Transcription
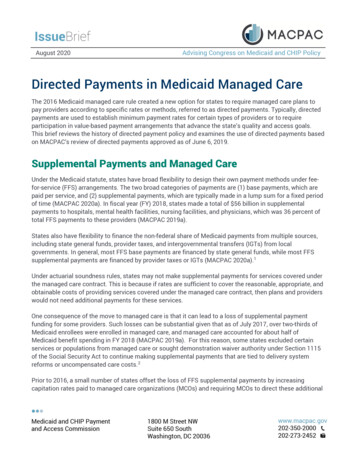
MEDICAID MANAGED CARE/FAMILY HEALTH PLUS/HIV SPECIAL NEEDS PLAN/HEALTH AND RECOVERY PLANMODEL CONTRACTMarch 1, 2019
MISCELLANEOUS/CONSULTANT SERVICES(Award Without Formal Request For Proposal)STATE AGENCY (Name and Address):New York State Department of HealthOffice of Health Insurance ProgramsDivision of Health Plan Contracting andOversightOne Commerce PlazaRoom 1609Albany, NY 12260CONTRACTOR (Name and Address):NYS Comptroller’s Number:Originating Agency GLBU: DOH01Department ID: 3450000 (Use Unit ID)TYPE OF PROGRAM(S):Medicaid Managed Care and/orFamily Health Plus and/or HIV Special Needs PlanCHARITIES REGISTRATION NUMBER:Contractor has ( ) has not ( ) timely filed withthe Attorney General’s Charities Bureau allrequired period or annual written reports.CONTRACT TERM:FROM: March 1, 2019TO:February 29, 2024FEDERAL TAX IDENTIFICATION NUMBER:FUNDING AMOUNT FOR CONTRACT TERM:NYS VENDOR IDENTIFICATION NUMBER:MUNICIPALITY NUMBER (if applicable):STATUS:CONTRACTOR IS [ ] IS NOT [ ]A SECTARIAN ENTITYCONTRACTOR IS [ ] IS NOT [ ]A NOT-FOR-PROFIT ORGANIZATIONCONTRACTOR IS [ ] IS NOT [ ]A NY STATE BUSINESS ENTERPRISE( ) IF MARKED HERE, THIS CONTRACT ISRENEWABLE FOR ADDITIONAL ONEYEAR PERIOD(S) AT THE SOLE OPTION OFTHE STATE AND SUBJECT TO THEAPPROVAL OF THE NEW YORK STATEDEPARTMENT OF HEALTH, THE UNITEDSTATES DEPARTMENT OF HEALTH ANDHUMAN SERVICES AND THE OFFICE OF THESTATE COMPTROLLER.
APPENDICES TO THIS AGREEMENT ANDINCORPORATED BY REFERENCE INTO THE AGREEMENT-X-Appendix A. Standard Clauses for New York State Contracts-X-Appendix B. Certification Regarding Lobbying-X-Appendix B-1. Certification Regarding MacBride Fair Employment Principles-X-Appendix C. New York State Department of Health Requirements for the Provision of FamilyPlanning and Reproductive Health Services-X-Appendix D. New York State Department of Health MCO Outreach/Advertising Activities-X-Appendix E. New York State Department of Health Member Handbook Guidelines-X-Appendix F. New York State Department of Health Action and Grievance and Appeal SystemRequirements for the MMC and FHPlus Programs-X-Appendix G. New York State Department of Health Requirements for the Provision ofEmergency Care and Services-X-Appendix H. New York State Department of Health Requirements for the Processing ofEnrollments and Disenrollments in the MMC and FHPlus Programs-X-Appendix I. New York State Department of Health Guidelines for Use of Medical Residents andFellows-X-Appendix J. New York State Department of Health Guidelines for Contractor Compliance withthe Federal Americans with Disabilities Act-X-Appendix K. Prepaid Benefit Package Definitions of Covered and Non-Covered Services-X-Appendix L. Approved Capitation Payment Rates-X-Appendix M. Service Area and Benefit Package Options-X-Appendix N. RESERVED-X-Appendix O. Requirements for Proof of Workers’ Compensation and Disability BenefitsCoverage-X-Appendix P. Facilitated Enrollment and Federal Health Insurance Portability and AccountabilityAct (“HIPAA”) Business Associate Agreements-X-Appendix Q. New York State Department of Health Recipient Restriction ProgramRequirements for MMC and FHPlus Programs-X-Appendix R. Additional Specifications for the MMC and FHPlus Agreement-X-Appendix S. New York State Department of Health Requirements for Long Term Services andSupports for MMC and FHPlus Programs-X-Appendix T. Additional Requirements for the HARP and HIV SNP Programs-X-Appendix U. Intellectual/Developmental Disabilities (I/DD)Specialized I/DD Plan (SIP)-X-Appendix X. Modification Agreement Form
IN WITNESS WHEREOF, the parties hereto have executed or approved this AGREEMENT asof the dates appearing under their signatures.CONTRACTOR SIGNATURESTATE AGENCY SIGNATUREBy:By:Printed NamePrinted NameTitle:Title:Date:Date:State Agency Certification:In addition to the acceptance of this contract, Ialso certify that original copies of thissignature page will be attached to all otherexact copies of this contract.STATE OF NEW YORKCounty of)))SS.:On the day of in the year , before me, the undersigned,personally appeared , personally known to me orproved to me on the basis of satisfactory evidence to be the individual(s) whose names(s) is (are)subscribed to the within instrument and acknowledged to me that he/she/they executed the samein his/her/their/ capacity(ies), and that by his/her/their signature(s) on the instrument, theindividual(s), or the person upon behalf of which the individual(s) acted, executed theinstrument.(Notary)ATTORNEY GENERALThomas P. DiNapoliSTATE COMPTROLLERTitle:Title:Date:Date:
Table of Contents for Model ContractRecitalsSection 1DefinitionsSection 2Agreement Term, Amendments, Extensions, and General ContractAdministration e Agreement2.5Renegotiation2.6Assignment and Subcontracting2.7Terminationa.SDOH Initiated Terminationb.Contractor and SDOH Initiated Terminationc.Contractor Initiated Terminationd.Termination Due to Loss of Funding2.8Close-Out Procedures2.9Rights and Remedies2.10 Notices2.11 SeverabilitySection 3Compensation3.1Capitation Payments3.2Modification of Rates During Contract Period3.3Rate Setting Methodology3.4Payment of Capitation3.5Denial of Capitation Payments3.6SDOH Right to Recover Premiums3.7Third Party Health Insurance Determination3.8Other Insurance and Settlements3.9Payment for Newborns3.10 Supplemental Maternity Capitation Payment3.11 Contractor Financial Liability3.12 Inpatient Hospital Stop-Loss Insurance for Medicaid Managed Care(MMC) Enrollees3.13 Mental Health Stop-Loss for MMC Enrollees3.14 Residential Health Care Facility (Nursing Home) Stop-Loss for MMCEnrollees3.15 Stop-Loss Documentation and Procedures for the MMC Program3.16 Family Health Plus (FHPlus) Reinsurance3.17 Tracking Visits Provided by Indian Health Clinics – Applies to MMCProgram Only3.18 Payment for Patient Centered Medical Homes and Adirondack HealthCare Home Multipayor Demonstration Program3.19 Prohibition on Payments to Institutions or Entities Located Outside of theUnited StatesTABLE OF CONTENTSMarch 1, 20191
Table of Contents for Model Contract3.203.213.223.233.24Primary Care Rate IncreasePayment for Long Term Placement in Residential Health Care Facilities(Nursing Homes)Minimum Medical Expense Targets and Limits on Profit and LossConditions on Incentive ArrangementsMedical Loss RatioSection 4Service Area4.1Service Area4.2Modification of Service Area and Optional Benefit Package CoveredServices During Contract Period4.3Modification of Benefit Package ServicesSection 5ReservedSection 6Enrollment6.1Populations Eligible for Enrollment6.2Enrollment Requirements6.3Equality of Access to Enrollment6.4Enrollment Decisions6.5Auto Assignment – For MMC Program Only [Not Applicable to HIV SNPand HARP Programs]6.6Prohibition Against Conditions on Enrollment6.7Newborn Enrollment6.8Effective Date of Enrollment6.9Roster/834 File6.10 Re-Enrollment6.11 Verification of HIV SNP Enrollment Eligibility [Applicable to HIV SNPProgram Only]Section 7Lock-In Provisions7.1Lock-In Provisions in MMC Mandatory Counties and for Family HealthPlus7.2Disenrollment During a Lock-In Period7.3Notification Regarding Lock-In and End of Lock-In Period7.4Lock-In and Change in Eligibility Status7.5Lock-In Provisions for Children in Foster Care7.6Lock-In Provisions for Individuals in Long Term Placement in NursingHomesSection 8Disenrollment8.1Disenrollment Requirements8.2Disenrollment Prohibitions8.3Disenrollment Requestsa.Routine Disenrollment Requestsb.Non-Routine Disenrollment Requests8.4Contractor Notification of DisenrollmentsTABLE OF CONTENTSMarch 1, 20192
Table of Contents for Model Contract8.58.68.78.88.9Contractor’s LiabilityEnrollee Initiated DisenrollmentContractor Initiated DisenrollmentSDOH, Enrollment Broker, NYSoH, or LDSS Initiated DisenrollmentPassive Reassignment of Enrollees in Receipt of MedicareSection 9RESERVEDSection 10Benefit Package Requirements10.1 Contractor Responsibilities10.2 Compliance with State Medicaid Plan, Applicable Laws and Regulations10.3 Definitions10.4 Child Teen Health Program/Adolescent Preventive Services10.5 Foster Care Children – Applies to MMC Program Only10.6 Child Protective Services10.7 Welfare Reform – Applies to MMC Program Only10.8 Adult Protective Services10.9 Court-Ordered Services10.10 Family Planning and Reproductive Health Services10.11 Prenatal Care and Elective Deliveries Less Than 39 Weeks Gestation10.12 Direct Access10.13 Emergency Services10.14 Reserved10.15 Services for Which Enrollees Can Self-Refera.Mental Health and Chemical Dependence Servicesb.Vision Servicesc.Diagnosis and Treatment of Tuberculosisd.Family Planning and Reproductive Health Servicese.Article 28 Clinics Operated by Academic Dental Centers10.16 Second Opinions for Medical or Surgical Care10.17 Contractor Responsibilities Related to Public Health10.18 Public Health Servicesa.Tuberculosis Screening, Diagnosis and Treatment; DirectlyObserved Therapy (TB/DOT)b.Immunizationsc.Prevention and Treatment of Sexually Transmitted Diseasesd.Lead Poisoning – Applies to MMC Program Onlye.Lead Poisoning – Applies to FHPlus Program Onlyf.Matching to Immunization and Lead Data Filesg.New York City Only10.19 Adults with Chronic Illnesses and Physical or Developmental Disabilities10.20 Children with Special Health Care Needs10.21 Mental Health Services10.22 Member Needs Relating to HIV10.23 Substance Use Disorder Services10.24 Native Americans10.25 Women, Infants, and Children (WIC)TABLE OF CONTENTSMarch 1, 20193
Table of Contents for Model Contract10.26 Urgently Needed Services10.27 Dental Services Provided by Article 28 Clinics Operated by AcademicDental Centers Not Participating in Contractor’s Network- Applies toMMC Program Only10.28 Optometry Services Provided by Article 28 Clinics Affiliated with theCollege of Optometry of the State University of New York10.29 Hospice Services10.30 Prospective Benefit Package Change for Retroactive SSI Determinations –Applies to MMC Program Only10.31 Coordination of Services10.32 Pharmacy Services10.33 Personal Care Services10.34 Additional Requirements for the HIV SNP Program Only10.35 Person Centered Services Plan10.36 Consumer Directed Personal Assistance Services (CDPAS) – MMCProgram Only10.37 Discharge Planning10.38 Critical Incidents10.39 Adult Day Health Care (ADHC) and AIDS Adult Day Health Care (AIDSADHC)10.40 Residential Health Care Facility (Nursing Home) Benefit for Long TermPlacement10.41 Care Coordination for the HARP Program and HARP-Eligible Enrolleesin the HIV SNP Program [Applicable to the HARP and HIV SNPPrograms]10.42 Behavioral Health Home and Community Based Services [Applicable tothe HARP and HIV SNP Programs]10.43 Cost-Effective Alternative Services10.44 Settings for Home and Community Based ServicesSection 11Outreach/Advertising11.1 Media11.2 Prior Approval of Advertising Materials and Procedures11.3 Restricted Activities and Remedial ActionsSection 12Member Services12.1 General Functions12.2 Translation and Oral Interpretation12.3 Communicating with the Visually, Hearing and Cognitively ImpairedSection 13Enrollee Rights and Notification13.1 Information Requirements13.2 Provider Directories/Office Hours for Participating Providers13.3 Member ID Cards13.4 Member Handbooks13.5 Notification of Effective Date of Enrollment13.6 Notification of Enrollee RightsTABLE OF CONTENTSMarch 1, 20194
Table of Contents for Model Contract13.713.813.913.1013.11Enrollee’s RightsApproval of Written NoticesContractor’s Duty to Report Lack of ContactLDSS Notification of Enrollee’s Change in AddressContractor Responsibility to Notify Enrollee of Effective Date of BenefitPackage Change13.12 Contractor Responsibility to Notify Enrollee of Termination, Service AreaChanges and Network Changes13.13 Post-Enrollment Follow-Up [Applicable to HIV SNP Program Only]Section 14Action and Grievance and Appeal System14.1 General Requirements14.2 Actions14.3 Grievance and Appeal System14.4 Notification of Action and Grievance and Appeal System Procedures14.5 Complaint Investigations by SDOH, OMH, OASAS and the LDSSSection 15Access Requirements15.1 General Requirement15.2 Appointment Availability Standards15.3 Twenty-Four (24) Hour Access15.4 Appointment Waiting Times15.5 Travel Time Standards15.6 Service Continuationa.New Enrolleesb.Enrollees Whose Health Care Provider Leaves Network15.7 Standing Referrals15.8 Specialist as a Coordinator of Primary Care15.9 Specialty Care Centers15.10 Cultural and Linguistic Competence15.11 Language Interpreter Services for Enrollee Encounters15.12 Telehealth Health Care and Telepsychiatry ServicesSection 16Quality Assurance16.1 Internal Quality Assurance Program16.2 Standards of Care16.3 Incentivizing Enrollees to Complete a Health Goal16.4 Quality Management (QM) Committee [Applicable to HIV SNP ProgramOnly]16.5 Quality Management Plan (QMP) [Applicable to HIV SNP Program Only]16.6 Quality Management (QM) Procedures [Applicable to HIV SNP ProgramOnly]16.7 HIV SNP Medical Director Requirements [Applicable to HIV SNPProgram Only]16.8 HIV Education for Staff [Applicable to HIV SNP Program Only]16.9 Quality Management (QM) and Provider Manuals [Applicable to HIVSNP Program Only]TABLE OF CONTENTSMarch 1, 20195
Table of Contents for Model Contract16.10 Quality Management (QM) Committee [Applicable to the HARP ProgramOnly]16.11 HARP Quality Management Plan (QMP) [Applicable to the HARPProgram Only]16.12 Quality Management (QM) Procedures [Applicable to the HARP ProgramOnly]16.13 Behavioral Health Clinical and Medical Directors Requirements16.14 HARP Behavioral Health Education for Staff [Applicable to the HARPand HIV SNP Programs]16.15 Quality Management (QM) and Provider Manuals [Applicable to theHARP Program Only]Section 17Monitoring and Evaluation17.1 Right To Monitor Contractor Performance17.2 Cooperation During Monitoring And Evaluation17.3 Cooperation During On-Site Reviews17.4 Cooperation During Review of Services by External Review AgencySection 18Contractor Reporting Requirements18.1 General Requirements18.2 Time Frames for Report Submissions18.3 SDOH Instructions for Report Submissions18.4 Notification of Changes in Report Due Dates, Requirements or Formats18.5 Reporting Requirements18.6 Ownership and Related Information Disclosure18.7 Public Access to Reports18.8 Professional Discipline18.9 Certification Regarding Prohibited Affiliations and Individuals Who HaveBeen Debarred or Suspended by Federal or State Government18.10 Conflict of Interest and Business Transaction Disclosure18.11 Physician Incentive Plan Reporting18.12 Disclosure of Criminal ActivitySection 19Records Maintenance and Audit Rights19.1 Maintenance of Contractor Performance Records, Records EvidencingEnrollment Fraud and Documentation Concerning Multiple CINs19.2 Maintenance of Financial Records and Statistical Data19.3 Access to Contractor Records19.4 Retention Periods19.5 OMIG’s Right to Audit and Recover Overpayments Caused by ContractorSubmission of Misstated Reports19.6 OMIG’s Right to Audit and Recover Overpayments Caused byContractor’s Misstated Encounter Data19.7 OMIG Audit Authority19.8 OMIG Compliance Review Authority19.9 Notification of AuditTABLE OF CONTENTSMarch 1, 20196
Table of Contents for Model ContractSection 20Confidentiality20.1 Confidentiality of Identifying Information about Enrollees, PotentialEnrollees, and Prospective Enrollees20.2 Medical Records of Foster Children20.3 Confidentiality of Medical Records20.4 Length of Confidentiality RequirementsSection 21Provider Network21.1 Network Requirements21.2 Absence of Appropriate or Available Network Provider21.3 Suspension of Enrollee Assignments to Providers21.4 Credentialing21.5 Exclusion or Termination of Providers21.6 Application Procedure21.7 Evaluation Information21.8 Choice/Assignment of Primary Care Providers (PCPs)21.9 Enrollee PCP Changes21.10 Provider Status Changes21.11 PCP Responsibilities21.12 Member to Provider Ratios21.13 Minimum PCP Office Hoursa.General Requirementsb.Waiver of Minimum Hours21.14 Primary Care Practitionersa.General Limitationsb.Specialists and Sub-specialists as PCPsc.OB/GYN Providers as PCPsd.Certified Nurse Practitioners as PCPse.Behavioral Health Clinicsf.Requirements Applicable to HIV SNP Program Only21.15 PCP Teamsa.General Requirementsb.Registered Physician Assistants as Physician Extendersc.Medical Residents and Fellows21.16 Hospitalsa.Tertiary Servicesb.Emergency Services21.17 Dental Networks21.18 Presumptive Eligibility Providers21.19 Behavioral Health Services Providers21.20 Laboratory Procedures21.21 Federally Qualified Health Centers (FQHCs)21.22 Provider Services Function21.23 Selective Contracting for Breast Cancer Surgery21.24 Patient Centered Medical Home21.25 Pharmacies21.26 Communication with PatientsTABLE OF CONTENTSMarch 1, 20197
Table of Contents for Model Contract21.2721.2821.2921.3021.3121.3221.33Health HomeCase Management Providers [Applicable to HIV SNP Program Only]Linkage Agreement Providers[Applicable to HIV SNP Program Only]Primary Care Rate IncreaseHospice ProvidersVeterans’ HomesIndian Health Care ProvidersSection 22Subcontracts and Provider Agreements22.1 Written Subcontracts22.2 Permissible Subcontracts22.3 Provision of Services Through Provider Agreements22.4 Approvals22.5 Required Components22.6 Timely Payment22.7 Recovery of Overpayments to Providers22.8 Restrictions on Disclosure22.9 Transfer of Liability22.10 Termination of Health Care Professional Agreements22.11 Health Care Professional Hearings22.12 Non-Renewal of Provider Agreements22.13 Notice of Participating Provider Termination22.14 Physician Incentive Plan22.15 Never Events22.16 Other Provider-Preventable Conditions22.17 Personal Care Services Worker Wage Parity Rules22.18 Value Based Payment ArrangementsSection 23Program Integrity23.1 Rights and Responsibilities23.2 Compliance Program23.3 Contractor Obligation to Return Overpayments23.4 Program Integrity Reporting Requirements23.5 Prevention Plans and Special Investigation Units23.6 Service Verification Process23.7 Withholding of Payments23.8 Shared Recovery Based on Referral23.9 Liquidated Damages for Failure to Report Recoveries23.10 State and Federal False Claims, Written Policies23.11 Contractor Obligation to Refer All Cases of Potential Fraud, Waste orAbuseSection 24Americans With Disabilities Act (ADA) Compliance PlanSection 25Fair Hearings25.1 Enrollee Access to Fair Hearing Process25.2 Enrollee Rights to a Fair HearingTABLE OF CONTENTSMarch 1, 20198
Table of Contents for Model Contract25.325.425.525.6Contractor Notice to EnrolleesAid ContinuingResponsibilities of SDOHContractor’s ObligationsSection 26External Appeal26.1 Basis for External Appeal26.2 Eligibility For External Appeal26.3 External Appeal Determination26.4 Compliance With External Appeal Laws and Regulations26.5 Member HandbookSection 27Intermediate Sanctions27.1 General27.2 Unacceptable Practices27.3 Intermediate Sanctions27.4 Enrollment Limitations27.5 Due ProcessSection 28Environmental ComplianceSection 29Energy ConservationSection 30Independent Capacity of ContractorSection 31No Third Party BeneficiariesSection 32Indemnification32.1 Indemnification by Contractor32.2 Indemnification by SDOHSection 33Prohibition on Use of Federal Funds for Lobbying33.1 Prohibition of Use of Federal Funds for Lobbying33.2 Disclosure Form to Report Lobbying33.3 Requirements of SubcontractorsSection 34Non-Discrimination34.1 Equal Access to Benefit Package34.2 Non-Discrimination34.3 Equal Employment Opportunity34.4 Native Americans Access to Services From Tribal or Urban Indian HealthFacilitySection 35Compliance with Applicable Laws35.1 Contractor and SDOH Compliance With Applicable Laws35.2 Nullification of Illegal, Unenforceable, Ineffective or Void ContractProvisionsTABLE OF CONTENTSMarch 1, 20199
Table of Contents for Model ificate of Authority RequirementsNotification of Changes in Certificate of IncorporationContractor’s Financial Solvency RequirementsCompliance With Care For Maternity PatientsInformed Consent Procedures for Hysterectomy and SterilizationNon-Liability of Enrollees For Contractor’s DebtsSDOH Compliance With Conflict of Interest LawsCompliance With Public Health Law (PHL) Regarding External AppealsFair Labor Standards ActSection 36Standard Clauses for New York State ContractsSection 37Medicaid UpdateAPPENDICESA.Standard Clauses for New York State ContractsB.Certification Regarding LobbyingB-1.Certification Regarding MacBride Fair Employment PrinciplesC.New York State Department of Health Requirements for the Provision of FamilyPlanning and Reproductive Health ServicesD.New York State Department of Health MCO Outreach/Advertising ActivitiesE.New York State Department of Health Member Handbook GuidelinesF.New York State Department of Health Action and Grievance and Appeal SystemRequirements for the MMC and FHPlus ProgramsG.New York State Department of Health Requirements for the Provision of EmergencyCare and ServicesH.New York State Department of Health Requirements for the Processing of Enrollmentsand Disenrollments in the MMC and FHPlus ProgramsI.New York State Department of Health Guidelines for Use of Medical Residents andFellowsJ.New York State Department of Health Guidelines for Contractor Compliance with theFederal Americans with Disabilities ActK.Prepaid Benefit Package Definitions of Covered and Non-Covered ServicesL.Approved Capitation Payment RatesTABLE OF CONTENTSMarch 1, 201910
Table of Contents for Model ContractM.Service Area and Benefit Package OptionsN.RESERVEDO.Requirements for Proof of Workers’ Compensation and Disability Benefits CoverageP.Facilitated Enrollment and Federal Health Insurance Portability and Accountability Act(“HIPAA”) Business Associate AgreementsQ.New York State Department of Health Recipient Restriction Program Requirements forMMC and FHPlus ProgramsR.Additional Specifications for the MMC and FHPlus AgreementS.New York State Department of Health Requirements for Long Term Services andSupports for MMC and FHPlus ProgramsT.Additional Requirements for the HARP and HIV SNP ProgramsU.Intellectual/Developmental Disabilities (I/DD)Specialized I/DD Plan (SIP)X.Modification Agreement FormTABLE OF CONTENTSMarch 1, 201911
STATE OF NEW YORKMEDICAID AND FAMILY HEALTH PLUSPARTICIPATING MANAGED CARE PLAN AGREEMENTThis AGREEMENT is hereby made by and between the New York State Department of Health(SDOH) and (Contractor) as identified on the face page ofthis Agreement.RECITALSWHEREAS, pursuant to Title XIX of the Federal Social Security Act, codified as 42U.S.C. Section 1396 et seq. (the Social Security Act), and Title 11 of Article 5 of the New YorkState Social Services Law (SSL), a comprehensive program of medical assistance for needypersons exists in the State of New York (Medicaid); andWHEREAS, pursuant to Title 11 of Article 5 of the SSL, the Commissioner of Health hasestablished a managed care program under the medical assistance program, known as theMedicaid Managed Care (MMC) Program; andWHEREAS, pursuant to Article 44 of the Public Health Law (PHL), the New York StateDepartment of Health (SDOH) is authorized to issue Certificates of Authority to establish HealthMaintenance Organizations (HMOs), PHL Section 4400 et seq., Prepaid Health Services Plans,(PHSPs), PHL Section 4403-a, and HIV Special Needs Plans (HIV SNPs), PHL Section 4403-c,and, jointly with the Commissioners of the Office of Mental Health (OMH) and the Office ofAlcoholism and Substance Abuse Services (OASAS), for Health and Recovery Plans (HARPs),PHL Section 4403-d andWHEREAS, pursuant to Title 11-D of Article 5 of the SSL, a health insurance programknown as Family Health Plus (FHPlus) was created effective January 1, 2001 for eligiblepersons who do not qualify for Medicaid , and such Law was repealed effective January 1, 2015;andWHEREAS, organizations certified under Article 44 of the New York State PublicHealth Law (PHL) are eligible to provide comprehensive health services through comprehensivehealth services plans to Eligible Persons as defined in Titles 11 and 11-D of the SSL, MMC, HIVSNPs, HARP and FHPlus Programs, respectively; andWHEREAS, the Contractor is organized under the laws of New York State and iscertified under Article 44 of the PHL and has offered to provide covered health services toEligible Persons residing in the geographic area specified in Appendix M of this Agreement(Service Area and Benefit Package Options); andRECITALSMarch 1, 2019Page 1 of 2
WHEREAS, the SDOH has determined that the Contractor meets the qualificationsestablished for participation in the MMC Program, the HIV SNP Program, the FHPlus, and/orthe HARP Program to provide the applicable health care coverage to Eligible Persons in thegeographic area specified in Appendix M of this Agreement.NOW THEREFORE, the parties agree as follows:RECITALSMarch 1, 2019Page 2 of 2
1.DEFINITIONS“834 Electronic Data Interchange Transmission File (834 File)” means a HIPAA5010 compliant transaction enacted as part of the Affordable Care Act (P.L. 111-148 and111-152). The 834 is an electronic Benefit Enrollment and Maintenance documentgenerated by the New York State of Health. The 834 File contains new enrollments,changes in enrollments, reinstatement of enrollments and disenrollments.“Abuse” means practices that are inconsistent with sound fiscal, business, medical orprofessional practices, and which result in unnecessary costs to the Medicaid program,payments for services that were not medically necessary, or payments for services whichfail to meet recognized standards for health care. It also includes enrollee practices thatresult in unnecessary costs to the Medicaid program.“Advance Directive” means a written instruction recognized under State law, whetherstatutory or as recognized by the courts of the State, relating to the provision of healthcare when the individual is incapacitated.“Aliessa” means a non-citizen under 65 years of age who entered the United States on orafter August 22, 1996 and is lawfully residing in New York State, who would otherwisebe ineligible for Medicaid solely due to his or her immigration status.“Auto-assignment” means a process by which an MMC Eligible Person, as this term isdefined in this Agreement, who is mandated to enroll in the MMC Program, but who hasnot selected and enrolled in an MCO within sixty (60) days of receipt of the mandatorynotice sent by the LDSS, is assigned to an MCO offering a MMC product in the MMCEligible Person’s county of fiscal responsibility in accordance with the auto-assignmentalgorithm determined by the SDOH.“Behavioral Health” means mental health and/or substance use disorders.“Behavioral Health Benefit Inclusion” means the date, as determined by the State, theContractor is responsible for the provision of the expanded behavioral health BenefitPackage services, pursuant to the New York State Section 1115 Behavioral HealthPartnership Plan Waiver Amendment, for Enrollees 21 years of age and older residing ina specified county within the Contractor’s Service Area or the date the State determinesthe Contractor may begin accepting Enrollees in their HARP line of business."Behavioral Health Home and Community-Based Services (BHHCBS)" meansservices as set forth in Appendix T of this Agreement that are provided to individualsenrolled in a HARP or HIV SNP who have been determined to be eligible for suchservices pursuant to this Agreement.“Behavioral Health Provider” means a provider of mental health services licensedunder Article 31 of the Mental Hygiene Law, a provider of substance use servicescertified under Article 32 of the Mental Hygiene Law and a New York State-designatedSECTION 1(DEFINITIONS)March 1, 20191-1
provider of Behavioral Health Home and Community Based Services. For the purposesof this Agreement, individual practitioners are not considered Behavioral HealthProviders except where specifically indicated.“Behavioral Health Services” means services to address mental health disorders and/orsubstance use disorders, including Behavioral Health Home and Community BasedServices.“Benefit Package” means the covered services for the MMC and/or FHPlus Programs,described in Appendix K of this Agreement, to be provided to the Enrollee, as Enrollee isdefined in this Agreement, by or through the Contractor, including optional BenefitPackage services, if any, as specified in Appendix M of this Agreement.“Capitation Rate” means the fixed monthly amount that the Contractor receives for anEnrollee to provide that Enrollee with the Benefit Package.“Chemical Dependence Services” means examination, diagnosis, level of caredetermination, treatment, rehabilitation, or habilitation of persons suffering fromchemical abuse or dependence, and includes the provision of alcohol and/or substanceabuse services.“Child/Teen Health Program” or “C/THP” means the program of early and periodicscreening, including inter-periodic, diagnostic and treatment services (EPSDT) that NewYork State offers all Eligible Persons under twenty-one (21) years of age. Care andservices are provided in accordance with the periodicity schedule and guidelinesdeveloped by the New York State Department of Health. The services includeadministrative services designed to help families obtain services for children includingoutreach, information, appointment scheduling, administrative case management andtransportation assistance, to the extent that transportation is included in the BenefitPackage.“Clinical Advisory Groups (CAGs)” means groups that are composed of individualswith clinical or industry experience and knowledge of specific care or conditions. TheCAGs review clinical and episodic bundles, subpopulations and outcome measures thatare relevant to
10.27 Dental Services Provided by Article 28 Clinics Operated by Academic Dental Centers Not Participating in Contractor's Network- Applies to MMC Program Only 10.28 Optometry Services Provided by Article 28 Clinics Affiliated with the College of Optometry of the State University of New York 10.29 Hospice Services