Transcription
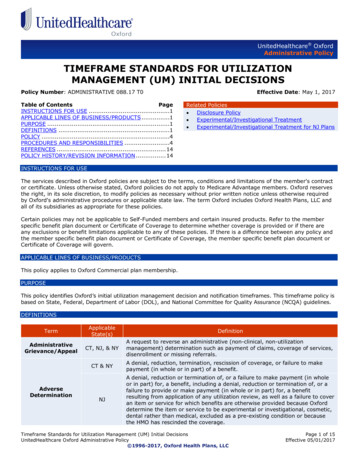
UnitedHealthcare OxfordAdministrative PolicyTIMEFRAME STANDARDS FOR UTILIZATIONMANAGEMENT (UM) INITIAL DECISIONSPolicy Number: ADMINISTRATIVE 088.17 T0Table of ContentsPageINSTRUCTIONS FOR USE .1APPLICABLE LINES OF BUSINESS/PRODUCTS .1PURPOSE .1DEFINITIONS .1POLICY .4PROCEDURES AND RESPONSIBILITIES .4REFERENCES . 14POLICY HISTORY/REVISION INFORMATION . 14Effective Date: May 1, 2017Related Policies Disclosure Policy Experimental/Investigational Treatment Experimental/Investigational Treatment for NJ PlansINSTRUCTIONS FOR USEThe services described in Oxford policies are subject to the terms, conditions and limitations of the member's contractor certificate. Unless otherwise stated, Oxford policies do not apply to Medicare Advantage members. Oxford reservesthe right, in its sole discretion, to modify policies as necessary without prior written notice unless otherwise requiredby Oxford's administrative procedures or applicable state law. The term Oxford includes Oxford Health Plans, LLC andall of its subsidiaries as appropriate for these policies.Certain policies may not be applicable to Self-Funded members and certain insured products. Refer to the memberspecific benefit plan document or Certificate of Coverage to determine whether coverage is provided or if there areany exclusions or benefit limitations applicable to any of these policies. If there is a difference between any policy andthe member specific benefit plan document or Certificate of Coverage, the member specific benefit plan document orCertificate of Coverage will govern.APPLICABLE LINES OF BUSINESS/PRODUCTSThis policy applies to Oxford Commercial plan membership.PURPOSEThis policy identifies Oxford’s initial utilization management decision and notification timeframes. This timeframe policy isbased on State, Federal, Department of Labor (DOL), and National Committee for Quality Assurance (NCQA) tionAdministrativeGrievance/AppealCT, NJ, & NYA request to reverse an administrative (non-clinical, non-utilizationmanagement) determination such as payment of claims, coverage of services,disenrollment or missing referrals.CT & NYAdverseDeterminationNJA denial, reduction, termination, rescission of coverage, or failure to makepayment (in whole or in part) of a benefit.A denial, reduction or termination of, or a failure to make payment (in wholeor in part) for, a benefit, including a denial, reduction or termination of, or afailure to provide or make payment (in whole or in part) for, a benefitresulting from application of any utilization review, as well as a failure to coveran item or service for which benefits are otherwise provided because Oxforddetermine the item or service to be experimental or investigational, cosmetic,dental rather than medical, excluded as a pre-existing condition or becausethe HMO has rescinded the coverage.Timeframe Standards for Utilization Management (UM) Initial DecisionsUnitedHealthcare Oxford Administrative Policy 1996-2017, Oxford Health Plans, LLCPage 1 of 15Effective 05/01/2017
Business DayApplicableState(s)CT, NJ, & NYA working day (not including weekends or holidays).Calendar DayCT, NJ, & NYBusiness and non-business days (including weekends and holidays).TermCT & NYClaimNJClaimantClinical PeerCT, NJ, & NYCTDefinitionAny request for service submitted by a Claimant for pre-service, concurrent,or post service benefits.A request by a member, a participating health care provider or anonparticipating health care provider who has received an assignment ofbenefits from the member, for payment relating to health care services orsupplies covered under a health benefits plan issued by Oxford.The covered member or the member's authorized designee.A physician or other health care professional who holds a non-restrictedlicense in a state of the United States and in the same or similar specialty astypically manages the medical condition, procedure or treatment underreview.Note: For all requests involving: A child or adolescent substance use disorder or a child or adolescent mentaldisorder the clinical peer must hold:o A national board certification in child and adolescent psychiatry; oro A doctoral level psychology degree with training and clinical experiencein the treatment of child and adolescent substance use disorder or childand adolescent mental disorder, as applicable. An adult substance use disorder or an adult mental disorder the clinicalpeer must hold:o A national board certification in psychiatry, or psychology, oro A doctoral level psychology degree with training and clinical experiencein the treatment of adult substance use disorders or adult mentaldisorders, as applicable.ConcurrentReviewCT, NJ, & NYA review conducted during the course of treatment and concomitant with atreatment plan. Included, but not limited to, concurrent review is theanticipation and planning for post hospital needs, arrangement for posthospital or acute treatment follow-up and support, ongoing review forchiropractic, mental health services and other ongoing therapies.EmergentCT, NJ, & NYSudden or unexpected onset of severe symptoms which indicate an illness orinjury for which treatment may not be delayed without risking the member'slife or seriously impairing the member's healthCT, NJ, & NYA modified review process for a Claim involving urgent or emergent care.Note: In addition, acute care inpatient admissions/stay in Connecticut, as perthe Connecticut Managed Care Act dated 11/1/97, can result in expeditedreview requests from providers for members admitted to an acute carehospital. The request is used when an attending physician determines that themember's life will be endangered or other serious injury could occur if themember is discharged and/ or treatment is delayed.NJAn adverse benefit determination that has been upheld by Oxford at thecompletion of the internal appeal process, an adverse benefit determinationwith respect to which Oxford has waived its right to an internal review of theappeal, an adverse benefit determination for which Oxford did not comply withthe requirements of N.J.A.C. 11:24-8.4 or 8.5, and an adverse benefitdetermination for which the member or provider has applied for expeditedexternal review at the same time as applying for an expedited internal appeal.CT & NYA request for services (Prospective) that requires approval by Oxford, in wholeor in part, before the service can be rendered; a service that must beapproved in advance before it is rendered.Expedited ReviewFinal Service)ClaimPrecertification,UrgentNJCT, NJ, & NYAny claim for a benefit with respect to which the terms of the plan conditionreceipt of the benefit, in whole or in part, on approval of the benefit inadvance of obtaining medical care.Requires immediate action, although it may not be a life-threateningcircumstance an urgent situation could seriously jeopardize the life or health ofTimeframe Standards for Utilization Management (UM) Initial DecisionsUnitedHealthcare Oxford Administrative Policy 1996-2017, Oxford Health Plans, LLCPage 2 of 15Effective 05/01/2017
t(continued)CT, NJ, & NYthe covered member or the ability of the member to regain maximum functionor in the opinion of a physician with knowledge of the claimant's condition wouldsubject the member to severe pain. An urgent care condition is a situation thathas the potential to become an emergency in the absence of treatment.Retrospective,(Post-Service)ClaimCT, NJ, & NYA claim for services, which have already been rendered. Occurs whennotification is after the fact of care/service/delivery. The need for "retroreview" is most often created by late or non-notification.TermUrgent BehavioralHealth ServicesCTCTUrgent CareRequestUtilization ReviewThose for a service or treatment for: Substance use disorder or co-occurring mental disorder; and Inpatient services, partial hospitalization, residential treatment or thoseintensive outpatient services needed to keep a covered person fromrequiring an inpatient setting in connection with a mental disorder. A request for a health care service or course of treatment for:o Which the time period for making a non-urgent care requestdetermination: Could seriously jeopardize the life or health of the covered personor the ability of the covered person to regain maximum function,or In the opinion of a health care professional with knowledge of thecovered person's medical condition, would subject the coveredperson to severe pain that cannot be adequately managed withoutthe health care service or treatment being requested. Whendetermining whether a benefit request shall be considered anurgent care request, an individual acting on behalf of a healthcarrier shall apply the judgment of a prudent layperson whopossesses an average knowledge of health and medicine, exceptthat any benefit request determined to be an urgent care requestby a health care professional with knowledge of the coveredperson's medical condition shall be deemed an urgent carerequest.o A substance use disorder* or for a co-occurring mental disorder, ormental disorder.o Inpatient services, partial hospitalization, residential treatment orintensive outpatient services necessary to keep a covered person fromrequiring an inpatient setting in connection with a mental disorder.*Persons with substance use disorders, as defined by the state of Connecticutare alcohol dependent or drug dependent persons.NJAny claim for medical care or treatment with respect to which application ofthe time periods for making non-urgent determinations, in the judgment of aprudent layperson who possesses an average knowledge of health andmedicine, could seriously jeopardize the life or health of the covered person orthe ability of the covered person to regain maximum function or that, in theopinion of a physician with knowledge of the claimant’s medical condition,would subject the covered person to severe pain that cannot be adequatelymanaged without the care or treatment that is the subject of the claim.NYA request for a health care service or course of treatment for which the timeperiod for making a non-urgent care request determination could seriouslyjeopardize the life or health of the covered person or the ability of the coveredperson to regain maximum function, or, in the opinion of a health careprofessional with knowledge of the covered person's medical condition, wouldsubject the covered person to severe pain that cannot be adequately managedwithout the health care service or treatment being requested.NYThe review to determine whether health care services that have beenprovided, are being provided or are proposed to be provided to a patient,whether undertaken prior to, concurrent with or subsequent to the delivery ofsuch services are medically necessary.Exceptions (not considered a utilization review): Denials based on failure to obtain health care services from a designatedor approved health care provider as required under a contract;Timeframe Standards for Utilization Management (UM) Initial DecisionsUnitedHealthcare Oxford Administrative Policy 1996-2017, Oxford Health Plans, LLCPage 3 of 15Effective 05/01/2017
TermApplicableState(s)Definition Utilization Review(continued)NY Where any determination is rendered pursuant to subdivision three-a ofsection twenty-eight hundred seven-c of the public health law;The review of the appropriateness of the application of a particular codingto a patient, including the assignment of diagnosis and procedure;Any issues relating to the determination of the amount or extent ofpayment other than determinations to deny payment based on an adversedetermination; andAny determination of any coverage issues other than whether health careservices are or were medically necessary.POLICYOxford follows all State, Federal and NCQA guidelines regarding timeframes for Utilization Management initialdeterminations. This includes Behavioral Health and Pharmacy initial determinations, and excludes issues of fraud orabuse. Although Oxford's goal is to adhere to the strictest timeframe applicable to all of its lines of business (see theTimeframe Standards Comparison grid below), Oxford will meet the mandated timeframes applicable to the particularrequest. Failure to adhere to applicable state, federal or regulatory resolution timeframes for any state in whichOxford or its delegate is licensed to perform Utilization Management, may result in a technical reversal of the initialdetermination.PROCEDURES AND RESPONSIBILITIESInitial Determination Timeframes for Utilization Management Issues The timeframe for utilization management decisions, and notification of decisions, is calculated from the date ofthe request for services, or the date on which we receive all necessary information, whichever is shorter. The Department of Labor (DOL) regulations will supersede all state timeframes unless the state timeframe is morerestrictive than the DOL regulations and does not prohibit application of the DOL regulations. This comparison isrepresented in the Timeframe Standards Comparison grid below. Initial determinations timeframes for utilization management issues includes Medically Necessary determinationsas well as determinations involving treatment or services that are considered Experimental or Investigational(refer to policies titled Experimental/Investigational Treatment and Experimental/Investigational Treatment for NJPlans). When additional information is necessary in order to make an initial determination, Oxford will notify the Memberor the Member’s designee of what specific information is needed.Note: Oxford administers benefit coverage for behavioral health services in coordination with OptumHealth BehavioralSolutions. OptumHealth Behavioral Solutions has developed level of care (LOC) guidelines which are used for purposesof clinical guidance, utilization management and medical necessity determinations, where applicable. The LOCguidelines ensure that services are essential and appropriate, and reflect empirically validated approaches.For additional information on Level of Care Guidelines and other topics, please refer to providerexpress.com and; Introduction to the OH/OHBSCA Level of Care Guidelines Common Criteria and Best Practices for All Levels of CareCT Products OnlyUtilization Management ReviewsWhen conducting utilization management reviews, Oxford or its designated utilization review agent must: Collect only information necessary, including pertinent clinical data, to make the utilization review or benefitdetermination. Ensure the review is conducted in a manner that ensures the independence and impartiality of the individual orindividuals involved in making the utilization review determination.Note: All adverse utilization review determinations must be evaluated by an appropriate clinical peer (Refer tothe Definitions section) not involved in the initial or previous adverse determination. Make no decisions regarding the hiring, compensation, termination, promotion or other similar matters of suchindividual or individuals based on the likelihood that such individual or individuals will supports the denial ofbenefits.Rescission of AuthorizationsPrior authorizations for admissions, services, procedures, or extensions of hospital stays may not be reversed orrescinded if:Timeframe Standards for Utilization Management (UM) Initial DecisionsUnitedHealthcare Oxford Administrative Policy 1996-2017, Oxford Health Plans, LLCPage 4 of 15Effective 05/01/2017
Oxford failed to notify the insured or member’s health care provider at least three business days before thescheduled date of the admission, service, procedure, or extension of stay that it was reversed or rescinded due tomedical necessity, fraud, or lack of coverage; andThe admission, service, procedure, or extension of stay took place in reliance on the prior authorization.Timeframe Standards ComparisonGo to the appropriate table to compare timeframe standards for CT, NJ, NY, RI, and DOL. Pre-Service Requests Post-Service (Retrospective Review) Requests Con-Current (On-Going Course of Treatment) Requests Urgent Requests Urgent Con-Current (On-Going Course of Treatment) RequestsInitial DecisionTimeframePre-Service RequestsStateNotificationStrictest Timeframe/Oxford GoalAdditional Information CTWithin 15 days afterreceiving the request.Exception: For certainurgent behavioral healthservices (Definitions), 24hours after receiving therequest (both initial andappeal determinations)*.*This timeframe will alsoapply to expeditedexternal urgent reviewsfor the behavioral healthservices (Definitions).Verbal notification will begiven to the requester,written notification willbe sent to the memberor the member’sdesignee and theprovider.If additional informationis required to make adetermination of medicalnecessity the claimantwill have 45 days toprovide the information. NJNYDeterminations arerendered on a timelybasis, as required by theexigencies of thesituation, but in no eventlater than 72 hours forurgent care claims andno later than 15 calendardays from receipt ofnecessary information.Written notification ofdenials or limitations willbe given to the hospitalor Provider.Three (3) business daysfrom receipt of necessaryinformation.Verbal notification will begiven to the requester,written notification willbe sent to the memberor the member’sdesignee and theprovider. To the extentpracticable, such writtennotification to themember's health careIf additional informationis required to make adetermination of medicalnecessity the claimantwill have 45 days toprovide the information. If additional informationis required to make adetermination of medicalnecessity the claimantwill have 45 days toprovide the information.Timeframe Standards for Utilization Management (UM) Initial DecisionsUnitedHealthcare Oxford Administrative Policy 1996-2017, Oxford Health Plans, LLC Initial determinationswill be made in 2business days fromreceipt of necessaryinformation, not toexceed 15 calendardays from receipt ofthe request.Oxford will notifywithin 2 businessdays that there is alack of information tomake thedetermination. Theclaimant will have 45days to provide theadditionalinformation.Initial determinationswill be made in 2business days fromreceipt of necessaryinformation, not toexceed 15 calendardays from receipt ofthe request.Oxford will notifywithin 2 businessdays that there is alack of information tomake thedetermination. Theclaimant will have 45days to provide theadditionalinformation.Initial determinationswill be made in 2business days fromreceipt of necessaryinformation, not toexceed 15 calendardays from receipt ofthe request.Oxford will notifywithin 2 businessPage 5 of 15Effective 05/01/2017
Initial DecisionTimeframePre-Service RequestsStateNotificationStrictest Timeframe/Oxford GoalAdditional Informationprovider shall betransmittedelectronically, in amanner and form agreedupon by the parties.Note: Effective forgroups new or renewingon or after 04/01/2016determinations for anyrequest for court orderedmental health and orsubstance use disorderservices must be madeby telephone within 72hours of receipt of therequest. Written noticeof the determination tothe member or member'sdesignee shall followwithin 3 business days.NYdays that there is alack of information tomake thedetermination. Theclaimant will have 45days to provide theadditionalinformation. DOLFifteen (15) calendardays from receipt of therequest. Up to 15-dayextension if requestedwithin the initialtimeframe for review.To member or member’sdesignee; written noticefor adversedeterminations.If additional informationis required to make adetermination of medicalnecessity the claimantwill have 45 days toprovide the information. RIDefault to DOL.Written notification willbe given to the memberor the member'sdesignee and to theprovider.Initial DecisionTimeframePost-Service (Retrospective Review)StateCTWithin 30 calendar daysafter receiving therequest.For RI residents andproviders, the claimantwill have 15 days toprovide the additionalinformation.NotificationAdditional InformationTo member or member’sdesignee; written notice(DOL).If additional informationis required to make adetermination of medicalTimeframe Standards for Utilization Management (UM) Initial DecisionsUnitedHealthcare Oxford Administrative Policy 1996-2017, Oxford Health Plans, LLC Initial determinationswill be made in 2business days fromreceipt of necessaryinformation, not toexceed 15 calendardays from receipt ofthe request.Oxford will notifywithin 2 businessdays that there is alack of information tomake thedetermination. Theclaimant will have 45days to provide theadditionalinformation.RI residents andproviders, theclaimant will have 15days to provide theadditionalinformation.A decision will bemade within 2business days ofreceipt of theinformation, or 2business days fromthe expiration of thetime to provide it.Strictest Timeframe/Oxford Goal Initial Determinationwill be made 30 daysfrom receipt of thePage 6 of 15Effective 05/01/2017
Initial DecisionTimeframePost-Service (Retrospective Review)StateNotificationnecessity the claimantwill have 45 days toprovide the information.Determinations arerendered on a timelybasis, as required by theexigencies of thesituation.To member or member’sdesignee; written notice(DOL).NYThirty (30) business daysof receipt of necessaryinformation.Written notification willbe sent to the memberor the member’sdesignee and theprovider. To the extentpracticable, such writtennotification to themember's health careprovider shall betransmittedelectronically, in amanner and form agreedupon by the parties.If additional informationis required to make adetermination of medicalnecessity the claimantwill have 45 days toprovide the information.DOLThirty (30) days fromreceipt of the request.Up to 15-day extension ifrequested within theinitial timeframe forreview.To member or member’sdesignee; written notice.If additional informationis required to make adetermination of medicalnecessity the claimantwill have 45 days toprovide the information.NJStrictest Timeframe/Oxford GoalAdditional Information RIThirty (30) days fromreceipt of the request.Up to 15-day extension ifrequested within theinitial timeframe forreview.To member or member’sdesignee; written notice.For RI residents andproviders, the claimantwill have 15 days toprovide the additionalinformation. Initial DecisionNotificationTimeframeCon-Current (On-Going Course of Treatment)StateCTFifteen (15) calendardays from receipt of therequest.Exception: For certainurgent behavioral healthservices (Definitions), 24hours after receiving therequest (both initial andappeal determinations).**This timeframe will alsoapply to expeditedexternal urgent reviewsfor the behavioral healthservices (Definitions).If additional informationis required to make adetermination of medicalnecessity the claimantwill have 45 days toprovide the information.Timeframe Standards for Utilization Management (UM) Initial DecisionsUnitedHealthcare Oxford Administrative Policy 1996-2017, Oxford Health Plans, LLCRI residents andproviders, theclaimant will have 15days to provide theadditionalinformation.A decision will bemade within 15 daysof receipt of theinformation orexpiration of thetime to provide it.Notification tomember, member’sdesignee andprovider in writing.Strictest Timeframe/Oxford GoalAdditional Information Verbal notification will begiven to the requester,written notification willbe sent to the memberor the member’sdesignee and theprovider.request.Oxford will notifywithin 30 days thatthere is a lack ofinformation and theclaimant will have 45days to provide theinformation. Initial Determinationwill be made within24 hours of receipt ofnecessaryinformation.If additionalinformation isrequired to make adetermination ofmedical necessity theclaimant will have 45days to provide theinformation.Page 7 of 15Effective 05/01/2017
Initial DecisionNotificationTimeframeCon-Current (On-Going Course of Treatment)StateNJNYDeterminations arerendered on a timelybasis, as required by theexigencies of thesituation, but in no eventlater than 24 hoursfollowing receipt ofnecessary information forinpatient hospitalservices or care renderedin the emergencydepartment of a hospitalor 15 calendar days forother sites of service.Written notification ofdenials or limitations willbe given to the hospitalor Provider.One (1) business day ofreceipt of necessaryinformation.Verbal notification will begiven to the requester,written notification willbe sent to the memberor the member’sdesignee and theprovider. To the extentpracticable, such writtennotification to themember's health careprovider shall betransmittedelectronically, in amanner and form agreedupon by the parties.Note: Effective forgroups new or renewingon or after 04/01/2016determinations for anyrequest for court orderedmental health and orsubstance use disorderservices must be madeby telephone within 72hours of receipt of therequest. Written noticeof the determination tothe member or member'sdesignee shall followwithin 3 business days.Strictest Timeframe/Oxford GoalAdditional Information If additional informationis required to make adetermination of medicalnecessity the claimantwill have 45 days toprovide the information. If additional informationis required to make adetermination of medicalnecessity the claimantwill have 45 days toprovide the information. DOLRIFifteen (15) calendardays from receipt of preservice requests, or 72hours from receipt ofrequest for urgent carerequests.To member or member’sdesignee; written notice.Written notification willbe given to the memberwithin one business dayof the adversedetermination and to theprovider prior to the endof the certified period.If additional informationis required to make adetermination of medicalnecessity the claimantwill have 45 days toprovide the information.Timeframe Standards for Utilization Management (UM) Initial DecisionsUnitedHealthcare Oxford Administrative Policy 1996-2017, Oxford Health Plans, LLC Initial Determinationwill be made within24 hours of receipt ofnecessaryinformation.If additionalinformation isrequired to make adetermination ofmedical necessity theclaimant will have 45days to provide theinformation.Initial Determinationwill be made within24 hours of receipt ofnecessaryinformation.If additionalinformation isrequired to make adetermination ofmedical necessity theclaimant will have 45days to provide theinformation.Initial Determinationwill be made within24 hours of receipt ofnecessaryinformation.If additionalinformation isrequired to make adetermination ofmedical necessity theclaimant will have 45days to provide theinformation.Page 8 of 15Effective 05/01/2017
Initial DecisionTimeframeUrgent RequestsStateCT72 hours after receivingrequest. Necessaryadditional information tobe requested within 24hours of receipt of therequest. The Claimantwill have 48 hours toprovide the necessaryinformation. A decisionwill be rendered within48 hours after the earlierof the date the personprovides the necessaryinformation, or the dateby which the informationwas to have beensubmitted.Exception: For certainurgent behavioral healthservices (Definitions), 24hours after receiving therequest (both initial andappeal determinations)*.NotificationStrictest Timeframe/Oxford GoalAdditional Information Verbal notification will begiven to the requester,written notification willbe sent to the memberor the member’sdesignee and theprovider (DOL).Additional informationwill be requested within24 hours. The claimantwill have 48 hours toprovide the information.A decision will berendered within 48 hoursof receipt of theinformation or expirationof the original request. Not later than 24hours after receipt ofthe request.Additionalinformation will berequested within 24hours. The claimantwill have 48 hours toprovide theinformation. Adecision will berendered within 24hours of receipt ofthe information orexpiration of theoriginal request.*This timeframe will alsoapply to expeditedexternal urgent reviewsfor the behavioral healthservices (Definitions).NJNY Determinations arerendered on a timelybasis, as required by theexigencies of thesituation, but in no eventlater than 24 hoursfollowing receipt ofnecessary information forinpatient hospitalservices or care renderedin the emergencydepartment of a hospitalor 15 calendar days forother sites of service.Written notification ofdenials or limitations willbe given to the hospitalor provider.3 business days ofreceipt of necessaryinformation.Verbal notification will begiven to the requester,written notification willbe sent to the memberor the member’sdesignee and theprovider. Writtennotification to themember's health careprovider shall betransmittedelectronically, to theextent practicable, in aAdditional informationwill be requested within24 hours. The claimantwill have 48 hours toprovide the information.A decision will berendered within 48 hoursof receipt of theinformation or expirationof the original request. Additional informationwill be requested within24 hours. The claimantwill have 48 hours toprovide the information.A decision will berendered within 48 hoursof receipt of theinformation or expirationof the original request.Timeframe Standards for Utilization Management (UM) Initial DecisionsUnitedHealthcare Oxford Administrative Policy 1996-2017, Oxford Health Plans, LLC Not later than 24hours after receipt ofthe request.Additionalinformation will berequested within 24hours. The claimantwill have 48 hours toprovide theinformation. Adeci
Expedited Review review requests from providers for members admitted to an acute care CT, NJ, & NY A modified review process for a Claim involving urgent or emergent care. Note: In addition, acute care inpatient admissions/stay in Connecticut, as per the Connecticut Managed Care Act dated 11/1/97, can result in expedited hospital.











