Transcription
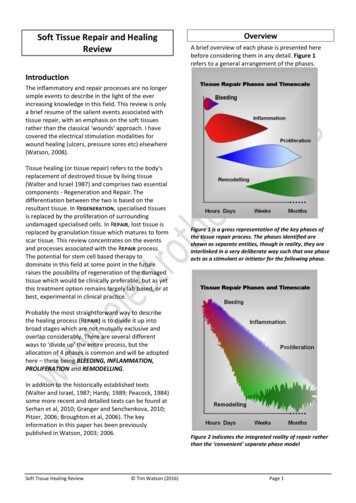
Soft Tissue Repair and HealingReviewOverviewA brief overview of each phase is presented herebefore considering them in any detail. Figure 1refers to a general arrangement of the phases.IntroductionThe inflammatory and repair processes are no longersimple events to describe in the light of the everincreasing knowledge in this field. This review is onlya brief resume of the salient events associated withtissue repair, with an emphasis on the soft tissuesrather than the classical 'wounds' approach. I havecovered the electrical stimulation modalities forwound healing (ulcers, pressure sores etc) elsewhere(Watson, 2008).Tissue healing (or tissue repair) refers to the body'sreplacement of destroyed tissue by living tissue(Walter and Israel 1987) and comprises two essentialcomponents - Regeneration and Repair. Thedifferentiation between the two is based on theresultant tissue. In REGENERATION, specialised tissuesis replaced by the proliferation of surroundingundamaged specialised cells. In REPAIR, lost tissue isreplaced by granulation tissue which matures to formscar tissue. This review concentrates on the eventsand processes associated with the REPAIR process.The potential for stem cell based therapy todominate in this field at some point in the futureraises the possibility of regeneration of the damagedtissue which would be clinically preferable, but as yetthis treatment option remains largely lab based, or atbest, experimental in clinical practice.Figure 1 is a gross representation of the key phases ofthe tissue repair process. The phases identified areshown as separate entities, though in reality, they areinterlinked in a very deliberate way such that one phaseacts as a stimulant or initiator for the following phase.Probably the most straightforward way to describethe healing process (REPAIR) is to divide it up intobroad stages which are not mutually exclusive andoverlap considerably. There are several differentways to ‘divide up’ the entire process, but theallocation of 4 phases is common and will be adoptedhere – these being BLEEDING, INFLAMMATION,PROLIFERATION and REMODELLING.In addition to the historically established texts(Walter and Israel, 1987; Hardy, 1989; Peacock, 1984)some more recent and detailed texts can be found atSerhan et al, 2010; Granger and Senchenkova, 2010;Pitzer, 2006; Broughton et al, 2006). The keyinformation in this paper has been previouslypublished in Watson, 2003; 2006.Soft Tissue Healing Review Tim Watson (2016)Figure 2 indicates the integrated reality of repair ratherthan the ‘convenient’ separate phase modelPage 1
BLEEDING PHASEThis is a relatively short lived phase, and will occurfollowing injury, trauma or other similar insult.Clearly if there has been no overt injury, this will beof little or no importance, but following soft tissueinjury, there will have been some bleeding. Thenormal time for bleeding to stop will vary with thenature of the injury and the nature of the tissue inquestion. The more vascular tissues (e.g. muscle) willbleed for longer and there will be a greater escape ofblood into the tissues. Other tissues (e.g. ligament)will bleed less (both in terms of duration andvolume). It is normally cited that the intervalbetween injury and end of bleeding is a matter of afew hours (4-6 hours is often quoted) though this ofcourse is the average duration after the averageinjury in the average patient. Some tissues maycontinue to bleed for a significantly longer period,albeit at a significantly reduced rate.INFLAMMATORY P HASE : OVERVIEWThe inflammatory phase is an essential component ofthe tissue repair process and is best regarded in thisway rather than as an 'inappropriate reaction' toinjury. There are, of course, numerous other initiatorsof the inflammatory process (e.g. repetitive minortrauma, mechanical irritation), though for thepurpose of this paper, the injury model will beadopted. The inflammatory phase has a rapid onset(few hours at most) and swiftly increases inmagnitude to its maximal reaction (1-3 days) beforegradually resolving (over the next couple of weeks). Itcan result in several outcomes (see below) but interms of tissue repair, it is normal and essential. Theonset and resolution are swifter in more vasculartissues and slower in the relatively poorlyvascularised tissues. The alternative initiators of theinflammatory events include mechanical irritation,repeated minor trauma, excessive heating andcooling plus others that may be less significant intherapy such as infection and a wide range ofautoimmune disorders. The inflammatory events areessentially the same whichever 'route' is relevant forthe initiation.PROLIFERATION PHASE : OVERVIEWThe proliferative phase essentially involves thegeneration of the repair material, which for themajority of musculoskeletal injuries, involves theproduction of scar (collagen) material. Theproliferative phase has a rapid onset (24-48 hours)but takes considerably longer to reach its peakreactivity, which is usually between 2-3 weeks postSoft Tissue Healing Review Tim Watson (2016)injury (the more vascular the tissue, the shorter thetime taken to reach peak proliferative production).This peak in activity does not represent the time atwhich scar production (repair) is complete, but thetime phase during which the bulk of the scarmaterial is formed. The production of a finalproduct (a high quality and functional scar) is notachieved until later in the overall repair process. Ingeneral terms it is usually considered thatproliferation runs from the first day or two postinjury through to its peak at 2-3 weeks anddecreases thereafter through to a matter of severalmonths (typically 4-6) post trauma.REMODELLING PHASE : OVERVIEWThe remodelling phase is an often overlooked phaseof repair in terms of its importance, especially in thecontext of therapy and rehabilitation. It is neitherswift nor highly reactive, but does result in anorganised, quality and functional scar which iscapable of behaving in a similar way to the parenttissue (that which it is repairing). The remodellingphase has be widely quoted as starting at aroundthe same time as the peak of the proliferative phase(2-3 weeks post injury), but more recent evidencewould support the proposal that the remodellingphase actually starts rather earlier than this, and itwould be reasonable to consider the start point tobe in the first week.The final outcome of these combines events is thatthe damaged tissue will be repaired with a scarwhich is not a ‘like for like’ replacement of theoriginal, but does provide a functional, long term‘mend’ which is capable of enabling qualityrecovery from injury. For most patients, this is aprocess that will occur without the need for drugs,therapy or other intervention. It is designed tohappen, and for those patients in whom problemsare realised, or in whom that magnitude of thedamage is sufficient, some ‘help’ may be required inorder to facilitate the process. It would be difficultto argue that therapy is ‘essential’ in some sense.The body has an intricately complex and balancedmechanism through which these events arecontrolled. It is possible however, that in cases ofinhibited response, delayed reactions or repeatedtrauma, therapeutic intervention is of value.It would also be difficult to argue that there was anyneed to change the process of tissue repair. If thereis an efficient (usually) system through which tissuerepair is initiated and controlled, why would therebe any reason to change it? The more logicalPage 2
approach would be to facilitate or promote thenormality of tissue repair, and thereby enhance thesequence of events that take the tissues from theirinjured to their ‘normal’ state. This is the argumentthat will be followed in this paper – the promotion ofnormality, rather than trying to achieve a betternormality. The best of the available evidence wouldalso support this approach.If the tissue repair process is slowed, stalled or insome way delayed, encouraging the 'normal'sequence is the best evidenced way forward. This canbe achieved with the same essential techniques asthose used for a 'normally' progressing repairsequence, though it may take a 'stronger' or more'intense' therapy to initiate a tissue response.Figure 3 represents the often encountered 'delayed'healing seen by many therapistsIn therapy practice, our view of tissue repair issomewhat skewed by the patients that are seen(Figure 3). The majority of patients whose tissues arerepairing 'on track' do not need therapy help in orderto achieve a quality result. The majority of thepatients that arrive in the clinical environment arethose for whom the normal repair sequence has beendisturbed, has not happened or is in some waydelayed. Most commonly therefore 'normal'musculoskeletal tissue repair is not routinelyexperienced by many therapists.The mechanism through which therapy can beeffective throughout the repair sequence is becomingbetter understood, though as a general comment,these effects appear to be achieved by 'stimulating'rather than 'changing' the events.Soft Tissue Healing Review Tim Watson (2016)Inflammatory EventsInflammation is a normal and necessaryprerequisite to healing (Aller et al, 2006; Hardy1989; Serhan et al 2010 with Medzhitov (2008) andmore recently, Dakin et al (2014) and Rees et al(2014) providing insightful analyses). Following thetissue bleeding which clearly will vary in extentdepending on the nature of the damage, a numberof substances will remain in the tissues which makea contribution to the later phases. Fibrin andfibronectin form a substratum which is hospitableto the adhesion of various cells.The complex chemically mediated amplificationcascade that is responsible for both the initiationand control of the inflammatory response can bestarted by numerous events, one of which istrauma. Mechanical irritation, thermal or chemicalinsult, and a wide variety of immune responses aresome of the alternative initiators, and for a widerange of patients experiencing an inflammatoryresponse in the musculoskeletal tissues, these aremore readily identified causes. For the purposes ofthis review, only the traumatic route will bepursued though the key events and control systemsinvolved in an inflammatory response subsequentto mechanical irritation etc are all but identical.There are two essential elements to theinflammatory events, namely the vascular andcellular cascades. Importantly, these occur inparallel and are significantly interlinked. Figure 4summarises the essential elements of theinflammatory cascade. The chemical mediators thatmake an active contribution to this process aremyriad. They are usefully summarised in severalreviews including Jiminez and Jiminez, (2004) andSinger and Clark (1999). Whilst these are clearly notthe newest reviews, they do provide a usefulbackground to the topic. Smith et al (2008) providea useful review of the mediators associated withmuscle injury, whilst Molloy et al (2003) havereviewed the role of these mediators in relation toligament and tendon injury. Rutkowski et al (2010)review the role of the complement cascade inrelation to growth and regeneration. A moredetailed account can be found in Serhan et al(2010).In recent years, the identification of numerouscytokines and 'growth factors' had led to severalimportant discoveries and potential new treatmentlines (e.g. Wagner et al 2003; Leung et al 2006). ThePage 3
effect of various therapies on the cytokine cascades isbecoming more obvious with the increasing volumeof research in this field (further reference support inthe latter part of this paper).VASCULAR EVENTSIn addition to the vascular changes associated withbleeding, there are also marked changes in the stateof the intact vessels. There are changes in the calibreof the blood vessels, changes in the vessel wall and inthe flow of blood through the vessels. Vasodilationfollows an initial but brief vasoconstriction andpersists for the duration of the inflammatoryresponse. Flow increases through the main channelsand additionally, previously dormant capillaries areopened to increase the volume through the capillarybed.The cause of this dilation is primarily by chemicalmeans (histamine, prostaglandins and complementcascade components C3 and C5 and many others)whilst the axon reflex and autonomic system mayexert additional influences. There is an initial increasein velocity of the blood followed by a prolongedslowing of the stream. The white cells marginate,platelets adhere to the vessel walls and theendothelial cells swell.In addition to the vasodilation response, there is anincrease in the vasopermeability of the local vessels(also mediated by numerous of the chemicalmediators), and thus the combination of thevasodilation and vasopermeability response is thatthere is an increased flow through vessels which aremore ‘leaky’, resulting in an increased exudateproduction.The flow and pressure changes in the vessels allowsfluid and the smaller solutes to pass into the tissuespaces. This can occur both at the arterial and venousends of the capillary network as the increasedhydrostatic pressure is sufficient to overcome theosmotic pressure of the plasma proteins. The vesselsshow a marked increase in permeability to plasmaproteins. There are several phases to thepermeability changes but essentially, there is aseparation of the endothelial cells, particularly in thevenules, and an increased escape of protein richplasma to the interstitial tissue spaces. The chemicalmediators responsible for the permeability changesinclude histamine, serotonin (5-HT), bradykinin andleukotreines together with a potentiating effect fromthe prostaglandins.Soft Tissue Healing Review Tim Watson (2016)INFLAMMATIONTissue Damage /Insult / InjuryMast Cells,PlateletsChemical eChemical raction ofPhagocytes(Neutrophils,PMN’s)Increase FlowVolumeIncrease isClearanceMacrophagesRelease of ProliferativemediatorsFigure 4 : Key Inflammatory elementsThe effect of the exudate is to dilute any irritantsubstances in the damaged area and due to the highfibrinogen content of the fluid, a fibrin clot can alsoform, providing an initial union between thesurrounding intact tissues and a meshwork whichcan trap foreign particles and debris. The meshworkalso serves as an aid to phagocytic activity (seebelow). Mast cells in the damaged region releasehyaluronic acid and other proteoglycans which bindwith the exudate fluid and create a gel which limitslocal fluid flow, and further traps various particlesand debris (Hardy 1989).CELLULAR EVENTSThe cellular components of the inflammatoryresponse include the early emigration (withinminutes) of the phagocytes (neutrophils;polymorphonucleocytes or PMN's) from the vessels.This is followed by several other species leaving themain flow, including monocytes, lymphocytes,eosinophils, basophils (Lorena et al 2002) andsmaller numbers of red cells (though these leavethe vessel passively rather than the activeemigration of the white cells). Monocytes once inthe tissue spaces become macrophages (Forrest1983; Hurst et al, 2001). The main groups ofchemical mediators responsible for chemotaxis arePage 4
some components of the complement cascade,lymphokines, factors released for the PMN's andpeptides released from the mast cells in the damagedtissue (Rankin, 2004; Egozi et al 2003; Luster, 1998;Vernon-Roberts 1988). Butterfield et al (2006)usefully consider the beneficial and the potentiallydetrimental effects of neutrophila and macrophagesin inflammation.The PMN escapees act as early debriders of thewound. Numerous chemical mediators have beenidentified as having a chemotactic role, for example,PDGF (platelet derived growth factor) released fromdamaged platelets in the area. Components of thecomplement cascade (C3a and C5a), leukotreines(released from a variety of white cells, macrophagesand mast cells) and lymphokines (released frompolymorphs) have been identified (see Walter andIsrael 1987; Vernon-Roberts 1988; Dierich et al 1987;Smith et al 2008)These cells exhibit a strong phagocytic activity andare responsible for the essential tissue debridementrole. Dead and dying cells, fibrin mesh and clot resideall need to be removed. As a ‘bonus’, one of thechemicals released as an end product of phagocytosisis lactic acid which is one of the stimulants ofproliferation – the next sequence of events in therepair process.The inflammatory response therefore results in avascular response, a cellular and fluid exudate, withresulting oedema and phagocytic activation. Thecomplex interaction of the chemical mediators notonly stimulates various components of theinflammatory phase, but also stimulates theproliferative phase. The course of the inflammatoryresponse will depend upon the number of cellsdestroyed, the original causation of the process andthe tissue condition at the time of insult.INFLAMMATORY OUTCOMESResolution is a possible outcome at this stage oncondition that less than a critical number of cells havebeen destroyed. For most patients that come to ourattention, this is an unlikely scenario unless tissueirritation rather than overt damage is the initiator.There is some considerable debate with regard 'microinjury' or 'micro trauma' and whether it leads to arepair event or a resolution. It is possible that theyshould result in a micro repair, and if the tissues failto respond in this way, the microdamaged tissue failsto mount a repair response, thus resulting inSoft Tissue Healing Review Tim Watson (2016)accumulative damage and possible longer termissues. This debate continues with interestingevidence e.g. Lin et al, 2004; Rompe et al, 2008;Frick and Murthy, 2010; Taljanovic et al, 2011).Widgerow (2012) authors an interesting paperlooking at the naturally occurring 'stop' signals forthe inflammatory events.Figure 5 : Inflammatory OutcomesSuppuration, in the presence of infective microorganisms will result in pus formation. Pus consistsof dead cell debris, living, dead and dyingpolymorphs suspended in the inflammatoryexudate. Clearly the presence of an infection willdelay the healing of a wound (Zederfelt 1979).Clearly in some areas of clinical practice, infection inthe tissues is a key issue. Whilst not ignoring itsimportance, it will not be considered further in thiscontext.Chronic inflammation does not necessarily implyinflammation of long duration, and may follow atransient or prolonged acute inflammatory stage(Vernon-Roberts 1988). Essentially there are twoforms of chronic inflammation : either the chronicreaction supervenes on the acute reaction or may infact develop slowly with no initial acute phase (abinitio) (Hurley 1985). Chronic inflammation ab initiocan have many causes including local irritants, poorcirculation, some micro-organisms or immunedisturbances. Chronic inflammation is usually moreproductive than exudative - it produces morefibrous material than inflammatory exudate.Frequently there is some tissue destruction,inflammation and attempted healing occurringsimultaneously (Serhan et al, 2010; Metz et al,2007;Hurly, 1985; Walters and Israel 1987).Healing/ Repair by fibrosis will most likely be takingplace in the tissue repair scenario considered here.The fibrin deposits from the inflammatory stage willbe partly removed by the fibrinolytic enzymes (fromthe plasma and PMN's) and will be graduallyreplaced by granulation tissue which becomesPage 5
organised to form the scar tissue. Macrophages arelargely responsible for the removal of the fibrin,allowing capillary budding and fibroblastic activity toproceed (proliferation). The greater the volume ofdamaged tissue, the greater the extent of, and thegreater the density of the resulting scar tissue.Chronic inflammation is usually accompanied bysome fibrosis even in the absence of significant tissuedestruction (e.g. Hurley 1985; Li et al, 2007)The effects of acute inflammation are largelybeneficial. The fluid exudate dilutes the toxins andescaped blood products include antibodies (andsystemic drugs). The fibrinogen forms fibrin clotsproviding a mechanical barrier to the spread ofmicro-organisms (if present) and additionally assistsphagocytosis. The gel like consistency of theinflammatory exudate also makes a positivecontribution by preventing the spread of theinflammatory mediators to surrounding, intacttissues. Transportation of invading bacteria (ifpresent) to the lymphatic system stimulates animmune response whilst the increased blood flowcontributes to the increased cell metabolismnecessary for the proliferative stage by increasinglocal oxygen content, supply of necessary nutrientsand removal of waste products. The leucocytesprovide a mechanism for the phagocytosis of foreignmaterial, bacteria, dead cells, with the neutrophils(PMN's) and monocytes (becoming macrophages)making the greatest contribution.There are several detrimental aspects ofinflammation which deserve mention. Firstly theincreased local hydrostatic pressure from theoedema can restrict blood flow if the injured tissuespace is limited, produce pain and therefore limitfunction and additionally reduce local oxygen levels.There have been suggestions that free radicalsproduced as a result of acute inflammatory responsesmay have detrimental effects on cell membraneprocesses as may overproduction of lysosomalenzymes from PMN activity.There are many aspects of the inflammatory eventsthat can be influenced by therapeutic intervention,ranging from the mechanical to the biochemical.There is a growing body of evidence to support theeffects of manual and exercise therapy on the ‘soup’of chemical mediators, cytokines and growth factors.Various therapy modalities can also exert influencewhen applied at appropriate doses e.g. (there arehundreds of these papers - this is a mini selection):Soft Tissue Healing Review Tim Watson (2016)EXERCISE AND MECHANICAL STRESS Caltrioni et al (2008) – link between exerciseand plasma glycosaminoglycan levels Fujiwara et al (2005) - mechanical stress andbFGF Handschin and Spiegelman (2008) - exerciseand PGC1 Kahn and Scott (2009) - mechanical stress andIGF Kido et al (2009) - mechanical stress and IL-11expression Li et al (2004) Mechanical stretching andfibroblast behaviour Ostrowski et al (2000) – link between exerciseand Interleukin-6 (IL-6) production Palomares et al (2009) – link betweenmechanical loading, bone repair and variousmediators and cytokines Takao et al (2011) - mechanical stress and COX2, interleukin-1β, PGE2ULTRASOUND (LIPUS AND TRADITIONAL ) Khanna et al (2009) - LIPUS and a range ofcytokine actions reviewed Leung et al (2006) –ultrasound and TGF-β inknee ligament healing Li et al (2003) - LIPUS and various cytokines(TNF- and TGF-β1 and IL-6) McBrier et al (2007) - US and Mechano GrowthFactor (MGF) Nussbaum and Locke (2007) - US and HeatShock Proteins Rego et al (2010) - US and PGE2 synthesis Sugita et al (2008) - US and nitric oxide (NO)LASER Bjordal et al (2006) - laser therapy and alteredprostaglandin levels in the tissue (Achillestendon) dos Santos et al (2014) illustrating that capacityof laser to influence a range of inflammatorybiomarkers Marcos et al (2011) – links between lasertherapy, COX-2 and PGE2 expression Mesquita Ferrari et al (2011) - laser therapy,TNF- and TGF-β Pires et al (2011) – links between laser therapyand inflammatory mediators Safavi et al (2008) - laser and a range ofinflammatory cytokines Sawasaki et al (2009) - laser and mast celldegranulationPage 6
Saygun et al (2008) - laser therapy and bFGF andIGF-1OTHER THERAPIES Zhang et al (2004) – demonstrated link betweenelectroacupuncture and peripheral inflammatoryresponses Sakurai et al (2008) - magnetic fields andprostaglandin E2 secretion Zhang et al (2014) and Wang et al (2011) areamongst numerous studies illustrating therelationship between shockwave andinflammatory modulation effects.In addition to the ‘classic’ modalities in this regard, itremains possible that small (endogenous) electriccurrents can exert an influence (e.g. Watson, 2008).The application of microcurrent based therapies isthought to enhance this component of theinflammatory/repair sequence (reviewed in Poltawskiand Watson, 2009) and whilst most electricalstimulation modalities do not have a direct influenceon the tissue repair sequence, microcurrent basedtherapies do appear to be increasingly supported bythe research evidence in this regard.Proliferative EventsPROLIFERATIONCytokine Based Drivers from Inflammatory EventsFibroblastsThe source of the majority of these cytokines is theinflammatory phase, thus 'turning off' or limiting theinflammatory events also reduces the signal strengthstimulating these proliferative events (e.g. Boursinoset al, 2009; Beck et al, 2005; Dimmen et al, 2009; Radiet al, 2005).Two fundamental processes involved in the repair arefibroplasia and angiogenesis (Figure 6). The functionof the fibroblast is to repair the connective tissue(Vanable 1989). Tim Watson (2016)EndothelialCellsProliferate and Increase Activity LevelsCollagen BasedScar TissueThe repair process restores tissue continuity by thedeposition of repair (scar) tissue. This is initiallygranulation tissue which matures to form scar tissue.Repair tissue is a connective tissue distinct right fromthe onset in several ways from the connective tissuenative to the site (Forrest 1983). Interesting recentdevelopments have identified that in muscle there isa degree of regenerative activity post trauma, linkedto the activation of a mechanosensitive growth factorand subsequent activation of muscle satellite (stem)cells (Hill et al 2003). A range of growth factors havebeen identified as being active in the processes ofproliferation, leading again to some new potentialtreatments (e.g. Hildebrand et al 1998).Soft Tissue Healing ReviewFibroblasts appear to migrate to the area fromsurrounding tissue. Fibroblastic activation appearsto be chemically mediated, particularly by chemicalsreleased from the macrophages during theinflammatory stage. Fibroblasts migrate into thedamaged area and proliferate within the first fewdays after the tissue damage. Macrophage DerivedGrowth Factors (MGDF's) are a complex group ofmediators responsible, at least in part for theactivation of isation)enhanced localcirculatory activityWoundContraction andEnhanced repairtissue StrengthFigure 6 : Key Proliferative elementsAlongside the fibroblastic activation, capillaries inthe region of the tissue damage bud and growtowards the repair zone. Loops and arcades areformed together with anastamoses which reestablish a blood flow through the region, providingoxygen and nutrients whilst removing metabolicand repair waste products. Oxygen is critical formany of the reparative processes, but especially forcollagen production (Vanables 1989, Niinikoski1980). A wide range of growth factors and chemicalmediators have been identified which exertinfluences on the developing capillaries. Theseinclude macrophage derived factors, PDGF, lacticacid and fibroblast growth factor (Vernon-Roberts1988). Some of these mediators are producedduring the inflammatory phase, thus making anessential link between the inflammatory andproliferative phases. Li et al (2005) provide a reviewPage 7
of the essential nature of the angiogenic events in therepair sequence. Numerous researchers (e.g. Oryanet al, 2012) have illustrated that the healing ratevaries between tissues - being slow for example inligament, which given its relatively poor vascularity isalmost predictable.There is growing evidence that various therapies areable to (positively) influence these proliferative andangiogenic events include :PHAGOCYTESPROCOLLAGENLACTIC CATION SPACING BETWEENFIBRILSProteoglycansMACROPHAGES Azuma et al (2001) demonstrate that LIPUSinfluences angiogenesis in relation to fracturehealing.Reher et al (2002) demonstrate influence ofultrasound in relation to NO and PGE2production.Zhao et al (2004) demonstrate link betweenelectrical stimulation and angiogenicenhancement by means of VEGF mediatedresponse.Fitzsimmons et al (2008) demonstrate linkbetween pulsed electric fields, chondrocyteactivity and nitric oxide pathways .Chao et al (2008) demonstrate links betweenshockwave therapy, TGF beta and nitric oxidepathways.Rego et al (2010) ultrasound stimulation ofprostaglandin (PGE2) synthesis.Cheung et al (2011) ultrasound (LIPUS) andangiogenesis in osteoporotic fracturesKuo et al (2009) shockwave therapy increasesseveral cytokines including VEGF in a woundhealing modelBossini et al (2009) demonstrate the influence oflaser therapy on the angiogenic events in woundrepairLu et al (2008) ultrasound (LIPUS) and VEGFregulation in fracture healingGranulation tissue invasion follows the 'demolition'phase (when autolytic enzymes are released fromPMN's and dead cells) (Walter and Israel 1987). Theactivation of fibroblasts and capillary budding wouldnormally occur by about the third day after the tissueinsult. The combination of capillary budding andcollagen production results in a more vascular thanusual repair site. The fibroblasts initially producepredominantly type III collagen which will becometype I collagen as the repair matures – duringremodelling (Walter and Israel 1987).Soft Tissue Healing Review Tim Watson (2016)REPRESENTATION OF FIBROBLAST / COLLAGEN PRODUCTION PATHWAYFigure 7 : Fibroblast activity during proliferationFibroblasts also produce fibronectins andproteoglycans which are essential components ofthe ground substance (Figure 7) (Walter and Israel1987, Forrest 1983, Hardy 1989).Myofibroblasts are derived from fibroblastsactivated by a variety o
normal time for bleeding to stop will vary with the nature of the injury and the nature of the tissue in question. The more vascular tissues (e.g. muscle) will bleed for longer and there will be a greater escape of blood into the tissues. Other tissues (e.g. ligament) will bleed less (both in terms of duration and volume).