Transcription
The International Technology Management Review, Vol. 3 (2013), No. 2, 127-139Implementation of E-Health Record Systems and E-Medical Record Systems in ChinaXiangzhu Gao, Jun Xu, Golam Sorwar & Peter CrollSouthern Cross Business School, Southern Cross UniversityLismore, NSW 2480, AustraliaE-mail: xiangzhu.gao@scu.edu.auAbstractIn 2005, Chinese government defined its direction to electronic health records and electronic medical records. Up to2012, hundreds of electronic health record systems and electronic medical systems have been developed, but thesystems are still in their infancy, and China is facing a variety of challenges in implementation of the systems. Toovercome the challenges and achieve system benefits, recommendations are provided for implementing a nationalelectronic health system.Keywords: E-health, E-health Record System, E-medical Record System, China1. IntroductionFrom 2000 to 2010, Chinese population increased by5.84%, reaching 1.34 billion according to the 6thnational census1. To meet the needs of the healthcare forsuch a large population and to improve healthcareservices, China increased its annual health expendituredramatically by 335% from CN 460 billion in 2000 toCN 2000 billion in 2010, according to the Ministry ofHealth (MOH) of China2. Over these years thehealthcare infrastructure in China has been welldeveloped. In 2011 there were 954,389 healthinstitutions, including 21,979 hospitals, 918,000 grassroots or community health service centres (CHSCs), and11,926 specialised public health institutions. However,as China is a developing country with a largepopulation, China’s health expenditure per capita ismuch lower than that of developed countries. In 2008,China’s health expenditure per capita was US 146,contrasting US’s US 7,164, France’s US 4,966,Germany’s US 4,720, Canada’s US 4,445, Australia’sUS 4,180, UK’s US 3,771 and Japan’s US 3,1902. Tofurther improve its healthcare, China must improve theefficiency of its healthcare services while maintaininglower costs, in addition to the increase in governmentbudget.The Chinese government laid a focus on healthcaresector in its 12th Five-Year Plan (2011-2016). MOHdefined its 3521 project for e-health, where the ‘3’refers to three levels of healthcare data platform:country, province and region levels; the ‘5’ points tofive applications: public health, medical services, newrural medial insurance plan, basic drug plan, and generalmanagement; the ‘2’ indicates two systems: electronichealth record (EHR) system and electronic medicalrecord (EMR) system; and the ‘1’ represents one specialnetwork for healthcare3,4,5. Regarding the EHR andEMR, a health record is the information of healthconditions about a healthcare recipient6 at CHSCs orother health institutions, while a medical record is theinformation of hospital clinic and therapy about amedical care recipient7. EHRs are collected, stored andshared by regional CHSCs, while EMRs are recorded orgenerated, stored and shared by hospitals.The Chinese government leads the development ofEHR and EMR systems. The MOH approved theestablishment of professional committees for researchon and development of standards and specifications.The China Hospital Information ManagementAssociation (CHIMA) focuses on the preparation ofmanagement specification and regulations for digitalhospitalisation standards8. The Health InformationStandards Professional Committee (HISPC) of theMOH prepared a series of guidebooks, standards andspecifications for both EHR and EMR systems. InPublished by Atlantis PressCopyright: the authors127
X. Gao et al.addition, the government has developed supportive ehealth policies including national e-health policy,national multiculturalism policy for e-health, nationaltelemedicine policy, and e-government policy.China’s e-health system development is significantlyaffected by its economy, administration, geography,demography and culture. Economic development inChina is extremely unbalanced. Urban development isfaster than rural development, and growth in easternregions is faster than that in western regions. There isgrowing inequity in health status, resource allocationand service delivery between rural and urban areas9.The Chinese population is rapidly aging, due to a lowermortality rate and the one-child policy, which wasforced to implement in 1979. In 2010, rural residentswere over 674 million (50.32%); mobile population wasover 261 million (19.07%); and elderly residents over60 years old were over 177 million (13.26%)1. Thesefeatures have led to healthcare challenges for the centralgovernment, which announced a comprehensivehealthcare reform in 2009 to address the issues withouta detailed roadmap10.The healthcare reform boosted CHSCs in urbanareas to play an important role in prevention, medicalcare, rehabilitation and health promotion. The CHSCsare non-profit institutions, and their service targets arewomen, children, elderly people, chronically sick anddisabled people and poor residents in residencecommunities. The communities are partitioned based onthe administrative areas where households are registeredaccording to China’s household registration system. Ahousehold registration record includes the members of afamily as residents of an administrative area andidentifies each member’s information of name, gender,date of birth and the relationship with the householder(parent, spouse, etc.). The household registrationrecords, and the roles and targets of the CHSCs affectthe implementation of EHR systems.2. Current StatusAccording to CHIMA8 computerisation in hospitals inChina started in late 1980s. Some economicallyadvanced cities started to develop regional EHRsystems in 200211. In this paper, however, the authorsonly review relevant efforts and results since 2005 forthe reason that major activities and significant eventshave happened since then. The development of EHRand EMR systems in China is marked with thefollowing milestones. In 2005, the 5th Plenum of the 16th CommunistParty Central Committee passed its suggestion forthe 11th Five-Year Plan12, which directed thedevelopment of EHR systems and EMR systems. In 2006, the HISPC was established by the MOHfor standards creation, administrative certificationand application promotion13. In 2009, the MOH issued the Guidebook forCreating Regional Health Information PlatformBased on Electronic Health Records, whichdescribes operation flow, and information andfunctionality of the platform, providing IT vendorswith clear system requirements14. In 2009, a series of standards and specificationswere published by MOH, including Basic Structureand Data Standards for Health Records15, BasicDataset Compilation Specification for HealthRecords16, Common Data Elements in HealthRecords17, and Basic Dataset of PersonalInformation18. In 2009, Beijing, Shanghai, Guangzhou, Xiamen,and Hangzhou, which are economically advancedcities in China, saw their initial achievements inEHR system initiatives11. In 2010, MOH developed Basic Standard forElectronic Medical Records. In 2010, Shanghai, Zhejiang, Anhui, Chongqing,and Xinjiang, which are located from east throughwest in China, participated in testing EHR andEMR systems sponsored by MOH5. In 2011, the Guidebook for Creating IntegratedAdministration Platform for Health Records wasreleased by MOE, which includes functionalrequirements and design concepts for the Platform,and provides health administrators and decisionmakers with information support and service19. In 2011, the MOH published the Technical Solutionfor Developing Hospital Information PlatformBased on Electronic Medical Records20. In 2012, the MOH published the Specification forSharing Documents of Health Information6, and theSpecification for Sharing Documents of ElectronicMedical Records7.Published by Atlantis PressCopyright: the authors128
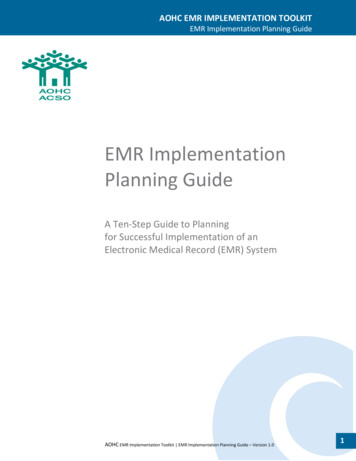
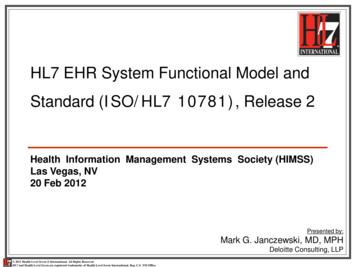
EHR/EMR Systems in China In 2012, the State Council21 published the 12thFive-Year Plan for Developing Health Services,which includes establishment of a national unifiedmedical and health information standard system.In planning for the EHR and EMR systems, Chinastudied international experiences from US, UK, Canada,Australia, etc. For example, China’s EMR systemsadopt the HL7 Standard20, which takes an importantposition in the US standard system and has become aninternational standard for medical informationexchange22. Because of the complexity of EHR systems,Australia has taken 3 stages to reach a national system:MediConnect, which was a pilot system23;HealthConnect, which consisted of seven regionalsystems24; and Personal Controlled Electronic HealthRecord (PCEHR) System, which is a national system25.China follows a similar procedure in deploying EHRsystems. Both local and international vendors haveprovided solutions for China’s EMR/EHR systems.Popular international vendors include IBM, Dell, Cisco,Siemens and Fujitsu, and main Chinese vendors areYonyou, DHC, Neusoft, B-Soft, Winning, Founder andJiangsu Zhongkang Software. Different hospitals usedifferent EMR systems26,27.By 2009, China had completed its pilot test of theEHR systems in major cities11. In 2010, fund isallocated for EHR initiatives in five provinces5. In thesestages of EHR attempts at regional and provinciallevels, some cities or provinces developed their ownstandards and systems. Based on these systems, theMOH developed standards and specifications forsubsequent stages. Until 2011, 120 EHR systems hadbeen completed, 40 systems were under developmentand 100 systems were in planning phase19. The 2009Guidebook14 required that by 2011 50% urban residentsand 30% rural residents will have their e-health recordsand by 2020 all residents will have their own e-healthrecords. The Minister of MOH declared on Feb 27,2012 that 900 million residents had created their healthrecords, accounting for 66% of the national population,and more than 50% of residents had created their ehealth records28. It is planned that 75% of urbanresidents will have their EHRs by 201521.The Basic Structure and Data Standards for HealthRecords15 defines that health records consist of personalinformation and the records of health services at healthservice institutions, including children’s health,women’s health, disease management, disease controland medical service. These are typical services providedby CHSCs, which are in charge of resident registrationwith and data entry to EHR systems. To meet MOH’stargets of EHR adoption, local governments encourageCHSCs to register residents by incentive perregistration. CHSCs visit residents at home or useresidents’ household information from local policestations. As the data are collected as a result ofadministrative intervention instead of the resultsrecorded when individuals receive health services, theinformation could be incomplete and inaccurate. Theauthors interviewed some residents in Beijing, Tianjin,Baoding, Dalian, Shenyang, Changchun and Wuhanduring October 2012 to January 2013, and found outthat none of them has personally accessed to EHRsystems, and most of them do not know EHR systems.Currently EHR systems are used by CHSCs to storehealth information of local residents in stand-alonecomputers.Governments at different levels have been workingon information exchange between communities byestablishing Regional Healthcare Information unication networks to share data and ities29. More efforts will be put into RHINs inthe coming years. For example, Jiangsu ZhongkangSoftware Co., Ltd. and Nantong University havedeveloped a Web platform (www.chinaehr.org)according to the Basic Structure and Data Standards forHealth Records15. The platform is designed to be usedby individuals and healthcare providers in JiangsuProvince and, possibly, other 12 provinces. Currentlythe platform invites medical doctors from CHSCs inNantong, Jiangsu to participate.Regarding EMR systems, there exist many standalone and scatted efforts across the country. IT vendorshave worked with hospitals to provide solutions forEMR systems. Reported examples include: IBM has developed a series of solutions, includingClinical and Medical Record Analysis and SharingSystem (CHAS) for a hospital in Guangdong30, andCloud Solution for sharing clinical data31. Cisco32 developed an Integrated Solution for DigitalHospitals for Peking University People’s Hospital.Published by Atlantis PressCopyright: the authors129
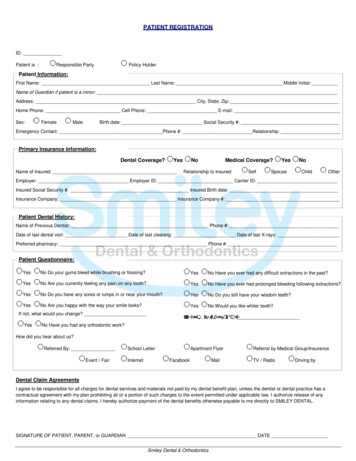
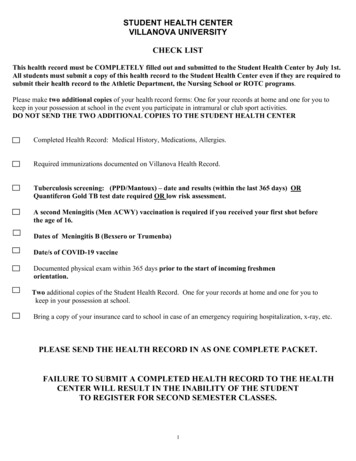
X. Gao et al. Dell provided its solution of virtual technology tohelp Xiamen University Zhongshan Hospitalupgrade its existing systems33.Early in 2008, 80% of hospitals had implemented ahospital information system of a kind. According toMOH2 there are 21,979 hospitals in China. This meansthat about 17,583 hospitals have installed or usedinformation systems for medical purposes or supportingactivities.Hospitals have developed EMR systems without aconsideration to share information with EHR systems.However, efforts have been made in sharing informationwith EMR systems when developing EHR systems bylocal governments. Xiamen has successfully attemptedthe association of an EHR system with an EMR system.In Xiamen’s system, which involves 95 medicalinstitutions and 60% of local residents, healthinformation, medical treatment records and check-upresults of a resident since birth are recorded in one datarepository34. Health Cards is another major projectrelating to connecting EHR and EMR. The system willlink hospitals, public health institutions, and insuranceoperations across China. Currently, the system has beenpiloted in Henan, Liaoning, Guangdong and InnerMongolia4.3. Challenges and Issues3.1. Insufficient Fund and Biased FundAllocationE-health projects are expensive35. For example, U.S.invested AU 28 billion (AU 1,320 per capita) in theBarack Obama Plan in five years, and Australia hasalready spent AU 466.7 million (AU 21 per capita) onthe first release of the PCEHR system in two years36.According to World Health Organization (WHO), lackof funding is one of the major hurdles affecting ehealthcare adoption in developing countries includingChina37. It is estimated that the required investment inhardware/software is CN 26 billion (CN 20 percapita)11,38. Normally hardware/software accounts for20% of the development cost39. Therefore developmentcost would be CN 130 billion (CN 100 per capita orAU 17 per capita). Generally speaking, the annual costto maintain an e-commerce or e-government system inits operation phase is between 50% and 200% of thecost for the development phase39. According to this rule,China needs CN 65 to CN 260 billion annually tomaintain the systems. Although the total healthcareexpenditure was CN 2000 billion in 2010, thegovernment contribution is CN 573 billion only1.Obviously, government healthcare budget cannotprovide sufficient fund for system operation.China has invested its limited fund for e-healthunevenly26,40. According to Ying41, 64.7% of the fundwas allocated to computer hardware. Contrasted withthe normal 20% cost by hardware/software, the largeproportion of fund for hardware indicates a lack ofresearch on and analysis of EHR and EMR systems.Moreover, while over 50% of the total population live inrural areas1, where healthcare infrastructure typicallylags behind, the government allocates 41% of its fundfor 2009-2011 to rural health29. The biased fundallocation poses more difficulties in implementing EHRor EMR systems in rural areas.3.2. Lack of Unified Planning and GovernanceHundreds of EHR and EMR systems are developed orare operating in different regions with no or little crossregion data sharing. There is not central governanceover regional development and unified planning for anational system. In 2004, the Chinese HealthInformation Society established the Health InformationStandardisation Professional Committee (CHISHISPC). In spite of the existence of CHIS-HISPC,MOH established its HISPC in 2006. The twocommittees are partly overlapped their roles and/orfunctionality. Although the MOH has issued standardsfor EHR and EMR systems, these standards are notclear and difficult to follow in practice42. Some regionalgovernments have developed local standards, hopingtheir efforts to become accepted as ‘golden pilots’29. Forexample Zhejiang Bureau of Quality and TechnicalSupervision43 developed the Technical Specification ofAccess Interface for Sharing Health Data.Because of the lack of unified national approach,clear planning and governance framework, the qualityof the EHR and EMR systems and the productivity ofthe development are low. A large amount of resourceshave been used for repetitive products that are isolatedfrom each other. The authors visited some hospitals inBeijing and CHSCs in Tianjin in 2012 and found thatnew patients have to fill in registration forms, whichPublished by Atlantis PressCopyright: the authors130
EHR/EMR Systems in Chinacapture different information at different hospitals, andresident health records are stored in CHSCs’ standalone computers.There is not general guidance and it is individualdoctors’ decision to share medical or health informationbetween medical or health institutions. Hospitals havenot formed positive attitude towards sharing informationfor reasons such as self-funded systems, propriety,concern of disclosing critical information to outsiders,and the fear of criticism by fellow professionals. Largeand metropolitan hospitals are typically not willing toshare information with their smaller counterparts orCHSCs even though the latter is keen on sharinginformation with the former. Doctors from largehospital tend not to recognise diagnosis and test resultsfrom smaller hospitals because of the concern aboutpersonnel’s proficiency and instrument’s accuracy.target. Data collected in haste may not be completeand/or accurate. However much information included inEHR systems can be obtained from EMR systems20,where information is obtained when patients visithospitals and therefore should be more accurate.In 2012, MOH6,7 published standards orspecifications for each of the two systems with anobjective of interaction between the two systems.However, beside the issue of interoperability,developing both EHR and EMR systems consumes theinsufficient resources while reinventing the wheel. Laterin the same year, the State Council21 planned toestablish a national unified medical and healthinformation standard system. However, there will beintegrity issue regarding data from the two legacysystems, which must be addressed now.3.5. Lack of Legislation and Regulation3.3. Lack of Willingness to Share InformationThere is not general guidance and it is individualdoctors’ decision to share medical or health informationbetween medical or health institutions. Hospitals havenot formed positive attitude towards sharing informationfor reasons such as self-funded systems, propriety,concern of disclosing critical information to outsiders,and the fear of criticism by fellow professionals. Largeand metropolitan hospitals are typically not willing toshare information with their smaller counterparts orCHSCs even though the latter is keen on sharinginformation with the former. Doctors from largehospital tend not to recognise diagnosis and test resultsfrom smaller hospitals because of the concern aboutpersonnel’s proficiency and instrument’s accuracy.3.4. Issue of Two Separate SystemsEHR systems and EMR systems are regarded asdifferent systems and operate in parallel respectively.EHRs are entered by CHSCs and EMRs are recorded inhospitals. Quality of data in EHR systems is uncertainbecause of unrealistic target that 50% urban residentsand 30% rural residents would have their EHRs by2011. The authors visited a CHSC, which takes chargeof 93,336 residents and stores their EHRs in a databasehosted in a stand-alone computer. If it takes 5 minutesto enter one person’s EHR, and data entry continues 8hours per day, it needs 486 working days to reach thePrivate data should be secret from non-expected users(secrecy), data should be available for meaningful use(necessity) and critical data must be correct and accurate(integrity), when data are stored in and transmittedbetween systems37. Even though security techniquessuch as authentication and encryption can address theseissues, legislation is necessary to define private data,and regulate meaningful use and trustful operation ofthe systems.Secrecy and necessity may conflict and must bebalanced in system analysis and design. Low level ofsecrecy increases the risk of privacy breach whileincreasing necessity, and low level of necessity maycause negative impacts on health44 while improvingsecrecy. Currently there is a lack of policy andregulation in China for recording, storing and usingpersonal health information11,37, and EHR and EMRsystems are developed and implemented withoutrelevant guidance. For example, EHR system users areidentified by national ID number, which includespersonal identifiable information of residence area anddate of birth, and individuals can access their EHRswith ID cards45.3.6. Issue of InteroperabilityEHR and EMR systems are complex and integratemultiple techniques46,47. China’s EHR and EMRsystems are developed by various vendors of softwarePublished by Atlantis PressCopyright: the authors131
X. Gao et al.firms, universities, research institutions, etc. Most ofthese systems are isolated. The aim of these systems isto meet specific needs of the healthcare institutions,including demographics, diagnosis and payment48without consideration for interoperability. China hasissued its standards, but interoperation of EHR or EMRsystems is more complex than standards could define,and software engineering solutions should be sought49.Moreover, the current standards should be improved.For example, the Basic Structure and Data Standards forHealth Records15 has some critical deficiencies in termsof privacy and security, support for different data typesand reference data, mechanism to support easy additionsand extensions to various medical domains andorganisations, and relational attributes for dataelements50.3.7. Issue of E-health Talent and ResearchHealth and medical informatics education and trainingin China cannot meet China’s need51. There is a lack ofskilled health IT professionals to develop health ITsolutions52 and the talent to combine ITknowledge/skills, healthcare, nursing and publichealth42,53. The authors noticed that it is difficult toobtain literature of theory on e-health in China. Thisindicates a lack of theory support for developing ehealth information systems in China, which is primarilygained from research38,54. Meanwhile, there is a need forEHR system education. According to Huang11, data forEHR systems are mainly collected in urbancommunities and rural villages from women, children,elderlies, chronically sick and disabled people, who arethe main targeted users of China’s EHR systems.Compared with others, this group of people is averagelyat lower levels in IT literacy. There is a need for EHRsystem education among these people.4. Recommendations and Outlook4.1. Developing a National System of HierarchicalStructureeventually build its national unified electronichealth/medical record (EH/MR) system. Because ofunbalanced economy across the country, insufficientfund and biased fund allocation, difference in regionalpolicies and difference in resources and organisations indifferent areas, the national EH/MR system shouldevolve in a top-down approach towards a hierarchicalstructure with 3 levels of country, province and region,as defined in the 3521 e-health project by MOH. Thesystem will be developed in object oriented (OO)approach55,56 to allow Inheritance – a child class at a lower level (provinceor region) inherits features and methods from itsparent class at a higher level (country or province)to ensure that a province or region carries outstandards, policies, etc. from the country or thegoverning province, and avoids repetition at lowerlevels; Overriding – a child class can implement themethods inherited from the parent class differentlyto ensure that a province or a region can bedifferent from another one at the same level; Encapsulation – a class is independent from othersto ensure that the change (participation, withdrawal,local reform, etc.) in the class will not affect otherclasses; and Polymorphism – objects in a class (institutions in aprovince or region) can have specificimplementation of user interfaces to ensure that thesystem is usable for different users includinghospitals, CHSCs and individuals.Figure 1.1 illustrates the class diagram of thenational unified system. The Country is the top levelclass. Province1 through ProvinceN are related to Nprovinces (including municipalities) in terms ofimplementing EH/MRs. If two or more provincesimplement EH/MRs in exactly the same way, they aretechnically regarded as one province. The Region1.1through RegionN.M are related to regions in respectiveprovinces. Because of the encapsulation, classes can beeasily added under a region class to adapt the EH/MRsystem to possible variety within regions.Although there are hundreds of EHR and EMR systems,these systems will have to be abandoned or upgradedeventually because of the challenges to and defects withthem. According to international experiences and the12th Five-Year Plan by State Council21, China willPublished by Atlantis PressCopyright: the authors132
CountryProvince1Province2EHR/EMR Systems in ChinaProvinceN Region1.1Region1.2Region2.1 RegionN.M Fig. 1. Hierarchical structure of the national EH/MR systemThe features of this approach areThe hierarchical structure conforms to China’sadministrative structure. The system is developed incrementally according tothe national e-health plan, and in order to meet thechallenge of insufficient funds. The system can beused at a higher level while it is developed for alower level. The system is maintainable to accommodateChina’s changing environments. The system is sustainable and will become simplerwith the change towards balanced economy andunbiased fund allocation.MOH will lead and govern the complete process ofsystem development and implementation, although localgovernments will be involved in timely stages. 4.2. Using Smart Cards at the Present Time Chinese people are used to keeping medical recordswith themselves. They had a history to keepmedical records by individuals before computersare used to store the records.They are used to using smart cards. Most people areusing medical insurance cards and other types ofcards.Smart cards are cost-effective and easy to use58.The smart cards do not need computer networks,except for cards and card readers.Smart cards can store more complete and betterquality data, which may be integrated from multipleinstitutions59. When inconsistency is noticed,human intervention will fix errors.Card holders control the access to theirEHRs/EMRs.Smart cards are in practice impossible to forge orunlawfully manipulate. Strong offline and/or onlineverification (PIN or biometric) limits the unlawfuluse of lost or stolen cards to gain access tohealthcare58.The smart cards will be the media from whichEH/MRs are transferred to the national system inthe future.4.3. Establishing Incentive MechanismCitizens will participate in the national system atdifferent stages of the system development, which maytake years of time. According to State Council21, thenumber of individual EHR users will increase from 50%to 75% of the residents from 2012 to 2015. Based onthis rate, it is estimated that all residents will use EHRsin 2018, when the national system evolves to becomplete. In the next 5 years, people need to use currentsystems and will be gradually transferred to the nationalsystem. China produces a huge amount of clinicaldocumentation every year50. According to a researchbased on a hospital in China, the hospital creates morethan 20,000 new inpatient records per year57. Suchrecords need to be shared between existing EHR/EMRsystems, and past data need to be transferred into thefuture system. Smart cards would be a cost-effectivemethod for sharing and transferring the records.An individual holds his or her EHR card, with whichthe individual can access to existing EHR or EMRsystems to download, append, edit or uploadEHR/EMRs. The card holder controls the operation onhis/her information.The features of using smart cards are:Appropriate incentive mechanism is essential forimplementing EHR and EMR systems. For adopting thePCEHR system, Australian government requires clinicsto participate, otherwise the clinics would becomeineligible for the eHealth PIP60, which is part of ablended payment approach. Similar as the PIP, China’sSocial Insurance Scheme (SIS) allows patients to paytheir own portion of fees at a hospital, and the hospitalwill be compensated for the remaining fees from theSIS. China can learn from Australia to enforce that SISsystem only links to the national EH/MR system.Chinese government allows hospitals to develophigher quality services, for which they can charge pricesabove the levels reimbursed by SIS. The charge forhigher quality services is one of the revenues thatproduce hospital gains61. Governments should requirethat higher quality services, including non-ensured drugsale and testing referral, are processed only by thenational EH/MR system.Australian government provides fund to supportclinics to develop their e-health capability60. It is morenecessary for Chinese governments to provide funds toPublished by Atlantis PressCopyright: the authors133
X. Gao et al.help CHSCs, county hospitals and township clinicsdevelop their EHR capability.4.4. Ensuring Sustainable FundAccording to software engineering research62 andinternational EHR experience35,63, system maintenancefor successful operation will cost much more than itsdevelopment. Sustainable fund is needed for adoptingEHRs and EMR
management; the '2' indicates two systems: electronic health record (EHR) system and electronic medical record (EMR) system; and the '1' represents one special network for healthcare3,4,5. Regarding the EHR and EMR, a health record is the information of health conditions about a healthcare recipient6 at CHSCs or