Transcription
Client selection, intake, andassessment in TelementalHealthSara Smucker Barnwell, PhDTuesday, May 26, 2020
Telehealth Learning Series: Tuesdays, 5-7 PMMay 12: Introduction to Telemental HealthMay 19: Preparing your office for Telemental HealthMay 26: Client selection, intake, and assessment in TelementalHealthJune 2: Clinical engagement in Telemental HealthJune 9: Emergencies, disruptions and pitfalls in Telemental HealthJune 16: Risk Management in Telemental HealthRegister @ NWATTC website
Sara Smucker Barnwell, PhDLicensed clinical psychologist in WAVA Telemental Health TeamYour presenterAPA Telepsychology GuidelinesCESATE fellowUnapologetic telehealth evangelist
Learning g yourpractice
Class structureDidactic lectureLive Q &A at section breaksVideo demonstrationsSubmitted questions nwattctelehealth@gmail.comLive Q & A
DisclaimersDuring a technology presentation, technology will failOffer best practice recommendations based on clinical work,literature review and regulatory experienceIdentifying personal best practices and guidance in developing area
DisclaimersAlways review state regulationsConsult with your own legal counselConsult with your risk management coverageI do not provide legal advice nor clinical advice
ConflictsProvides telehealth trainingKnown telehealth evangelist
Agenda: Preparing your officeClient selectionInclusion, exclusionIntakes, assessments, terminationSpecial populations (neuropsychology, forensic, youth)Building your TMH practiceAdvertising, staffThe role of physical space
The balanceBrief reviewDeep divesYour questions answeredOn demand prior classes
You look familiar Is this your first class?Please respond in chat window
Definitions and examples(Abbreviated!)
Operational definitionsTelemental Health (TMH):The provision of any mental health service usingtelecommunication technologies videoconferencingAccess is at the heart of this mission
HIPAAHealth Information Portability and Accountability Act (HIPAA):Federal law (Pub.L. 104-191, 100 Stat. 1936, enacted August 21, 1996)that aims to make it easier for people to keep health insurance, protectthe confidentiality and security of healthcare information and help thehealthcare industry control administrative costsHIPAA Privacy RuleHIPAA Security Rule
Protected Health Information(PHI)/ ePHI NamesFull-face photographic imagesGeographical subdivisionssmaller than stateAll dates (birth, death, discharge)Phone/ fax numbersElectronic mail addressesSocial Security numbersMedical record numbersHealth plan beneficiary numbersAccount Numbers Certificate/license numbersVehicle identifiers and serialnumbers, including license platenumbersDevice/ serial numbersWeb Universal Resource Locators(URLs)Internet Protocol (IP) addressBiometric identifiers, includingfinger and voice printsAny other unique ID numbers,code, or characteristic
Business Associates Agreement (BAA)Contract between HIPAA coveredentity and HIPAA BusinessAssociate (BA) that is used toprotect personal health information(PHI) in accordance with HIPAAguidelines.This Photo by Unknown Author is licensed under CC BY-SA
Novel Coronavirus/ COVID-19Current public health crisisSocial distancing and “stay home” ordersTelepractice as a tool to protect public healthSome providers now mandated to telehealth
Client selection
Client selection criteriaResearch suggests equivalence of in-person and many remotetreatments and high satisfactionObserve usual standards of care/ APA ethics codeTechnology is not a clinical specialty though it requirescompetence
Cultivating clientsAssess why remote service v. in-personThis assessment is evolvingLittle empirical/ few legal reasons to exclude specific clients;question of risk managementAssessing service appropriateness is ongoing
Your practiceWhat population do you serveWhat services do you offerWhat practice do you want
Client characteristicsClient vision and hearingPreference for modalityPractical adaptabilityThis Photo by Unknown Author is licensed under CC BY-NC
Client characteristicsHealth status/ status of loved onesJurisdictional requirements/ rulesCare access (e.g., distance, medical, financial)
Client clinical characteristicsDiagnosisAvoidance, Delusions regarding technology, othersTreatment historyStability
Client SUD historySUD considerations (UAs, reporting)Transportation concernsMedication assisted treatment for opioidsDHHS/ OCR announcements also applySpecial considerations for controlled substances
Client characteristicsClient care environment (e.g., office, home)Insurance/ reimbursementPrivacy/ stigma
ClienttechnicalcapabilitiesTechnical abilityTeachingAge, gender,education,experience goodexplanationThis Photo by Unknown Author is licensed under CC BY-NC
Client technical capabilitiesDoes the client possess technical resourcesComputer/ mobile device accessAdequate internet speedHardware/softwareMobile device, phone
Not the perfect client
Emergency probabilityClients receiving interactive remote care have emergency planConsider what you will do in case of medical or psychiatricemergency (e.g., local hospital, wellness check, others).
Emergency probabilityProblems that do not meet mandated reporting threshold butcause concernAvailability of support personWhere will patient discharge if no longer appropriate
Remember your clinical considerations
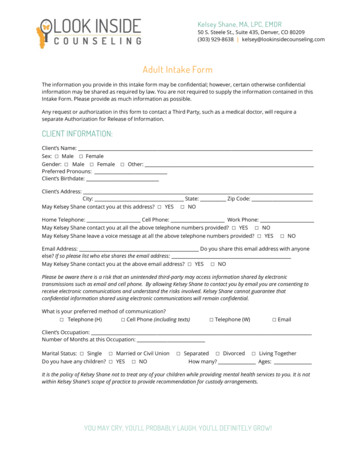
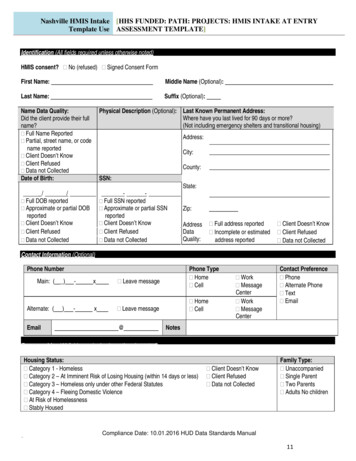
Telehealth Appropriateness AssessmentDelivering psychological services through remote technology provides the opportunityto reach clients who might not otherwise receive care. However, not every client will beappropriate for telehealth services. The questions below provide guidance regardingclinical and technical factors that you may wish to consider before committing to delivertelehealth care.Clinical Assessment1. What is the patient’s age?a. If a minor, how will you gather the parent’s consent?2. Is the client currently in crisis?3. In the past 12 weeks, have they had thoughts, intention or plans to hurtthemselves?a. About hurting someone else?4. Have they ever been hospitalized for emotional health reasons?a. When?b. What happened?5. Explain that telehealth services typically serve in non-crises. Explain manner inwhich telehealth providers support patients who later develop crises, but mayneed to supplement care with in-person meetings or transfer care.6. Is this issue related to an accident or legal action that is pending?a. Are they seeking an assessment related to legal action?7. Are they hoping to use insurance to pay for your visit?a. Who is their insurance carrier?b. Are you/ they familiar with your mental health benefits?c. With the insurance carrier’s policy regarding telehealth?d. Will you or the client contact insurance to discuss the telehealth policy?8. Why are they seeking telehealth care vs. in-person care?a. Is in-person care available in their community?9. Are they available to meet in person with the provider now or in the future?10. How do you plan to verify the client’s identity?11. In what state does the client intend to receive care?a. Does the client intend to travel often while receiving remote care?Technical Assessment1. Do they have access to a private space in their home?2. Is it relatively soundproof? How easily can conversation be overheard?a. Explain to the client the critical importance of keeping this space secureand confidential during appointments3. Do they have access to a computer or mobile device?a. What kind (e.g., desktop, laptop, tablet)?b. How old is it ( 7 years old)?Assessment
Take awayConvenience is neither a solely determining nor deterring factorNot every client is appropriateNo codified exclusion criteria
Take awayKnow your jurisdictional rules regarding COVID-19Decisions made using research and risk managementAs with in-person practice, you are not obligated to provideservice, but once begun you are obligated to refer for continuedcare
Vignette: Dr. EvilClient seeks services for alcohol use disorderActive use, comorbid Panic DisorderAvoidance of social circumstancesModerate suicidal ideation without active plan or intentHistory of self harm
ConsiderationsAccessibility of other treatment optionsClient health, willingness for in person care, referral availabilityRole of exposureClient willingness to pursue safe exposureYour comfort with remote emergency management
Live Q & A
Intakes, assessments,termination
Intakes
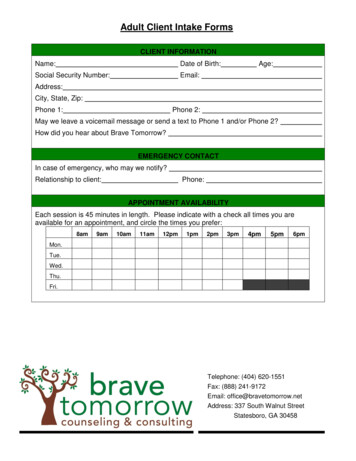
Intake preparationWho: inclusion/exclusion criteriaWhat: what servicesHow: which technologies (videoconferencing, telephone)When: schedule by phone, secure email, EMRRules: jurisdictional concerns, initial intakes
Intake preparationFee structureSelf-pay v. direct bill insurancePayment for session in which technology disruption occursSurchargesCollection of fee
Intake preparationYour space: austere background, adequate lighting, soundproofConsider use of headphonesHome office v. professional officePrivacyPHISmart speakers
Intake preparationIntake documentationTelehealth informed consent, emergency plan, questionnaires,payment, ROISimple documents; verbal consent
Intake preparationSecure document exchangeMail, fax, downloads from your websiteSecure email programs, secure FTP, EMR
Intake preparationCommunicate expectationsVideo call mechanics/ embed this in remindersBoundariesInterruptions, helpFor clients new to modality, 5 minute “test” check in
Initiating the intakeConfirm client can hear/see youConfirm location and setting securitySilence devices, windows, notifications
Initiating the intakeREVIEW RISKS ANDBENEFITSREVIEW EMERGENCY PLANANSWER ANY REMAININGNON-CLINICAL QUESTIONS
Conducting the intakeAdvance informationEngage with usualskillsAsk questions
Conducting the intakeConsider structured clinicalinterviewSCID VPace may differ
Assessment measuresCollect in advanceVerbally reviewScreen sharing
Behavioral observationsEye contact, facial expressionMay not offer same informationLooking away v. distractions inhome environmentBody posture and movements(gait, psychomotor agitation)
Behavioral observationsVOICE VOLUME/VOCALIZATIONSOLFACTORY DATALOSS AND GAIN
Intake conclusionEngagement/ how to meet their needsAdditional intake session is indicatedDiscuss future homework/ information transfer
Intake conclusionUsual concluding statementsIf appropriate, propose an engagement (a number of sessions,treatment plan)If accepted, schedule the next appointment/ invite client to scheduleonlineReview options or possible referral out/ where will referrals goAnswer patient's questions
Assessment
Remote assessmentNorm availabilityLicensing,permissionsConsultation
Remote assessmentObserved administrationImpacts of remoteassessment on self reportPotential secondary gainissues
Online psychometric assessmentMany more tests now onlineRemote MMPI administrationBatteries constructed for remote administrationObservations/ psychometricians
ConsiderIS REFERRING QUESTIONSTILL THE SAMECAN THE TEST BEADAPTEDARE NORMS AVAILABLE
ConsiderLICENSINGABBREVIATECAN IT WAIT
Special populations
ForensicsCOURT AVAILABILITYIN YOURJURISDICTIONWILL ADAPTATIONWITHSTANDEXAMINATIONSECONDARY GAINGOING INTO JAIL
YouthZoom fatigueRelevance of referring questions for IEPConsider abbreviated sessionsConsider increased parental involvement where appropriate
NeuropsychologicalPermissions, licensingNecessity of physical examFeedback sessionsWatch the marketplaceInterorganizational practice committee
Vignette: Dr. ImpossibleForensic assessment caseParental fitnessQuarantine configurationAcademic impacts
ConsiderationsCourts open/ closedStability of living situationWithstand attorney’s reviewCurrent school configurationIs delay appropriate
Termination
Termination and referralTermination occursfor diverse reasonsReferral resourcesKnow your telehealthcommunity
Termination and referralTermination due to modalityWhat is clinically advisableRole of avoidance v. preferenceYour recommendations
Vignette: Dr. VentureClient treated for comorbid benzodiazepine use and anxietydisorderDoes not like modalityFrustrated
ConsiderationsWillingness/ availability of referralMedical safetyLegal involvementYour clinical judgement
Live Q & A
Building your TMHpractice
Building a TMH practiceRole of physical spaceReferralsDocumentationTraining and consultation
tionshipsin communityyou wish toserveAdvertising
OutreachPrimary careSpecialty clinicsSUD, medication assisted opioid careCommunity organizationsConsider offering free psychoeducation to membership
Physical spaceOffice spaceEmergency management, assessmentJurisdictional requirementsThis Photo by Unknown Author is licensed under CC BY
Technology investmentProducts designed for healthcareVideoconferencing, telephoneDocument transfer (email, fax, secure message)EMR
Administrative staffIntegrating administrative staff into use of TMHCoordinate 1 treatment “room” for patientAdministrative login to EMR/ videoconferencing product
Administrative staffWhat do we wantthem to accomplishMeasure collectionConfirm privacy,visibilityReview risks/benefits
Coronavirusconsiderations
Transition from shortto long-termTelemental HealthLong-termTMHExisting clients, newclientsInvestment in long-term
Temporary v. a practiceyou will continue toofferLong-termTMHBalanceSelf care
In summary
Client selectionDetermine and document your inclusion/ exclusion criteriaDetermine what services you want to offer whoAssessment is ongoing
IntakesCollect information beforehandSlow the paceAsk question, structured interviewingFocus on rapport
Assessment, special populationsUse appropriate online assessment when possiblePractical considerationsAbbreviated batteriesSome assessments will be delayed
TerminationKnow your referralsContemplate avoidanceOffer your opinion
Building your practiceAdvertise, reach outInvest in sustainable technologyRole of physical spaceKnow your jurisdictionTrain staff
That’s a good questionPreviously submitted questions
Telepsychology templatesReturn to in person care informed ustinsurance.com/ResourceCenter/COVID-19-Resources
SAMSHA handout1-pagehandoutEMR (Simple Practice)may have templates
Live Q & A
Questions for future learning series sessionsPlease contact nwattctelehealth@gmail.com
Thank you!Sara Smucker Barnwellnwattctelehealth@gmail.com
Offer best practice recommendations based on clinical work, . Hardware/software Mobile device, phone. Not the perfect client. Emergency probability . Decisions made using research and risk management As with in-person practice, you are not obligated to provide service, but once begun you are obligated to refer for continued .