Transcription
TENNESSEE DEPARTMENT OF HEALTHUPDATE ON THE HEALTHCARESAFETY NETPresented toThe General Assembly,State of TennesseeFebruary 19, 2015John J. Dreyzehner, MD, MPH, Commissioner
Table of ContentsExecutive Summary for the Update on the HealthCare Safety Net .1I.INTRODUCTION.6II.ACCESS TO CARE AND ARRAY OF SERVICES .6A. .Public Health Primary Care Safety Net Expansion .61.Statewide Expansion of the Capacity of Local Health Departments .62.State Funded Expansion of the Capacity of Federally Qualified Health Centers or FQHC Look-ALikes & Local Health Department (LDH) Federally Qualified Health Centers .73.Statewide Expansion of the Capacity of Selected Faith-Based, Community-Based Rural Health andFederally Funded Centers .114.Comparison of HealthCare Safety Net Uninsured Adult Medical Encounters for FY2009-2014.165.Access To Statewide Dental Services .17B. .Behavioral Health Safety Net .20C. .Special Populations.211.Ryan White Part B Funds .21D. .Insurance Options for Uninsured .221.CoverTN .222.CoverKids .223.AccessTN .23E. Pharmacy Assistance .231.III.CoverRX .23SUMMARY .24
List of VisualsTable 1: Non-FQHC Local Health Department Primary Care Clinics .7Table 2: FQHC Growth and State Funding, FY2007-2014 .8Table 3: Community/Faith Based Growth and Funding, FY 2009-2014 .13Table 4: HealthCare Safety- Net Medical Encounters FY 2009 – FY 2014 .16Graph 1: HealthCare Safety Net Primary Care for Uninsured Adults 19-64 Years of Age .2Graph 2: FQHC State Funding Picture FY 2007 – 2014 . 9Graph 3: Uninsured Adult Medical Encounters – FQHC FY 2007 – FY 2014 9Graph 4: Community/Faith Based Funding, FY 2007 – FY 2014 . 13Graph 5: Uninsured Adult Medical Encounters Community/Faith BasedFY 2008 – FY 2014 . .14Graph 6: Adult Primary Care Visits in Local Health Departments and Safety Net ProviderSites, FY2009-2014 (To complement Table 4) .17Graph 7: Safety-Net Dental Providers FY 2008 – FY 2014 . .19Graph 8: Emergency Dental Extractions FY 2008 – FY 2014 19Map 1: Adult Healthcare Safety-Net Provider Sites 3
List of AttachmentsAttachment 1: Map & List of Primary Care Health Professional Shortage Areas (HPSAs)Listings for Primary Care, Dental and Mental Health HPSAs .26Attachment 2: Medically Underserved Areas (MUAs) and Medically UnderservedPopulations (MUPs) .36Attachment 3: Adult Dental Data, FY2012-2013 & FY2013-2014 .39Attachment 4: FQHC Grant Recipients Serving a 30 Mile Radius .42Attachment 5: Local Health Department Primary Care Sites Serving a 30 Mile Radius .43Attachment 6: Community and Faith Based Sites Serving a 30 Mile Radius .44Attachment 7: HealthCare Safety Net Services .45
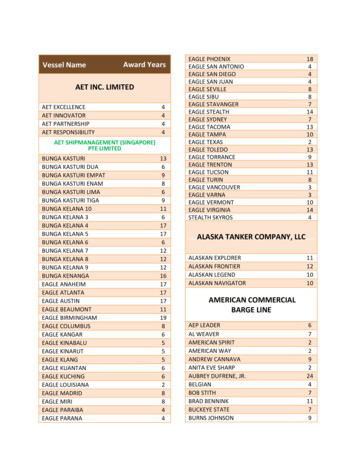
Executive Summary for the Update on the HealthCare Safety NetThe Update to the HealthCare Safety Net Report as prepared by the Tennessee Department ofHealth provides an assessment of the FY 2013-2014 HealthCare Safety Net Program consistentwith the intent of TCA 68-1-123, which is to evaluate “the array of services, adequacy ofservices, and access to care”. This annual update is a comprehensive look of access to carethrough the collaborative efforts among state, public, private not-for-profit and private for profitsectors.Safety Net Support Primary Health Care Services for Uninsured Adults:In FY 13-14 the HealthCare Safety Net Primary Care for Uninsured Adults 19-64 Years of Age,provided a total of six hundred fifty six thousand six hundred forty six (656,646) medicalencounters by all service providers, as compared to six hundred forty eight thousand fourhundred twenty two (648,422) reported in FY 12-13 (1.2% increase). A delineation of medicalencounters by service provider follows with supporting details is referenced in Table 4, page 16of this report. Of the total six hundred fifty six thousand forty six (656,646) medical encounters,the Department of Health’s forty-one (41) Local Health Department (LHD) Clinics notdesignated as Federally Qualified Health Centers (FQHC) provided one hundred twentythousand three hundred twenty eight (120,328) medical encounters, compared to one hundredtwenty nine thousand two hundred four (129,204) reported in FY 12-13 (6.8% decrease); fifteen(15) LDH clinics designated as FQHCs, provided forty thousand nine hundred forty (40,940) ascompared to forty four thousand thirty (44,030) in FY 12-13 (7% decrease); all other FederallyQualified Health Centers (excluding the 15 LDH clinics with an FQHC designation) providedtwo hundred seventy eight thousand eight hundred forty five (278,845) as compared to twohundred eighty eight thousand five hundred eight (288,508) in FY12-13 (3.3% decrease);Community & Faith-Based providers performed two hundred sixteen thousand five hundredthirty three (216,533) as compared to one hundred eighty six thousand six hundred eighty(186,680) in FY 12-13 ( 13.7% increase). The 216,533 encounters were generated byapproximately one hundred one thousand one hundred fourteen (101,114) uninsured adultpatients between the ages of 19-64. Funding is provided through the Tennessee Department ofHealth.1
Graph 1: HealthCare Safety Net Primary Care for Uninsured Adults 19-64 Years of Age700,000HealthCare Safety Net Primary Care for Uninsured Adults 19-64 Yearsof Age656,646648,422600,000Medical 0,00044,03040,9400LHDLHD FQHCFQHCs (Non-LHD)Service ProviderCFBTotal All ProviderTypesIn FY 13-14 continued funding of the case management component of the HealthCare Safety NetPrimary Care Program enabled uninsured adults with assistance obtaining necessary medicalcare and treatment that extends beyond the realm of primary cares services. Programs whichfollow the National Project Access Model include: Nashville Academy of Medicine,Appalachian Mountain; Hamilton County Project Access and Knox County Project Access.These organizations provided care coordination for complicated health issues for seven thousandnine hundred (7,900) uninsured Tennesseans, obtaining access to specialty care, diagnostictesting procedures, in addition to surgery and hospitalization at little to no cost to the patient.Those 7,900 patients generated approximately forty three thousand eight hundred eighty five(43,885) medical encounter visits. Funding is provided through the Tennessee Department ofHealth.2
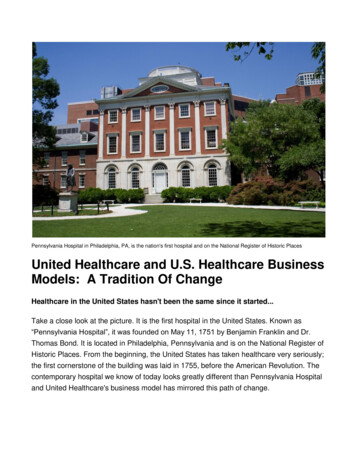
Adult Healthcare Safety Net Provider Sites Now Provided in 88 of 95CountiesThe Safety Net Emergency Dental Program for Uninsured Adults19-64 Years of Age, comprisedof seventeen (17) Dental Providers, performed a total of seventeen thousand nine hundred eightytwo (17,982) extractions in FY 13- 14, as compared to twenty thousand five hundred sixty nine(20,569) in FY 12-13 (12.5 % decrease). Funding is provided through the Tennessee Departmentof HealthIn an effort to help Tennesseans with serious mental illness that lack behavioral health insurancecoverage, the Behavioral Health Safety Net (BHSN) of TN collaborates with community mentalhealth agencies across the state to provide vital services, helping people with serious mentalillness lead functional and productive lives. Services include assessment, evaluation, diagnostic,therapeutic intervention, case management, peer support services, psychosocial rehabilitationservices, psychiatric medication management, labs related to medication management, andpharmacy assistance and coordination.During FY14, the BHSN of TN partnered with fifteen (15) Community Mental Health Agenciesthat provided vital behavioral health services to approximately thirty five thousand five hundredand ten (35,510) individuals across the state of Tennessee. The top three (3) services utilizedwere: Case Management; Office Visit for Evaluation and Pharmacological Management; andIndividual Therapy. Funding for these services is provided through the Department of MentalHealth and Substance Abuse Services.In addition to direct funding support to providers of care for services, the State of Tennesseeenacted a series of insurance products which assisted the uninsured to gain coverage for all orpart of their medical related expenses.3
Cover TN:CoverTN did not meet the Affordable Care Act insurance requirements that went into effect andtherefore CoverTN was suspended by the Cover Tennessee Program on January 1, 2014.Members were sent notices informing them that their coverage would end December 31, 2013,along with information on the federal Health Insurance Marketplace. Individuals now haveaccess to coverage through the Health Insurance Marketplace or through their employer in thefederally-run Small Business Health Options Program (SHOP) Exchange.CoverKids continues to provide health coverage to children whose families earn within 250percent of the federal poverty level (FPL), which was 59,625 per year for a family of four in2014, as well as, providing unborn/maternity coverage through HealthyTNBabies. With thepassage of the Affordable Care Act and access to the Health Insurance Marketplace, themembers in the CoverKids buy-in program were notified in September, 2013 that their coveragewould end December 31, 2013. The CoverKids buy-in program, which was state funded,required members to pay premiums as their income was above the threshold for the CoverKidsprogram. CoverKids buy-in program members were supplied with information on how to contactthe Health Insurance Marketplace through the internet or by phone for coverage options.AccessTN members with incomes at or below the federal poverty level AND who receivepremium assistance were able to maintain their coverage in 2014. Individuals above the federalpoverty level and/or not receiving premium assistance were allowed to maintain their coveragethrough April 30, 2014. This extension allowed these individuals to find alternative coveragethrough the Health Insurance Marketplace open enrollment period active through March 31,2014 to allow consumers an opportunity to transition insurance coverage prior to April 30, 2014.Effective January 1, 2014, CoverRx continued to provide pharmacy assistance to eligibleTennesseans below the federal poverty level including members of the Mental Health Safety Netpopulation.Summary of Changes to Tennessee Healthcare Safety Net in 2014Safety Net funding now provides access to primary health care for uninsured adults in 88 ofTennessee’s 95 counties. During the past three years, a total of six (6) new contracts have beenadded to the Community and Faith Based practices and Community Health Centers (FQHCs) inthe following counties; Rutherford, Lewis, Davidson, and Claiborne, Macon and Williamson.Funding partially reimburses providers for their costs of care through payments for each visitdocumented and billed to the State. With support from the 12 million recurring appropriation, atotal of 536,318 visits to Community and Faith Based Clinics, Federally Qualified Health Center,and Project ACCESS Providers were delivered in 2014 representing a 3.2 percent increase overthe previous year.4
The enactment of the Patient Protection and Affordable Care Act of 2010, which introducedspecific insurance eligibility requirements and the Health Insurance Market Place, significantlyimpacted CoverTN, the CoverKids buy-in program and AccessTN members whose incomeexceeds the federal poverty level. Subsequently, both CoverTN and the CoverKids buy-inprograms were discontinued effective December 31, 2013, along with coverage for affectedAccessTN members, ending on April 30, 2014. This resulted in thirteen thousand six hundredtwenty three (13,623) CoverTN members, three hundred forty three (343) CoverKids Buy-Inprogram members and four hundred ninety one (491) AccessTN members being redirected toaccess alternative insurance coverage through the Health Insurance Market Place or theiremployer sponsored health insurance programs, including the federal Small Business HealthOptions Program (SHOP) Exchange.Affordable Care Act Health Insurance Enrollment Navigator programs, outreach andenrollment staff funded through federal grants from ACA was assigned to provide in-personHealth Insurance Marketplace enrollment assistance to uninsured individuals at safety-netprovider’s sites, including Community Health Centers, Community Faith Based organizationsand Local Health Departments. One hundred fifty one thousand three hundred fifty two(151,352) Tennesseans enrolled, state-wide during the first open enrollment period betweenOctober 1, 2013 and March 31, 2014. As of December 15, 2014, eighty seven thousand onehundred thirty seven (87,137) Tennesseans have enrolled (including re-enrollments from theprevious year) during the current open enrollment period which is active from November 15,2014 through February 15, 2015.Safety-Net provider sites are a premium access point for providing people with assistanceenrolling in the Health Insurance Marketplace. The safety-net patient demographic is comprisedof the uninsured, low-income, disproportionately poor and in many communities they are amember of a racial, ethnic or cultural minority, challenged with transportation, distance orgeographic barriers to access care, and experience unmet health needs due to delayed care or lackof preventative care. Even if this vulnerable population of uninsured adults obtains healthinsurance through the Affordable Care Act, evidence points to a continuing issue of affordabilityof new insurance premiums, co-pays, deductibles, and other out-of-pocket expenses whichcreates an additional barrier to accessing care. The Adult Health Care Safety-Net provides adedicated stream of funding support to safety-net patients navigating economic challenges andaccess to a medical home for patients whose health needs would have been unmet.5
I.INTRODUCTIONThis report is provided in response to Tennessee Code Annotated 68-1-123, which requires theCommissioner of Health, in consultation with the Department of Finance and Administration andany other state agencies involved in the administration of the HealthCare Safety Net Program toprovide a report to the General Assembly regarding data relating to access to care and healthcaresafety net adequacy related issues. The aforementioned report addresses the allocation of scarcehealthcare resources with attention to assuring a safety net of for access to health services thatare part of community systems of care in rural and underserved areas across the state. Pleasenote that this report is due following a calendar year period; however, references to allocationof funding and service provision throughout the report are based on the State’s fiscal year.II.ACCESS TO CARE AND ARRAY OF SERVICESA.Public Health Primary Care Safety Net Expansion1.Statewide Expansion of the Capacity of Local Health DepartmentsOn January 1, 2006, the Department of Health initiated a statewide expansion of primary careservices to uninsured adult Tennesseans in the following ways: (1) increasing access for acuteand episodic care and chronic disease management; and (2) offering the “best care possible” viapreventive physical exams and essential health screenings. These strategies assist in individualpreventive health maintenance, which in turn aids significant reduction in unnecessaryhospitalizations. Prior to the safety net statewide expansion of primary care services on January1, 2006, local health departments in seventeen (17) counties across the state provided primarycare in a total of twenty (20) sites. At present, primary care services are provided in fifty-six (56)local health department (LHD) sites in fifty-one (51) of Tennessee’s ninety-five (95) counties,including fifteen (15) Department of Health Federally Qualified Health Center (FQHC) clinicsites located in fifteen (15) counties of the state.In fiscal year 2013-14, forty-one (41) local health department (LHD) sites provided,approximately one hundred twenty thousand three hundred twenty eight (120,328) uninsuredadult medical encounters to adult Tennesseans nineteen (19) to sixty-four (64) years of age, adecrease of approximately seven (7) percent from the Department of Health’s uninsured adult6
encounters in FY2012-2013. 1 The aforementioned encounter numbers do not include the fifteen(15) local health departments operated by the Department of Health that are designated FQHCs.The visit numbers of the forty-one (41) local health department sites are included in Table 1.Table 1: Non-FQHC Local Health Department Primary Care ClinicsNon-FQHC Local Health Department Primary Care ClinicsPrimary Care Age Groups19-20 Years21-24 Years25-29 Years30-34 Years35-39 Years40-44 Years45-49 Years50-54 Years55-59 Years60-64 YearsGrand TotalUninsured Adult 42416,94720,29016,82313,077120,328In conjunction with primary care services, LHDs offer prescription medications, includinggeneric drugs, priority drug groups, patient drug assistance programs and referral for specialtycare when necessary. For example, some local health departments have partnered with localhospitals to offer discounted diagnostic services or a limited amount of diagnostics at no chargefor uninsured adult health department patients. Also, some local hospitals have allowed thehealth department online access to emergency room records. Finally, in addition to expandedprimary care services at many local health departments, all health departments continue toprovide traditional public health services such as Family Planning, Communicable DiseaseSurveillance and Management, Breast and Cervical Cancer Screening, Immunizations, andWomen, Infants, and Children (WIC) services.2.State Funded Expansion of the Capacity of FQHCs, FQHC Look-A-Likes & LDH FQHCsIn fiscal year 2007, twenty-three (23) provider organizations designated as FQHCs (FederallyQualified Health Centers, a Medicare and Medicaid reimbursement designation for organizationsthat offer a broad range of primary care and prevention services including Community Health1In response to compliance with 2012 Tenn. Pub. Acts, ch. 1061 (the “Eligibility Verification for Entitlements Act”) as requiredby Tenn. Code Ann. § 4-57-106(b). The Tennessee Department of Health, including local health departments, boards andcommissions, has implemented protocols and policies to verify that every adult applicant for “public benefits” is a United Statescitizen or a “qualified alien”, within the meaning of Chapter 1061.7
Center Organizations that receive United States Public Health Service Section 330 GrantFunding) with a total of eighty-four (84) sites received 6 million in funding to expand existingcapacity of primary care services in forty-one (41) of Tennessee’s ninety-five (95) counties.This provided funding for a total of two hundred seventeen thousand six hundred seventy-three(217,673) uninsured adult medical encounters. In fiscal year 2008 the funding allocationincreased to 7.6 million comprised of 4.6 million of recurring funding and 3 million of nonrecurring funding. The funding allocation decreased to 6.9 million in fiscal year 2009,continuing to decrease to 6 million in fiscal year 2010 where it has remained consistent at thisamount throughout fiscal years 2010 to 2014. The number of uninsured adult medical encounterssteadily increased from fiscal years 2007 to 2011 and peaked at three hundred six thousand threehundred thirty six (306,336) in fiscal year 2012. This upward trend of utilization is reflective ofan economic downturn perpetuating a high unemployment rate and subsequent loss of employersponsored health insurance resulting in an increased number of uninsured adults during this time.As the economic status began to improve, the number of medical encounters began to decrease,as is reflective in fiscal year 2013 where the number of medical encounters progressivelydecreased to two hundred eighty eight thousand five hundred eight (288,508) and furtherdecreased to two hundred seventy eight thousand eight hundred forty five in fiscal year 2014.Table 2: FQHC Growth and State Funding Picture FY 2007 – FY 2014FQHC State Funding Picture FY2007-FY2014State Fiscal Year PeriodAllocationNumber of Uninsured AdultMedical EncountersFY 2007 6,000,000217,673FY 2008 7,600,000241,737FY2009 6,900,000280,404FY2010 6,000,000296,942FY2011 6,000,000294,427FY2012 6,000,000306,336FY2013 6,000,000288,508FY2014 6,000,000278,8458
Graph 2: State Funding Support for Primary Care Services at FQHCs FY 2007 – FY 2014FQHC State Funding Picture FY2007-FY2014 8,000,000 7,600,000 7,500,000 7,000,000 6,900,000 6,500,000 6,000,000 6,000,000 6,000,000 6,000,000 5,500,000 6,000,000 6,000,000 6,000,000 5,000,000 4,500,000 3FY2014Graph 3: Uninsured Adult Medical Encounters FY 2007 – FY 2014Uninsured Adult Medical Encounters - 3FY20149
Currently, there are twenty-seven (27) community health center FQHCs and one (1) FQHCLook-A-Like in Tennessee with just over 200 service delivery sites. Delivery sites includeprimary care service delivery sites, dental service delivery sites, and other miscellaneous servicedelivery sites such as school based health centers and homeless clinics. Note: Attachment 7 listsonly Safety Net primary care FQHC sites.These private, nonprofit, community-directed health care facilities provide high-quality, costeffective and comprehensive primary and preventive care to medically underserved anduninsured Tennesseans. In 2013 FQHCs in Tennessee provided care to over 396,000 patients.According to the Tennessee Primary Care Association (TPCA), on average approximately 40%of community health center patients are uninsured; however, that number may be as high as 80%for some centers. Nearly 80% of the total FQHC patients have income levels below 100% of theFederal Poverty Level. Historically, community health centers participated in Health DisparitiesCollaborative, a national effort to improve health outcomes for all medically underserved peoplewith chronic diseases, such as diabetes, cardiovascular disease, depression and asthma. Thisinitiative prepared community health centers to begin transforming their practices into PatientCentered Medical Homes (PCMHs). The patient-centered medical home is a “way of organizingprimary care that emphasizes care coordination and communication to transform primary careinto ‘what patients want it to be.’ Medical homes can lead to higher quality and lower costs, andcan improve patients’ and providers’ experience of care.” (National Committee for QualityAssurance). Health centers in Tennessee are working on PCMH Recognition through theNational Committee for Quality Assurance (NCQA) or Primary Care Medical HomeCertification through The Joint Commission (TJC). The first Tennessee health center achievedPCMH Certification in March 2013. Through October 2014, thirty eight (38) sites from eleven(11) health centers have achieved PCMH Recognition or Certification.These centers are also working hard to improve clinical quality. The Center for Quality inCommunity Health is a network of Community Health Centers and partners that supports acontinually evolving health care system by sharing information and expertise to facilitatelearning, support quality improvement and develop leadership. Through the use of timely,relevant data, the Center for Quality in Community Health promotes collaboration, sustainability,cost effectiveness and healthier communities in Tennessee.With the exception of two centers, all Tennessee community health centers now have anelectronic health record and will continue working towards achieving meaningful use federalcriteria. Community Health Centers are consistently providing the recommended standards ofcare for the aforementioned chronic health conditions, which should result in improved healthoutcomes for participants. In addition, all Community Health Centers are eligible and mayparticipate in the federal 340B Drug Pricing Program, which provides significant savings onpharmaceuticals for their patients.10
Many Tennessee community health centers are using the advanced technology of telehealth toimprove patient access to primary and specialty care. Telehealth uses electronic information andtelecommunications technologies to support long-distance clinical health care, patient andprofessional health-related education, public health and health administration.2 Nationwidestudies have found that telehealth can reduce the cost of health care, reduce travel times, andresult in better management of chronic diseases.3 Additionally, some Community Health Centersare using telehealth to provide care to students in public schools. The use of telehealth in schoolscan reduce student absenteeism, reduce the amount of work missed by parents to transportchildren to physicians’ offices, and improve school nursing staffing requirements.42A diabetes self-management telehealth pilot project was conducted from March through June of2013, as a collaborative initiative among the Tennessee Department of Health, the TennesseePrimary Care Association and local Community Health Centers. The goal was to increase accessto supplemental primary care services for uninsured adult patients dually diagnosed with diabetesand depression. The intention was to provide nutritional and behavioral counseling to improvediabetes self-management outcomes for adult patients diagnosed with diabetes who receivedprimary care through one of five (5) contracted Community Health Center safety net providers.The target patient population selected for a telehealth consult was patients diagnosed withdiabetes and screened as positive for depression or those who were referred because ofcontinuing self-management issues related to diet and weight issues. Patients referred for atelehealth consultation received a nutritional consult from a designated Tennessee Department ofHealth nutritionist and a behavioral health telehealth consult provided by an East TennesseeState University Staff, Clinical Psychologist. The outcome of this pilot was a successfuldemonstration of telehealth as an effective means of remote access to patient care from both thepatient and telehealth consultant perspective. Alleviating distance as an access barrier to careincreased the likelihood of returned patient visits for subsequent consults which is directlyassociated with enhanced patient self-management outcomes. Additionally, this pilot also provedtelehealth services as a successful technology to support an interdisciplinary health care teamapproach for patient care.3.Statewide Expansion of the Capacity of Selected Faith-Based, Community-Based RuralHealth, and Federally Funded CentersIn September of 2005, the Department of Health received an appropriation of approximately 6.3million by the General Assembly. The Department of Health accepted applications, reviewed,21 U.S.Department of Health Resources Services Administration. elehealth Association. ?pageID icantelemed.org/i4a/pages/index.cfm?pageID 33084 American Telehealth Association2 American11
and awarded grant applications for expansion of primary care services among faith-based,community-based, rural health, and other federally funded centers. The grant process funded anadditional sixty-seven (67) healthcare safety net providers and created expanded capacity inforty-four (44) counties. From July 15, 2005 (date of actual TennCare disenrollment) throughJune 30, 2006, this further expansion of the healthcare safety net resulted in basic primary carefor an additional fifty seven thousand six hundred seventy one (57,671) uninsured adultTennesseans (visit data was not requir
The Safety Net Emergency Dental Program for Uninsured Adults1964 Ye- ars of Age, comprised of seventeen (17) Dental Providers, performed a total of seventeen thousand nine hundred eighty two (17,982) extractions in FY 13- 14, as compared to twenty thousand five hundred sixty nine of Health