting timePT/INR method. Dabigatran concentrations 500(ACT) were each reported in a single study. Both theng/ml were beyond the POC system’s limit ofdilute PT and PiCT evinced a complex nonlineardetection (22).dose-response curve (17). As with heparin, the ACTDownloaded From: http://content.onlinejacc.org/ by Veronica Wilson on 09/30/2015a s s a y s . Relationships between dabigatran
Cuker et al.JACC VOL. 64, NO. 11, 2014SEPTEMBER 16, 2014:1128–39Laboratory Testing of Anticoagulantsproved insensitive to lower concentrations of dabi-references were identified from bibliographies. Wegatran. In an ex vivo study, the ACT was normal inexcluded 121 articles: 108 did not report an original40% of trough samples despite on-therapy dabigatranresearch study, 12 did not report a relationship be-levels (25).tween a coagulation assay and drug levels measuredRIVAROXABAN. Rivaroxaban is an oral inhibitor ofby LC-MS/MS, and 1 was published as an abstractfree and clot-associated factor Xa through reversible,only. The remaining 15 articles (27,37–50) met eligi-competitive interactions with its active site (30).bility criteria (Figure 1). Rivaroxaban concentrationsBioavailability following oral administration is dosein eligible studies ranged from 0 to 1,000 ng/ml.dependent (80% to 100% following a 10-mg dose;Four studies used ex vivo plasma from rivaroxaban-66% following a 20-mg dose). It is highly bound totreated patients, 1 incorporated ex vivo plasma fromplasma proteins ( 90%) (31); plasma levels peak 2 tohealthy controls, and the remainder used normal4 h following oral administration (32,33). Partiallyplasma spiked in vitro with rivaroxaban (Table 3).excreted by the kidneys (36%), rivaroxaban has aP r o t h r o m b i n t i m e . We found 11 studies evaluatinghalf-life of 6 to 13 h depending on dose and agethe effect of rivaroxaban on PT (Table 3). In general,(31–35). Table 1 shows expected peak and troughrivaroxaban prolonged the PT in a concentration-plasma concentrations in patients with AF treateddependent, linear fashion in plasma spiked withwith 20 mg daily (36).rivaroxaban and in plasma from patients receivingyieldedrivaroxaban for approved indications. On-therapy134 unique rivaroxaban articles. Two additionalrivaroxaban concentrations showed a modest effectStudys e l e c t i o n . OurliteraturesearchT A B L E 3 Characteristics of Eligible Rivaroxaban StudiesRef. #(26)SettingEuropeRange of DrugConcentration,ng/ml60–305Test MaterialIndication (n)Dose, mgCoagulationTestR2NRNRNRSpiked normal pooled plasmaNA (NA)NAAnti-XaAPTTPT/INR(36)United States, Canada 10– 1,000Spiked normal pooled plasmaNA (NA)NAPT/INR(37)France0–1,000Spiked normal pooled plasmaNA (NA)NAAnti-XaAPTTDilute PTDilute R1.000.99–1.00(38)FranceNREx vivo patient plasmaMOS and100–70040–150(43)Germany1.9–283.0(44)the Netherlands0–1,00010 qdNRSpiked normal pooled plasmaNA (NA)NAAnti-XaNRSpiked normal pooled plasmaNA (NA)NAAnti-XaAPTTPT/INRNRNRNRSpiked normal pooled plasmaNA (NA)NAPT/INRNREx vivo healthy volunteer plasmaSpiked normal pooled plasmaNA (20)NA (NA)10 qdNAAnti-Xa0.98–0.99Ex vivo patient plasmaMOS (80)10 qdAnti-Xa1.00Spiked normal pooled plasmaNA (NA)NAAnti-XaAPTTPT/INRNR1.001.00*(45)Europe, North America20–662Spiked normal pooled plasmaNA (NA)NAAnti-XaNR(46)Europe, North America19–643Spiked normal pooled plasmaNA (NA)NAPT/INRNR(47)the Netherlands0–800Spiked normal pooled plasmaNA (NA)NAPT/INR1.00(48)BelgiumNREx vivo patient plasmaAF, VTE (52)NRAnti-XaPT/INR0.950.58–0.66(49)FranceNREx vivo patient plasmaMOS (41)10 qdAnti-XaPT/INR0.99NR*Relationship described by second-order polynomial regression.RVVT ¼ Russell viper venom time; other abbreviations as in Tables 1 and 2.Downloaded From: http://content.onlinejacc.org/ by Veronica Wilson on 09/30/20151133
1134Cuker et al.JACC VOL. 64, NO. 11, 2014SEPTEMBER 16, 2014:1128–39Laboratory Testing of AnticoagulantsT A B L E 4 Characteristics of Eligible Apixaban StudiesSettingRange of DrugConcentration, ng/ml(36)United States, Canada 10– 1,000(53)Global1–933Ex vivo patient plasmaACS (1,691)(54)United States0–2,500Ex vivo healthy volunteer plasmaSpiked healthy volunteer plasmaNA (39)NA (21)(55)France0–1,000Spiked normal pooled plasmaNA (NA)Ref. #Test MaterialIndication (n)Ex vivo patient plasmaSpiked normal pooled plasmaVTE (348)NA (NA)Dose, mgCoagulationTestR25–10 bid, 20 qdNAAnti-XaPT/INR0.88–0.890.365–20 qdAnti-Xa0.9720 SDNAPT/INR0.41NAAnti-XaAPTTPT/INRNRNRNRACS ¼ acute coronary syndrome; other abbreviations as in Tables 1 and 2.on PT. Typical trough (41 to 60 ng/ml) and peaksamples. Investigators found a greater degree of(219 to 305 ng/ml) concentrations increased PT by 6%assay imprecision at higher rivaroxaban concentra-to 19% and 50% to 135%, respectively (27,38,42,47).tions (800 ng/ml) in one study (45). In a multicenterAssay sensitivity varied significantly among throm-study, both intralaboratory and interlaboratory pre-boplastin reagents. Interassay variability was reducedcision were satisfactory except at the lower limit ofby use of an international sensitivity index specificdetection (20 ng/ml); use of a centrally distributedfor rivaroxaban but not by conversion to an INRreagent reducedused for monitoring VKA therapy (38,42). TheseMathematical modeling also decreased interassayobservations suggest that coagulation laboratoriesvariability resulting from different sensitivities ofshould perform dose-response studies using calibra-individual reagents to rivaroxaban (40). When com-tion standards to determine the sensitivity of theirmercial anti-Xa assays were used with unfractionatedinterlaboratory variability(46).particular PT method for rivaroxaban and communi-or low-molecular-weight heparin (LMWH) calibratorscate the results to clinicians.(rather than rivaroxaban calibrators), the relationshipActivatedpartialthromboplastint i m e . Fiveremained linear up to a rivaroxaban concentration ofstudies evaluated the effect of rivaroxaban on APTT500 ng/ml (38,41).(Table 3). Whereas rivaroxaban prolonged APTT in aO t h e r a s s a y s . The relationship between rivaroxabandose-dependent manner, the overall relationshipconcentration and the dilute PT, dilute Russell viperbetween rivaroxaban concentration and APTT pro-venom time (dRVVT), and PiCT was evaluated inlongation was nonlinear, with studies reportinga single study (38). Researchers uncovered a linear,conflicting data regarding the concentration rangesdose-dependent relationship between rivaroxabanoverandwhich nonlinearitywasmost 1,45). Similar to PT results, there was significantdRVVT ratio (expressed as ratio vs. baseline) in avariability among reagents and among individualconcentration-dependent but nonlinear manner. Atlaboratories in a multicenter study (27,45). Hillarplow concentrations of rivaroxaban ( 200 ng/ml),et al. (41) reported that the APTT assay was insensi-there was a paradoxical shortening of PiCT, whereastive at the lowest drug level studied (25 ng/ml).PiCT was prolonged in a concentration-dependentA n t i - X a a c t i v i t y . Ten studies assessed the effectfashion at higher concentrations.of rivaroxaban on anti-Xa activity (Table 3). InAPIXABAN. Like rivaroxaban, apixaban is a small,general, the studies showed a linear, concentration-orally available, direct inhibitor of coagulation factordependent relationship between rivaroxaban con-Xa (51). It has 50% bioavailability and, in healthycentration and anti-Xa activity over a wide range ofvolunteers, reaches its maximum plasma concentra-concentrations (e.g., 20 to 660 ng/ml) when they weretion approximately 3 h after ingestion. Apixaban ismeasured using a standard curve generated withhighly protein bound in plasma, and concomitantrivaroxaban calibrators and controls with R 2 valuesfood intake has little impact on its pharmacokineticsranging from 0.95 to 1.00 (39,43,44,49,50). The cor-(52). Metabolized through multiple routes, apixabanrelation was less robust at concentrations 100 ng/mlis less dependent on renal clearance than dabigatran(49). However, Samama et al. (46) demonstrated thatand rivaroxaban. In persons with normal renallow rivaroxaban concentrations could be measuredfunction, apixaban has a half-life of approximatelywith a modified anti-Xa test using less diluted12 h (53). As measured by LC-MS/MS, the expectedDownloaded From: http://content.onlinejacc.org/ by Veronica Wilson on 09/30/2015
Cuker et al.JACC VOL. 64, NO. 11, 2014SEPTEMBER 16, 2014:1128–391135Laboratory Testing of Anticoagulantssteady-state concentrations of apixaban have beenex vivo patient samples. Concern about the applica-published by Frost et al. (52) and are shown inbility of these studies to clinical practice within theTable 1.patient selection domain was judged to be high. SomeS t u d y s e l e c t i o n . Our literature search for apixabanstudies examined assays not widely available to cli-yielded 70 articles; 3 additional references werenicians (e.g., ECA, ECT, dilute TT). Concern regardingidentified from bibliographies. Sixty-nine articlesapplicability of these studies to clinical practicewere excluded: 68 did not report an original researchacross the index test domain was judged to be high.study and 1 was published as an abstract only. TheBecause data correlating plasma NOAC levels andremaining 4 articles (37,54–56) met eligibility criteriaclinical outcomes are scarce, concern about the(Figure 1). Eligible studies collectively evaluatedapixaban across a range of concentrations from 0 to2,500 ng/ml (Table 4).Prothrombintime/internationalnormalizedT A B L E 5 Study Quality Assessment Using QUADAS-2 Criteriar a t i o . We found 3 studies th
centrations and may be used for drug quantification. For rivaroxaban and apixaban, anti-Xa activity is linear (R2 ¼ 0.89 to 1.00) over a wide range of drug levels and may be used for drug quantification. Undetectable anti-Xa activity likely excludes clinically relevant drug concentrations.