Transcription
Billing and Coding UpdateAlexander Miller, M.D.AAD Representative to the AMA CPTAdvisory Committee
New Skin Biopsy CPT CodesIt’s all about the Technique!
SPEAKER:Alexander Miller, M.D.AAD Representative to the AMA-CPT Advisory CommitteeChairAAD Health Care Finance Committee
Arriving on January 1, 2019New and Restructured Biopsy CodesTangential biopsyPunch BiopsyIncisional Biopsy
How Did We Get Here?CMS CY 2016Biopsy codes (11100, 11101 identified as potentially mis-valued; high expenditureRUC Survey sent to AAD MembersSpecialty survey results are the only tool available to support code valuesChallenging survey resultsSurvey revealed bimodal data distribution;respondents were valuing different proceduresCPT Codes 11100, 11101 referred to CPT forrestructuring
Rationale for New Codes11100; 11101 Previous skin biopsy codes did not distinguish between thedifferent biopsy techniques that were being usedCPT Recommended technique specification in newbiopsy codes Will also provide for reimbursement commensurate with thetechnique used
How Did We Get Here?February 2017March 2017April 2017 CPT Editorial Panel deleted 11100; 11101 6 New codes created based on technique utilized Each technique: primary code and add-on code RUC survey sent to AAD members Survey results presented to the RUC
Biopsy Codes Effective Jan., 1, 2019 Integumentary biopsy codes11100, 11101 have been deleted New Skin Biopsy codes: 11102 skin1110711755301004049040808only, does not includemucosa4110041105 Site-specific biopsy codes still41108applicable541005660556606All remain unchanged6781069100Biopsy of nail unit (plate, bed, matrix, hyponychium,proximal and lateral nail foldsBiopsy, intranasalBiopsy of lip mucosaBiopsy, vestibule of mouthBiopsy of tongue; anterior two-thirdsBiopsy of tongue; posterior one-thirdBiopsy of floor of mouthBiopsy of penisBiopsy of vulva or perineum; 1 lesionBiopsy of vulva or perineum, each separate additionallesionIncisional biopsy of eyelid skin including lid marginBiopsy external ear
Definition: Procedure to obtain tissue solely for histopathologicexamination Sampling of a lesionYou want to know what it is on histopathology, so you biopsy it Stratum corneum sampling by any method (scraping, tapestripping) is not a biopsy
Skin Biopsy codes can be reported to indicate:that the procedure wasperformed independently, orthat the procedure to obtainwas unrelated or distincttissue was solely forfrom otherdiagnostic ided during the sameencounterDuring excisions,destructions, orshave removals,tissue submittedfor histopathologyis a routinecomponent of suchprocedure(s) and isnot reportedseparatelybiopsies performed on a different lesion or different site(s) on the same date of service maybe reported separately as they are not considered components of other procedures
Code Criterion is Based on TechniqueBiopsytechniqueis selectedbased on:Optimal tissuesampling: considertype of neoplastic,inflammatory or otherlesion requiring tissuediagnosisThree distincttechniques:three primarybiopsy codes;three add-oncodes
2019 Skin Biopsy Codes11102Tangential biopsyof skin, (eg, shave,scoop, saucerize,curette), singlelesion11103each separate/additional lesion11104Punch biopsy ofskin, (includingsimple closurewhen performed),single lesion11105each separate/additional lesion11106Incisionalbiopsy of skin(eg, wedge),(including simpleclosure whenperformed),single lesion11107each separate/additional lesion
Tangential biopsy Vs. Shave removalShave removalTangential biopsyTangentialbiopsy Intent: obtain tissue sample fordiagnostic pathologic examinationInstrument: sharp blade, such as scalpel,flexible blade, curetteDepth: may include epidermis only, orepidermis and dermisHistopathologic tissue evaluation: alwaysdoneTwo codes only: primary and add-on Intent: therapeutic removal ofepidermal or epidermal-dermal lesion Instrument: removal with a sharpblade, such as scalpel, flexible blade Depth: not through dermis No suturing required Histopathologic tissue evaluation: maybe done Code selection: determined by site andlesion size
Tangential biopsy vs. Shave removal, examplesShave removalTangential biopsy Biopsy of an inflammatorydermatosis with the shavetechniqueBiopsy of a large atypicalpigmented lesion (saucerization orscoop biopsy technique, into deepdermis)Intent: obtain an optimal tissuesample for histopathology Cosmetic shave removal of anelevated nevus Shave removal of irritatedseborrheic keratosis, irritatednevus Intent: to completely remove thelesion; or to completely removethe noxious portion of lesion
Punch Biopsy (11104, 11105)Intent:obtain tissue sample fordiagnostic pathologicexamination usingpunch instrumentFull-thickness removal ofa skin sample, includingsimple closurePunch penetratesthrough dermis intosubdermal spaceHistopathologic tissueevaluation always doneManipulation of theadjoining skin, such asremoval of adjacentstanding cones/Burow’striangles/dog ears isincludedTwo codes only:primary and add-on1110411105
Punch Biopsy ExamplePunch defect:through dermisExcision ofstanding conesincludedSimplesuturingincluded
Incisional Biopsy Vs. ExcisionIncisional Biopsy Intent: obtain tissue sample for diagnostichistopathologic examination Instrument: sharp blade (not a punch) Depth: full-thickness tissue sample:o penetrates into the subcutaneous spaceo May include large fat tissue sample, ifrequired (eg, panniculitis) Includes: simple closure Histopathologic evaluation: always done Two codes only: primary and add-onExcision, benign or malignant Intent: excision of entire lesion, with marginsInstrument: sharp bladeDepth: full-thickness, through dermisIncludes: simple closureHistopathologic evaluation: usually doneCode selection determined by:– Benign vs. Malignant– Location– Maximum excision diameter
Incisional Biopsy Vs. Soft Tissue BiopsyIncisional Biopsy Intent: obtain tissue sample for diagnostichistopathologic examination Instrument: sharp blade (not a punch) Tissue sample: full-thickness skino penetrates into the subcutaneous spaceo Contains skino May include large fat tissue sample, ifrequired Includes: simple closure Histopathologic evaluation: always done Two codes only: primary and add-onBiopsy, Soft Tissue Intent: sampling of tissues deep to skin:subcutaneous, subfascial, intramuscular Instrument: sharp blade Tissue sample: subcutaneous or subfascial ormuscleo Skin may not be included Includes: simple or intermediate repair Histopathologic evaluation: always done Code selection determined by:oLocationoType of biopsy: superficial or deep
2018 vs. 2019 Biopsy Coding20192018 First biopsy: First biopsy:11100 each additional:1110111106: Incisional11104: Punch11102: Tangential each additional:11107: Incisional11105: Punch11103: Tangential
Biopsy Coding HierarchiesIncisionalbiopsy 11106Punch ch:11105AdditionalPunch: l:11103TangentialBiopsy 11102Additionaltangential:11103
Single Technique Biopsy Coding ExamplesTangentialPunchThree tangential Bx:11102, 11103x2Three punch Bx:11104, 11105x2IncisionalTwo incisional Bx:11106, 11107
Multiple Biopsies, Different Lesions or SitesMore than one biopsywith differenttechniques used foreach additional lesionList the highest valuebase (primary) codefirstAdditional biopsy addon codes in order ofhighest to lowest value
11102 11103311104 11105211106 111071
Multiple Biopsies of Different Lesions or Sites Only one primary code is used, regardless if multiple biopsytechniques used When multiple biopsies are done, use one primary code and addon code(s) appropriate to the additional biopsy techniques used Incisional biopsy (11106) is always primary to other biopsytechniques Punch biopsy (11104) is always primary when shave biopsy alsoperformed
Multiple Techniques Biopsy Coding ExamplesOne incisional,one punch, twotangential 11106(incisional) 11105 (punch) 11103x2(tangential)Two punch, onetangential 11104 (punch) 11105 (punch) 11103(tangential)One incisional,two tangential 11106(incisional) 11103(tangential) 11103(tangential)
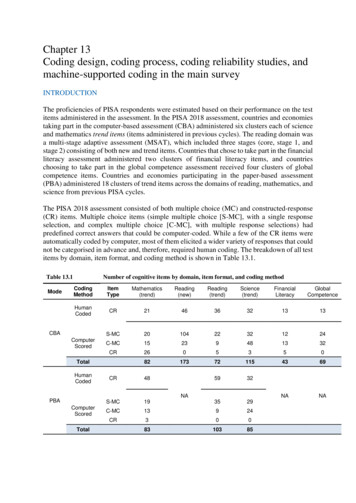
CodeCMS 2019 Proposed RVUsDescriptorRVU11102Tangential.6611103Tangential Add-On.29 (RUC recommended .38)11104Punch.8311105Punch Add-On.4511106Incisional1.0111107Incisional Add-On.5411100Deleted Biopsy.8111101Deleted Biopsy Add-On.41
CMS Proposed Values for Skin Biopsy Codes - 20192019CPT /DescriptionHCPCS11100Biopsy of ilityRVUs3.00Medicare MedicareNational NationalAverage2019 Total Average2018Non2019Payment PaymentFacilityAmount Amount RVUsNA 108.00NA11101Biopsy of skin add-on0.41n/a0.93NA 33.48NA11102Tangential bx skin single lesionNA0.66NA2.68NA 96.6011103Tangential bx skin ea sep/addlNA0.29NA0.64NA 23.0711104Punch bx skin single lesionNA0.83NA3.37NA 121.4811105Punch bx skin ea sep/addlNA0.45NA1.09NA 39.2911106Incisional bx skin single lesionNA1.01NA4.06NA 146.3511107Incisional bx skin ea sep/addlNA0.54NA1.25NA 45.06
National Correct Coding Edits Medically Unlikely Edits (MUEs) for the new biopsy codeshave been determined Multiple procedures on the same date of service are still likelyto be reduced under the multiple surgical reduction rule(MSRR) Add-on codes need not be further discounted However, payers can choose to discount payment for any reason in spiteof CMS/NCCI guidelines
2019 NCCI Edits ExamplesColumn1/Column 2 EditsColumn 1Column 2114421144211442116021160211602170001700017000 11102 11104 11106 11102 11104 11106 11102 11104 11106Modifier0 Not Allowed1 Allowed9 Not Applicable111111111Column 1Column 2170041700417004171101711017110172621726217262 11102 11104 11106 11102 11104 11106 11102 11104 11106Modifier0 Not Allowed1 Allowed9 Not Applicable111111111
2019 MUE Edits/MAI IndicatorsPractitionerHCPCS/CPT Code Services MUEValuesMUE AdjudicationIndicator (MAI)MUE Rationale 1110212 Date of Service EditDate of Service Edit 1110363 Date of Service EditDate of Service Edit 1110412 Date of Service EditDate of Service Edit 1110533 Date of Service EditDate of Service Edit 1110612 Date of Service EditDate of Service Edit 1110723 Date of Service EditDate of Service EditMAI 2 Based on policy; not appealableMAI 3 Based on “clinical benchmarks:”; appealable
MAI123Impact onClaimCLAIM LINEEDITDATE OFSERVICEEDIT:POLICYDATE OFSERVICEEDIT:CLINICALEdit Rationale These are “claim line edits”Based on CPT code descriptor and is not appealable These are “per day edits based on policy”Rigorously reviewed and vetted within CMSMAI designation because UOS on the same date of service (DOS) in excess of the MUE value would beconsidered impossible because it was contrary to statute, regulation or subregulatory guidance. This subregulatory guidance includes clear correct coding policy that is binding on both providers and CMSclaims processing contractors.Limitations created by anatomical or coding limitations are incorporated in correct coding policy, both in theHIPAA mandated coding descriptors and CMS approved coding guidance as well as specific guidance inCMS and NCCI manuals.) These are “per day edits based on clinical benchmarks”. If claim denials based on these edits are appealed, contractors may pay UOS in excess of the MUE value ifthere is adequate documentation of medical necessity of correctly reported units. If contractors have pre-payment evidence (e.g. medical review) that UOS in excess of the MUE value wereactually provided, were correctly coded and were medically necessary, the contractor may bypass the MUEfor a HCPCS/CPT code with an MAI of “3” during claim processing, reopening or redetermination, or inresponse to effectuation instructions from a reconsideration or higher level appeal.)
Questions/More InformationFaith McNicholasfmcnicholas@aad.orgPeggy Eiden peiden@aad.orgCynthia Stewart cstewart@aad.org
Is this a: Simple repair Intermediate repair Complex repairSimple repair ” requires simple one layerclosure.” (CPT 2018)
Intermediate Repair Layered closure Underminingnot required
Complex RepairExcision of standing cones (Burow triangles, dog ears) does not justify a complexrepair code.Complex repair Layered closure plus “extensive” undermining,retention sutures, scar“Note: Dogrevision, debridement (forears/Burow'straumatic lacerations,triangles may beavulsions)included as a part of Nothing is said in CPT aboutthe complex repair.”standing cone removalCPT Assistant Excision of standing conesAugust 2006, pg 1Standing coneslengthens the line of closure(Burow triangles) Complex repair codes arestratified via location and length
Complex Repairs: CPT 13100-13153Excision of redundant skin triangles to generate a fusiform shapefor repair does not make it a complex repairWhy doesn’t theCPTdefine extensiveundermining?
CPT : “Sum of lengths of repairs for each group of anatomic sites.”Repair, complex, scalp, arms, and/or legs;
Complex Repairs: CPT 13100-13153Retention Sutures are used to reinforce asingle layer closure of atrophic, fragile skinthat is unable to support buried dermalsutures.
Modifier 25: Undergoing Insurer Scrutiny andattempts at payment reductionsCPT : Significant, separately identifiable evaluation and management service by the samephysician or other qualified health care professional on the same day of the procedure or otherservice Patient’s condition required a significant, separately identifiable E/M Service is above and beyond usual preoperative and postoperative careincluded in a procedure Substantiated by documentation that satisfies the relevant criteria for therespective E/M service to be reported E/M service may be prompted by the symptom or condition for which theprocedure was provided Separate diagnoses are not required Service needs to be reasonable and necessary40
What is Included in a proceduralCPT code? Evaluation of a specific lesion for which aprocedure is done Decision to perform a minor surgical procedure (0and 10 day global) Certain elements of history pertaining to thelesion for which a procedure is done Usual, uncomplicated preoperative evaluation Usual, uncomplicated postoperative care41
An established patient comes in with a complaint of an asymptomatic, growingplaque on his nose. You generate a differential diagnosis of BCC, adnexal tumoror granulomatous disease. You proceed to biopsy the lesion.You submit the following billing:A) Biopsy, 11100 and E/M, 99213B) Biopsy 11100C) Biopsy 11100 and E/M 99213.25D) Biopsy 11100 and E/M 99212.25E) Biopsy 11100.59 and E/M 9921342
What is included in biopsy valuation?CPT 11100 (biopsy)Pre-service: one obtains a pertinent history includingprevious skin cancer, prior treatments, and sun protection.Indications for the biopsy, expected benefits, and adescription of the procedure and its risks are discussed.Consent is obtained and the biopsy tray is prepared.Intra-service: selection of the optimal biopsy site andlesion inspection and palpation, and then the biopsyprocedure itself from start to bandaging.Post-service: patient instruction on care and follow-up,charting, and communication with any referring physician.
An established patient comes in with a complaint of an asymptomatic, growingplaque on his nose. You generate a differential diagnosis of BCC, adnexal tumoror granulomatous disease. You proceed to biopsy the lesion.You submit the following billing:Biopsy 11100Why only 11100?The evaluation focused only upon the biopsied lesion. No other work beyond thatincluded in the 11100 biopsy valuation was done.44
What is included in procedure valuation?CPT 17260 -17286 (malignant lesion destructions)Pre-service: review of pertinent medical records data, followed bydiscussion of the treatment options and risks. Obtain informedconsent and have the necessary procedure tray prepared.Intra-service: the lesion is inspected, palpated, and its size,location, functional risks, and depth are recorded. Anesthetic isadministered and the procedure is done.Post-service: antibiotic ointment and any dressing are applied andpertinent instructions are given. Recurrence risks and the need forfollow-up are discussed. Charting, any operative note report, andcommunication with a referring physician are included.
What is included in procedure valuation?CPT 17000 and 17110 series (destruction)Pre-service (before the destruction is done) work: includes areview of pertinent medical records data, a discussion oftreatment choices, a review of risks of the treatment withthe patient, obtaining informed consent, and preparation ofnecessary equipment.Intra-service work: inspection and palpation of lesions toestablish a diagnosis and to specify size, location, depth, andthen the actual destruction with liquid nitrogen freezing.Post-service work: application of any antibiotic ointment anddressings, if needed, and post-procedure patient and familyinstructions. Charting and any communication with areferring physician are included in this work.
“Moreover, where the decision to perform the minor procedure is typicallydone immediately before the service, it is considered a routine preoperativeservice and a visit or consultation is not billed in addition to the procedure.”Medicare Claims Processing Manual, Chapter 12, Section 40.147
Conclusion: all procedures have somebuilt-in E&M component The procedure’s E&M component must be separated fromany additional E&M provided in order to determinequalification for .25 modifier use and the level of anyadditional E&M to be billed. Adequately document the extent of separate E&M workdone and its pertinent clinical justification.
You evaluate a new patient with a history of malignant melanoma. You take ahistory, do a review of systems, do a complete skin examination plus lips,oral mucosa, conjuctivae, palpate lymph node basins and identify a clinicallyatypical pigmented lesion on the arm that you excise.You bill:A)B)C)D)Excision and repair codes 99203 E/M codeExcision and repair codes onlyExcision and repair 99203.25 E/M code*99203 only, and schedule the excision for another day, as E/Mdone on same day as procedure is never coveredWhy? Significant, separately identifiable, medically indicated (and documented)service was done beyond that inherent in the excision.*Some Medicare contractors (e.g., Noridian) do not require appending .25 to aNew patient E/M.49
How to determine a level of E/M separate from thatof a concurrently done procedure? Subtract all E/M included in the procedure from the total E/M done What is left determines level of potentially billable E/M Reminder: the separate service should be reasonable and necessaryYou evaluate a new patient with a history of malignant melanoma. You take a history, do a review of systems, do acomplete skin examination, palpate nodes and identify a clinically atypical pigmented lesion on the arm that you excise.Nevus E/MOverlapSeparate E/M Related to Chief Complaint: History of melanomaExaminationof atypicalnevus,discussion ofremoval need,plan, careHistory, including past melanoma, treatments, interim changes, complaints;Family historyReview of systemsComplete skin examination and inspection of lips, oral mucosa, eyes, nailsPalpation of lymph node basinsDiscussion of melanoma risks, vigilance and prevention strategies50
A patient is referred to you for Mohs surgery. You review pertinent history,evaluate a nasal biopsy-proven BCC and do a 3 stage Mohs excision. You referthe patient out for repair of the defect.You bill:A) Mohs surgery first and 2-3 stages: 17311, 17312x2B) 17311, 17312x2 and 99202.25C) 17311, 17312x2 and 99202.57“The initial evaluation focused upon the lesion being treated is usually included inthe allowance for a minor surgical procedure.” AAD “Audits on Modifier 25 areComing” webinar 12/13/2017Mohs surgery alone is a minor surgical procedure: 0 day global period51
Global Surgical Periods0 Days: MinorProcedureBiopsy (11100 )Shave removal(11300 – 11313)Debridement(11000, 11011-42)Mohs (17311 –17315)10 Days: MinorProcedureDestruction(17000 - 17286)Excisions (11400 –11646)Repairs (12001 –13153)90 Days: MajorProcedureFlapsGraftsTissue ExpandersDestruction ofVascularProliferative Lesion(17106 – 08)No modifier is needed when an E/M or a surgical service isDermabrasion,done at any day following a zero day global surgical procedure Chemical Peel52
Most Common Modifiers Used During theGlobal Period24: Unrelated E/M Service by the Same Physician or Other Qualified Health Care ProfessionalDuring aPostoperative Period25: Significant, Separately Identifiable E/M Service by the Same Physician Or Other QualifiedHealthCare Professional on the Same Day of the Procedure or Other Service57: Decision for Surgery (refers to E/M service resulting in a decision to perform a 90 dayglobal surgery the day of or day after the evaluation)79: Unrelated Procedure or Service by the Same Physician or Other Qualified Health CareProfessional During the Postoperative Period58: Staged or Related Procedure or Service by the Same Physician or Other Qualified HealthCare Professional During the Postoperative Period53
Global Surgical Package Includes all normal/usual preoperative, intraoperative andpostoperative services Included postoperative services are limited to the globalperiod Payment for the procedure includes usual services withinthe global period, including wound care/checks and sutureremoval The global period applies to both the surgeon and tophysicians of the same specialty in a group practice whomay do postoperative care for the patient54
Group Practice and Surgical Follow-up When services are furnished by a physician of the same specialty withina group practice the services are considered part of the global surgicalpackage. Separate coding/billing is not appropriate. If the patient were new to a physician of a different specialty within thegroup practice or the physician of any specialty were independent of thegroup practice, then an appropriate E/M office visit would be billable.Global Surgery Fact Sheet, lSurgery-ICN907166.pdf55
Services included in Global PackageIncludedNot Included Initial evaluation to determine 0or 10 day global procedure need Treatment of complications notrequiring operating room care Postop visits related to surgery Pain management Routine surgical site care: Initial evaluation to determine 90day global surgery need Treatment of complications inthe operating room Visits unrelated to the diagnosisleading to the surgical procedure Additional treatment unrelatedto the surgery Staged procedures Unrelated procedures– Dressing changes– Sutures/staples removal56
Medicare definition: Operating/Procedure Room“A place of service specifically equipped and staffed for the solepurpose of performing procedures”OR/Procedure RoomNOT OR/Procedure Room Room exclusively used andstaffed for procedures/surgeries Laser suite Your office procedure/surgeryroom if it meets the definition Patient examination room Multipurpose patient treatmentroom Any location not usedexclusively for doingprocedures/surgeriesConclusion: if a postoperative complication requires surgical treatment in theoffice setting, and that treatment is done in a room used exclusively forprocedures/surgeries, then that treatment is billable with an appended .78modifier.57
Steps for Optimal Coding Determine level of E/M service &/orProcedure type(s) Correlate ICD-10 diagnoses with CPT codes Select Modifiers if needed Document appropriately to justify billing58
CPT and ICD-10 CodesCorrelate CPT code with corresponding ICD-10 code(s)Example:Established patient with history of melanoma, evaluated for several lesionsEvaluation established diagnosis, treatment and plan for the following:Dx and ServiceCPT CodeICD-10 Code(s)H/O MM: Hx, ROS, complete skinexam, nodal palpation, discussion99213Z85.820 (Personal Hx MM)L82.1 (SKs found)Actinic keratoses17000, 17003 (or 17004) (destruc.)L57.0BCC, on back17261 (desctruc., malig., 0.6-1 cm)C44.519Atypical nevus, on chest11100 (biopsy)D48.5 (neoplasm, uncertain behav.)Append modifiers as appropriate59
Next step: Modifier needed? If two or more procedures are done, which one(s) qualify for a modifier? Which codes are primary (no modifier), and which qualify for amodifier?Multiple procedures: consult National Correct Coding ng/NationalCorrectCodInitEd/index.html?redirect /NationalCorrectCodinitEd/ Procedure-to-procedure (PTP or column 1/2) edits Medically Unlikely Edits (MUE)
The purpose of the NCCI Procedure-to-Procedure (PTP) edits is to prevent improperpayment when incorrect code combinations are reported. The NCCI contains one table ofedits for physicians/practitioners and one table of edits for outpatient hospital services.The Column One/Column Two Correct Coding Edits table and the Mutually Exclusive Editstable have been combined into one table and include PTP code pairs that should not bereported together for a number of reasons explained in the Coding Policy Manual. Thepurpose of the NCCI MUE program is to prevent improper payments when services arereported with incorrect units of alCorrectCodInitEd/index.html?redirect /NationalCorrectCodinitEd/61
tCodInitEd/NCCI-Coding-Edits.htmlUpdated quarterly62
NCCI PTP Example: destruction codesPrimarycodeSecondaryCode (appendmodifier)1 Modifier allowed,both paired payable withmodifier (59 &/or 76)
NCCI PTP Example: Destruction/BiopsyPrimarycodeSecondaryCode (appendmodifier)1 Modifierallowed, bothpaired payable withmodifier 59 &/or 76
You freeze 5 actinic keratoses with liquid nitrogen, biopsy two atypical nevi, one on theback and the other, on the abdomen, and destroy a 1.2 cm wide superficial basal cellcarcinoma on the chest with curetting and electrodesiccation.Per NCCI PTP edits, 17000, 17004 are column 1 codes 17562 and 11100 are column 2 codes 11101 is not listed in column 2Conclusion: 17000, 17004 are primary to both malignant destruction and tobiopsy codes (and to shave removal codes, as well) Append .59 modifier to biopsy and malignant destruction codespaired with destruction of actinic keratoses Add-on codes (i.e., 11101, 17003) do not require a .59 modifier65
8 stages of Mohs done on Medicarepatient. Your MAC is likely to pay for:A.B.C.D.E.All 8 stages, CPT 17311 and 17312x7Only 4 stages, CPT 17311 and 17312x3Only 5 stages, CPT 17311 and 17312x4Only 6 stages, CPT 17311 and 17312x5Only 7 stages, CPT 17311 and 17312x6
Answer: E, Only 7 stagesWhy? NCCI Medically Unlikely Edits (MUE) Accessible on NCCI website. MUE table lists CPT codes, MUE valueand MAI number (1, 2 or 3)
MUE and MAI for Mohs SurgeryMUE for 17312 is 6, meaning 6 stagesMAI for 17312 is 3, meaning a date of serviced editWhen the MAI is 3, one may appeal an unpaid claim via a redetermination, and theappeal should be upheld as long as: The service was provided The service was correctly coded The service was medically necessary
Modifier 59 Definition“Under certain circumstances, it may be necessaryto indicate that a procedure or service was distinctor independent from other non-E/M servicesperformed on the same day. Modifier 59 is used toidentify procedures/services, other than E/Mservices, that are not normally reported together,but are appropriate under the circumstances.”CPT 2018
Modifier 59, part 2“However, when another already established modifier isappropriate it should be used rather than modifier 59. Only if nomore descriptive modifier is available, and the use of modifier59 best explains the circumstances, should modifier 59 be used.”(color accent added)CPT 2018
Practical -59 Modifier Guidelines Two or more procedures done during one patientencounter:––––Look up NCCI editsDetermine whether both may be payable if a modifier is usedDetermine the primary code (Column 1 in NCCI)Determine the secondary code (Column 2 in NCCI) If secondary code has a modifier indicator of 1, then a modifier canbe used to bypass the NCCI edit– Append -59 &/or -76 modifier to secondary code
“Duplicate” procedures coding Modifier –76 should be appended to procedure(s) orsurgical service(s) to indicate a repeatprocedure/surgery was performed on the same day forpatient management purposes.– eg, 11401, 11401.76 Modifier –91 should be appended to laboratoryprocedure(s) or service(s) to indicate a repeat test orprocedure performed on the same day for patientmanagement purposes.– eg, 88305, 88305.91
Modifier .76 and .91 Use Two basal cell carcinomas destroyed: cheek andforehead, 0.7 and 0.6 cm diam.– Previously code: 17281, 17281.59 Now code: 17281, 17281.76 Histopathology dx. for above lesions:– Basal cell carcinoma, cheek & BCC, forehead– Previously code: 88305.26, 88305.26 Now code: 88305.26, 88305.26.91
Correct -59 Modifier UseCPTModifier992132511100591110117004Keep track: does your MAC follow theabove NCCI guideline conventions? It maynot!NO ModifierNeeded
Incorrect Modifier 59 UseCPTModifier1110017000591700359According to the NCCI, 17000 is the Column 1 code and does not need a modifier.11100 is in Column 2, and would be bundled into the 17000 code, resulting in nopayment for the service, unless one uses a modifier appended to 11100.17003 is an add-on code to 17000 and does not require a modifier.Correct Modifier 59 UseCPTModifier17000170031110059
MLN Matters MM8863 -59 is most used modifier“Associated with considerable abuse and high levels of m
Biopsy Codes . Effective Jan., 1, 2019 Integumentary biopsy codes 11100, 11101 have been deleted New Skin Biopsy codes: 11102 - 11107 . skin only, does not include mucosa Site-specific biopsy codes still applicable . 11755