![OASIS-D Handouts [Read-Only] - Missouri](/img/30/oasis-d-powerpoint-2-slides.jpg)
Transcription
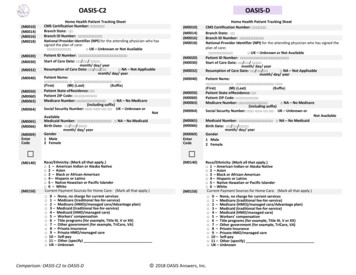
11/06/2018OASIS-D UpdatePresented by:Suzi Hamlet RN, MSN, COS-C, OASIS Educational CoordinatorRobin Swarnes RN, BSN, COS-C1OASIS-D UpdateLEARNING OBJECTIVES Identify the changes to Outcome and Assessment Information Set(OASIS) resulting from the Improving Medicare Post-Acute CareTransformation (IMPACT) Act of 2014 Describe the major changes from OASIS-C2 to OASIS-D Understand OASIS M-item coding instructions to accurately code newand revised OASIS items Identify available resources for implementing OASIS-D21
11/06/2018Why OASIS-D?IMPACT ACT OF 2014 Improving Medicare Post-Acute Care Transformation Act of 2014 Bipartisan bill signed into law by President Obama October 6, 2014 Requires Post-Acute Care (PAC) providers to report standardized patientassessment data and quality measure data Long Term Care Hospitals (LTCH)Skilled Nursing Facilities (SNF)Inpatient Rehabilitative Facility (IRF)Home Health Agencies (HHA)Hospices PAC Medicare spending 73.8 Billion.3IMPACT ACT of 2014 Driving ForcesPURPOSE: Improve Medicare beneficiary outcomes Provide access to longitudinal data to facilitatecoordinated care Enable comparable data and quality across PACsettings Improve hospital discharge planning ResearchPost AcuteCare?Why the attention on Post-Acute Care? Escalating cost associated with PAC Lack of data standards across PAC Goal of establishing payment rates according tothe individual characteristics of the patient, notthe care setting42
11/06/2018Why Standardization in PAC?Inpatient RehabFacilitiesSkilled NursingFacilitiesHome HealthAgenciesLong Term Eating5Why Standardization in PAC?Inpatient RehabFacilitiesSkilled NursingFacilitiesHome HealthAgenciesLong Term Eating63
11/06/2018Standardized Patient Assessment DataElements (SPADEs)SPADEs: Questions and response options that are identical inall four PAC assessment instruments Identical standards and definitions applyOASISIRFPAILCDS The move toward standardized assessment dataelements facilitates cross-setting data collection,quality measurement, outcome comparison, andinteroperable data exchangeMDS7Why is OASIS Being Updated Now?IMPACT Act/StandardizationNew StandardizedItems Section J: J1800& J1900 Section GG:GG0100,GG0110,GG0130, &GG0170Cross-SettingAlignmentAlignment incontent of itemsthat support crosssetting measures Drug RegimenReview Pressure Ulcers Active Diagnosis Height & WeightStandardized DataCollectionUpdates andCorrectionsReduction ofburden Quality measurechanges Survey andcertificationGeneral updatesCorrections madeas necessary84
11/06/2018 New items are added Different time point versions of some items Removal of items Revision of some items Updated Skip Patterns9 Chapter 3, two new sections of standard guidance added: Section J – Health Conditions Section GG – Functional Abilities and Goals Chapter 4, Illustrative Examples are retired Removal of many items and their corresponding guidance Revisions to existing Guidance for some OASIS items to update or clarifyinformation Appendix F - sample reports are not included in this version. Users mayrefer to the Casper Reporting User Manual, Section 6, OASIS QualityImprovement Reports, located at: https://qtso.cms.gov/hhatrain.html105
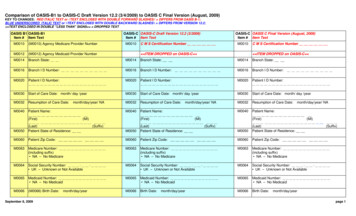
11/06/2018OASIS-D Guidance Manual ChangesGuidanceManualChanges for33 ItemsM0080, M0090, M0102, M1021, M1023, M1046,M1056, M1060, M1307, M1332, M1334, M1342,M1610, M1730, M1800, M1810, M1820, M1830,M1840, M1845, M1850, M1860, M1870, M1910,M2001, M2003, M2005, M2010, M2016, M2020,M2030, M2301, M2401For these 33 items, the Guidance Manual has been updated in oneor more of the following sections: Item Intent Time Points Collected Response Specific Instructions Examples Data Sources and ResourcesOASIS-D ChangesEffective January 1, 201911OASIS-D New ItemsSection J: Health Conditions (Falls) J1800: Any Falls Since SOC/ROC J1900: Number of Falls Since SOC/ROCSection GG: Functional Abilities and Goals GG0100: Prior Functioning: Everyday ActivitiesGG0110: Prior Device UseGG0130: Self-CareGG0170: Mobility126
11/06/2018OASIS-D Revised ItemsM1028Active DiagnosesM1306Unhealed Pressure Ulcer/Injury at Stage 2 or Higher?M1311Current Number of Unhealed Pressure Ulcers/Injuries at Each StageM1322Current Number of Stage 1 Pressure InjuriesM1324Stage of Most Problematic Unhealed Pressure Ulcer/Injury that is StageableM2102Types and Sources of AssistanceM2310Reason for Emergent Care13OASIS-D Revised ItemsThe 7 revised assessment items may have changes in one or more ofthe following areas:Time pointversionsItem textResponseoption(s)Use of theDASH (-) as avalid responseSkip patterns147
11/06/2018Skip Pattern ChangesM1000Go To M1021 (M1017 item removed)M1051M1501 and M1230 items removed, New Go To PatternM1306SOC/ROC/F-up Go To M1322, Discharge Go To M1324M1311New Time Point Versions, with specific Go To PatternsM1340M1350 item removed, New Go To PatternM1610M1615 and M1620 items removed, No Go To Pattern neededM2001M2040 item removed, New Go To PatternM2410M2430 and M0906 items removed, No Go To Pattern neededM2420M2430 item removed, No Go To Pattern needed15OASIS Items Removed28 Items Removed M0903, M1011, M1017, M1018, M1025, M1034,M1036, M1210, M1220, M1230, M1240, M1300,M1302, M1313, M1320, M1350, M1410, M1510,M1511, M1615, M1750, M1880, M1890, M1900,M2040, M2110, M2250, M2430OASIS Items were removed if they were not used to support: HH QRP measures HH Prospective Payment System (PPS) Survey process for Medicare certification HH Value-Based Purchasing (VBP) demonstration measures Critical risk-adjustment factors Conditions of Participation168
11/06/2018Updated One Clinician Rule Although one clinician must take responsibility for the comprehensive assessment,collaboration with the patient, caregivers, and other health care personnel, including thephysician, pharmacist, and/or other agency staff is appropriate. For items requiring patientassessment, the collaborating healthcare providers must have had direct contact with thepatient. Agencies may have the comprehensive assessment completed by one clinician. Ifcollaboration with other health care personnel and/or agency staff is utilized, the agency isresponsible for establishing policies and practices related to collaborative efforts, includinghow assessment information from multiple clinicians will be documented within the clinicalrecord, ensuring compliance with applicable requirements, and accepted standards ofpractice. When collaboration is utilized, the M0090 Date assessment completed should reflect thelast date the assessing clinician gathered or received any input used to complete thecomprehensive assessment, including the OASIS items. When used, collaboration must occur within the appropriate timeframe and consistent withdata collection guidance. Any exception to this general convention concerning collaborationis identified in item-specific guidance.17Comprehensive Assessment Completion At the start of care time point, the comprehensive assessment should becompleted within five days after the start of care date. At the resumption of care, the comprehensive assessment must becompleted within 48 hours of return home after inpatient facilitydischarge, or within 48 hours of knowledge of a qualifying stay in aninpatient facility. A physician-ordered resumption of care (ROC) visit must be conducted onthe physician-ordered ROC date. For the transfer to inpatient facility, discharge from home care, death athome, and other follow-up, the assessments must be completed on, orwithin 48 hours of becoming aware of the significant change in condition,transfer, discharge, or death date.189
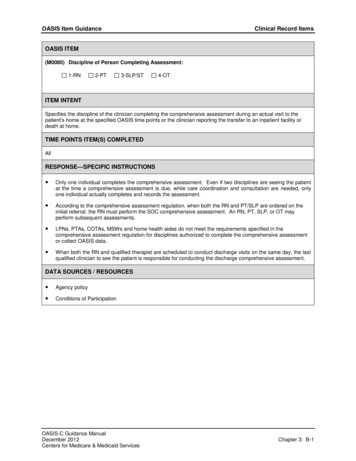
11/06/2018M0080 Discipline of PersonConducting Assessment(M0080) Discipline of Person Completing AssessmentEnter Code1.2.3.4.RNPTSLP/STOTITEM INTENTSpecifies the discipline of the cliniciancompleting the comprehensive assessmentduring an actual visit to the patient’s home atthe specified OASIS time point or the clinicianreporting the transfer to an inpatient facility ordeath at home.Response Specific Instructions While only the assessing clinicianis responsible for accuratelycompleting and signing acomprehensive assessment,he/she may collaborate to collectdata for all OASIS items, if agencypolicy allows.TIME POINTS ITEM(S) COMPLETED All19M0090 Date Assessment Completed(M0090) Date Assessment Completed/month/dayyearITEM INTENT Specifies the actual date the assessment is completed.TIME POINTS ITEM(S) COMPLETED All2010
11/06/2018M0102 Date of Physician-orderedStart of Care (Resumption of Care)(M0102) Date of Physician-ordered Start of Care (Resumption of Care): If the physician indicated a specific start of care (resumptionof care) date when the patient was referred form home health services, record the date specified./month/dayyearNA - No Specific SOC date ordered by physicianITEM INTENTSpecifies the date that home care services are ordered to begin or toresume following an inpatient stay of 24 hours or longer and forreasons other than diagnostic tests, if a SOC/ROC date was specifiedby the physician.The item refers to the order to start home care services (that is,provide the first covered service), or resume home care services (thatis provide the first visit following a qualifying inpatient stay) regardlessof the type of services ordered (for example, therapy only).TIME POINTS ITEM COMPLETED Start of care Resumption of care21M1000 Which of the following Inpatient Facilitieswas Patient Discharged within past 14 Days?(M1000) From which of the following Inpatient Facilities was the patient discharged within thepast 14 days? (Mark all that apply.)1 - Long-term nursing facility (NF)2 - Skilled nursing facility (SNF/TCU)3 - Short-stay acute hospital (IPPS)4 - Long-term care hospital (LTCH)5 - Inpatient rehabilitation hospital or unit (IRF)6 - Psychiatric hospital or unit7 - Other (specify)NA - Patient was not discharged from an inpatient facility [Go to M1021]2211
11/06/2018RESPONSE SPECIFICINSTRUCTIONSM1021 Primary Diagnosis /M1023 Other Diagnoses The assessing clinician is expected to complete the patient’scomprehensive assessment and understand the patient’s overall medicalcondition and care needs before selecting and assigning diagnoses andmay elicit input from other agency staff that have had direct in-personcontact with the patient, or have had some other means of gatheringinformation to contribute to the OASIS data collection.23Revised ItemM1028 Active Diagnoses(M1028) Active Diagnoses – Comorbidities and Co-existing Conditions – Check all that applySee OASIS Guidance Manual for a complete list of relevant ICD-10 codes.1 - Peripheral Vascular Disease (PVD) or Peripheral Arterial Disease (PAD)2 - Diabetes Mellitus (DM)3 - None of the aboveITEM INTENTThis item identifies whether two specificdiagnoses are present and active. Thesediagnoses influence a patient’s functionaloutcomes or increase a patient’s risk fordevelopment or worsening of pressureulcer(s).TIME POINTS ITEM(S) COMPLETED Start of care Resumption of care2412
11/06/2018CODING INSTRUCTIONSM1028 Active DiagnosesA DASH is avalid responsefor this item. Code 1, Peripheral Vascular Disease (PVD) or Peripheral ArterialDisease (PAD), if the patient has an active diagnosis of PeripheralVascular Disease (PVD) or Peripheral Arterial Disease (PAD). Code 2, Diabetes Mellitus (DM), if the patient has an active diagnosisof Diabetes Mellitus (DM) indicated by any of the following diagnosiscodes: Code 3, None of the Above, if the patient does not have any of theactive diagnoses listed above.25CODING TIPSM1028 Active Diagnoses The physician (nurse practitioner, physician assistant, clinical nursespecialist, or other authorized licensed staff if allowable under statelicensure laws) may specifically indicate that a diagnosis is active. If there is documentation in the clinical record that a patient hasdiabetes mellitus, Select Response 2, Diabetes Mellitus (DM). If there is only documentation in the clinical record of a complicationsuch as nephropathy or neuropathy and there is no documentationthat the patient has diabetes, it should not be assumed thecomplication is associated with diabetes, and Response 2, DiabetesMellitus, should not be checked.2613
11/06/2018M1028 Active DiagnosesEXAMPLE 1 Mr. A is prescribed insulin for diabetes mellitus. He requires regular blood glucose monitoring to determine whether blood glucose goalsare achieved by the current medication regimen. The physician progress note documents diabetes mellitus.(M1028) Active Diagnoses – Comorbidities and Co-existing Conditions – Check all that applySee OASIS Guidance Manual for a complete list of relevant ICD-10 codes.1 - Peripheral Vascular Disease (PVD) or Peripheral Arterial Disease (PAD)2 - Diabetes Mellitus (DM)3 - None of the above27M1028 Active DiagnosesEXAMPLE 2 During the SOC/ROC assessment, Mrs. K told Nurse J, RN that she has had diabetesfor 20 years. Nurse J reviewed the transfer documents from the acute care facility and all clinicalrecords on the patient but was unable find a documented diagnosis of DiabetesMellitus by physician, nurse practitioner, physician assistant or authorized licensedstaff member in their state. There is no documented diagnosis of PVD or PAD.(M1028) Active Diagnoses – Comorbidities and Co-existing Conditions – Check all that applySee OASIS Guidance Manual for a complete list of relevant ICD-10 codes.1 - Peripheral Vascular Disease (PVD) or Peripheral Arterial Disease (PAD)2 - Diabetes Mellitus (DM)3 - None of the above2814
11/06/2018M1046 Influenza Vaccine Received, andM1056 Reason Pneumococcal Vaccine not receivedRESPONSE-SPECIFIC INSTRUCTIONS for M1046: Enter Response 5 if the influenza vaccine is contraindicated for medical reasons. Refer to the Centers for Disease Control and Prevention (CDC) website forinformation on contraindications for the influenza vaccine (See link in Chapter 5).RESPONSE-SPECIFIC INSTRUCTIONS for M1056: Enter Response 2 if pneumococcal vaccine administration is contraindicated forthis patient. Refer to the Centers for Disease Control and Prevention (CDC) website forinformation on contraindications for the pneumococcal vaccine (See link inChapter 5).29M1051 Pneumococcal Vaccine(M1051) Pneumococcal Vaccine: Has the patient ever received the pneumococcal vaccination(for example, pneumovax)?Enter Code1. No2. Yes [Go to M2005 at TRN, Go to M1242 at DC]3015
11/06/2018M1060 Height and Weight(M1060) Height and Weight – While measuring, if the number is X.1-X.4 round down; X.5 or greaterround upinchespoundsa. Height (in inches). Record most recent height measure since the most recentSOC/ROCb. Weight (in pounds). Base weight on most recent measure in last 30 days; measureweight consistently, according to standard agency practice (for example, in a.m.after voiding, before meal, with shoes off, etc.ITEM INTENT These items support calculation of the patient’s body mass index (BMI) using the patient’s heightand weight.TIME POINTS ITEM(S) COMPLETED Start of care Resumption of care31CODING INSTRUCTIONSHEIGHTM1060 Height and Weight Measure height in accordance with the agency’s policies and procedures. Measure and record the patient’s height to the nearest whole inch. Use mathematical rounding (i.e., if height measurement is X.5 inches or greater, roundheight upward to the nearest whole inch. If height measurement number is X.1 to X.4inches, round down to the nearest whole inch). For example, a height of 62.5 inches wouldbe rounded to 63 inches, and a height of 62.4 inches would be rounded to 62 inches. Only enter a height that has been directly measured by agency staff. Donot enter a height that is self-reported or derived from documentationfrom another provider setting.3216
11/06/2018CODING INSTRUCTIONSWEIGHTM1060 Height and Weight Weight should be measured in accordance with the agency’s policies and procedures. Measure and record the patient’s weight in pounds. Use mathematical rounding (e.g., if weight is X.5 pounds [lbs.] or more, roundweight upward to the nearest whole pound. If weight is X.1 to X.4 lbs., round downto the nearest whole pound). For example, a weight of 152.5 lbs. would be roundedto 153 lbs. and a weight of 152.4 lbs. would be rounded to 152 lbs. If agency staff weighs the patient multiple times during the assessment period, usethe first weight. Only enter a weight that has been directly measured by agency staff. Do notenter a weight that is self-reported or derived from documentation fromanother provider setting.33CODING TIPSM1060 Height and WeightA DASH is a validresponse for thisitem. When reporting height for a patient with bilateral lower extremityamputation, measure and record the patient’s current height (i.e., heightafter bilateral amputation). If a patient cannot be weighed, for example, because of extreme pain,immobility, or risk of pathological fractures, the use of a dash ( – ) isappropriate. Document the rationale on the patient’s medical record. When there is an unsuccessful attempt to measure a patient’s height orweight, at SOC/ROC, and there is a documented agency-obtained height orweight from one or more previous home health visits, an agency-obtainedheight or weight from a documented visit conducted within the previous30-day window may be used to complete M1060 for this SOC/ROCassessment. Whenever possible, a current height and weight should be obtained by theagency as part of the SOC/ROC assessment.3417
11/06/2018Pressure Ulcer / Injury ReviewDeleted ItemsM1300 & M1302Pressure Ulcer RiskM1313Worsening of PressureUlcer StatusM1320Status of MostProblematic Pressure UlcerM1350Other Skin LesionsRemaining ItemsM1306Unhealed Pressure Ulcer/Injury atStage 2 of Higher or UnstageableM1307Oldest Stage 2 Pressure UlcerM1311Current Number Unhealed PressureUlcers/Injuries at Each StageM1322Current Number of Stage 1 PressureInjuriesM1324Most Problematic PressureUlcer/Injury Stage35Pressure Ulcer / Injury TerminologyStage 1Now called Pressure InjuryStage 2,3 & 4Now called Pressure UlcerDTIDeep Tissue InjuryUnstageable due to Slough/Eschar – Pressure UlcerUnstageableUnstageable due to Non-removable Dressing/Device – Pressure Ulcer/InjuryPressure Ulcer that was staged and now has a “scab” indicates it ishealing and therefore staging does not change.3618
11/06/2018Pressure Ulcers/Injuries at Each StageDEFINITIONSStage 2Stage 3Stage 4Stage 2 pressureulcers arecharacterized bypartial thickness lossof dermis presentingas a shallow openulcer with a red-pinkwound bed, withoutslough. May alsopresent as an intactor open/rupturedblister.Stage 3 pressure ulcersare characterized by fullthickness tissue loss.Subcutaneous fat may bevisible but bone, tendonor muscle is not exposed.Slough may be presentbut does not obscure thedepth of tissue loss. Mayinclude undermining ortunneling.Stage 4 pressure ulcersare characterized by fullthickness tissue losswith exposed bone,tendon or muscle.Slough or eschar may bepresent on some partsof the wound bed.Often includesundermining andtunneling.SLOUGH TISSUENon-viable yellow, tan,gray, green or browntissue; usually moist,can be soft, stringy andmucinous in texture.Slough may beadherent to the base ofthe wound or presentin clumps throughoutthe wound bed.ESCHAR TISSUEDead or devitalizedtissue that is hard orsoft in texture; usuallyblack, brown, or tan incolor, and may appearscab-like. Necrotictissue and eschar areusually firmly adherentto the base of thewound and often thesides/edges of thewound.If any bone, tendon or muscle or joint capsule (Stage 4 structures) isvisible, the pressure ulcer should be reported as a Stage 4 pressureulcer, regardless of the presence or absence of slough and/or eschar inthe wound bed.37Pressure Ulcer / Injury Guidance Skin assessment should be completed as close to that actual time ofthe SOC/ROC as possible Report pressure ulcer/injury stage (or whether unstageable) based on the firstskin assessment Do Not change OASIS coding if the ulcer/injury increases in numerical stage(worsens) or becomes stageable or unstageable within the assessment timeperiod Once a Stage 2, 3, or 4 pressure ulcer is completely covered with newepithelial tissue, it is considered healed and no longer reported as apressure ulcer A pressure ulcer treated with a skin graft is a surgical wound until thegraft edges are completely healed3819
11/06/2018Pressure Ulcer / Injury GuidancePressure ulcers/injuries that are known to be present but that are unobservable due to a dressing/device,such as a cast, that cannot be removed to assess the skin underneath. “Known” refers to whendocumentation is available that states a pressure ulcer/injury exists under the non-removabledressing/device.Pressure ulcers that have eschar (tan, black, or brown) or slough (yellow, tan, gray, green or brown) tissuepresent such that the anatomic depth of soft tissue damage cannot be visualized in the wound bed,should be classified as unstageable. If the wound bed is only partially covered by eschar or slough, andthe anatomical depth of tissue damage can be visualized, numerically stage the ulcer, and do not codethis as unstageable.Pressure ulcers that are covered with slough and/or eschar, and the wound bed cannot be visualized,should be coded as unstageable because the true anatomic depth of soft tissue damage (and thereforestage) cannot be determined. Only until enough slough and/or eschar is removed to expose the anatomicdepth of soft tissue damage involved, can the stage of the wound be determined.39Revised Item(M1306)Enter CodeM1306 Unhealed PU/Injury atStage 2 or HigherDoes this patient have at least one Unhealed Pressure Ulcer/Injury at Stage 2 or Higher or designated asUnstageable? (Excludes Stage 1 pressure injuries and all healed pressure ulcers/injuries)0 No [Go to M1322 at SOC/ROC/FU; Go to M1324 at DC]1 YesIncorporated National Pressure Ulcer Advisory Panel (NPUAP) terminologyupdates to align with other PAC instruments.Item text revised: Replaced “excludes .healed Stage 2 pressure ulcers” with “excludes .allhealed pressure ulcers” Added Pressure ulcer/injuriesTIME POINTS ITEM(S) COMPLETED Start of careITEM INTENT Resumption of careIdentifies the presence or absence of Follow-upUnhealed Stage 2 or higher or Unstageable Discharge from agency – not topressure ulcers/injuries only.inpatient facility4020
11/06/2018M1307 Oldest Stage 2 Pressure Ulcer(M1307)Enter CodeThe Oldest Stage 2 Pressure Ulcer that is present at discharge: (Excludes healed Stage 2 pressure ulcers)12Was present at the most recent SOC/ROC assessmentDeveloped since the most recent SOC/ROC assessment. Record date pressure ulcer first identified:MonthDayYearNA No Stage 2 pressure ulcers are present at dischargeITEM INTENT The intent of this item is to a) identify theoldest Stage 2 pressure ulcer that is presentat the time of discharge and is not fullyepithelialized (healed), b) assess the length oftime this ulcer remained unhealed while thepatient received care from the home healthagency and c) identify patients who developStage 2 pressure ulcers while under the careof the agency.TIME POINTS ITEM(S) COMPLETEDDischarge from agency – not to inpatientfacility41M1311 Current Number of UnhealedPressure Ulcers/Injuries at Each StageRevised ItemM1311 updated and changed: Now shows time point versions for each time point an assessment iscompleted For SOC/ROC and Follow-up OASIS assessments Shows A1 to F1 For Discharge OASIS assessment Shows A1, A2, B1, B2, to F1, F2 SOC/ROC and Discharge information used to calculate revised pressureulcer measureA Dash is a Alignment with other PAC instruments Incorporated NPUAP terminology updates Skip pattern language and directions modifiedvalid responsefor DISCHARGEONLY.4221
11/06/2018M1311 Current Number of UnhealedPressure Ulcers/Injuries at Each StageRevised Item(M1311) Current Number of Unhealed Pressure Ulcers/Injuries at Each Stage (SOC/ROC)A1.Stage 2: Partial thickness loss of dermis presenting as a shallow open ulcer with a red or pink wound bed,without slough. May also present as an intact or open/ruptured blister.Number of Stage 2 pressure ulcersB1.Stage 3: Full thickness tissue loss. Subcutaneous fat may be visible but bone, tendon, or muscle is notexposed. Slough may be present but does not obscure the depth of tissue loss. May include undermining andtunneling. Number of Stage 3 pressure ulcersC1.Stage 4: Full thickness tissue loss with exposed bone, tendon, or muscle. Slough or eschar may be present onsome parts of the wound bed. Often includes undermining and tunneling.Number of Stage 4 pressure ulcersD1.Unstageable: Non-removable dressing/device: Known but not stageable due to non-removabledressing/deviceNumber of unstageable pressure ulcers/injuries due to non-removable dressing/deviceE1.Unstageable: Slough and/or eschar: Known but not stageable due to coverage of wound bed by sloughand/or escharNumber of unstageable pressure ulcers due to coverage of wound bed by slough and/or escharF1.Unstageable: Deep tissue injuryNumber of unstageable pressure injuries presenting as deep tissue injuryEnterNumber43(M1311) Current Number of Unhealed Pressure Ulcers/Injuries at Each Stage (Discharge)Enter NumberA1. Stage 2: Partial thickness loss of dermis presenting as a shallow open ulcer with a red or pink wound bed, without slough. May also present as an intact oropen/ruptured blister. Number of Stage 2 pressure ulcers [If 0 – Go to M1311B1, Stage 3]A2. Number of these Stage 2 pressure ulcers that were present at most recent SOC/ROC – enter how many were noted at the time of most recent SOC/ROCB1. Stage 3: Full thickness tissue loss. Subcutaneous fat may be visible but bone, tendon, or muscle is not exposed. Slough may be present but does not obscure thedepth of tissue loss. May include undermining and tunneling. Number of Stage 3 pressure ulcers [If 0 – Go to M1311C1, Stage 4]B2. Number of these Stage 3 pressure ulcers that were present at most recent SOC/ROC – enter how many were noted at the time of most recent SOC/ROCC1. Stage 4: Full thickness tissue loss with exposed bone, tendon, or muscle. Slough or eschar may be present on some parts of the wound bed. Often includesundermining and tunneling. Number of Stage 4 pressure ulcers [If 0 – Go to M1311D1, Unstageable: Non-removable dressing/device]C2. Number of these Stage 4 pressure ulcers that were present at most recent SOC/ROC – enter how many were noted at the time of mostrecent SOC/ROCD1. Unstageable: Non-removable dressing/device: Known but not stageable due to non-removable dressing/device Number of unstageable pressure ulcers/injuriesdue to non-removable dressing/device [If 0 – Go to M1311E1, Unstageable: Slough and/or eschar]D2. Number of these unstageable pressure ulcers/injuries that were present at most recent SOC/ROC – enter how many were noted at the time of most recentSOC/ROCE1. Unstageable: Slough and/or eschar: Known but not stageable due to coverage of wound bed by slough and/or eschar Number of unstageable pressure ulcersdue to coverage of wound bed by slough and/or eschar [If 0 – Go to M1311F1, Unstageable: Deep tissue injury]E2. Number of these unstageable pressure ulcers that were present at most recent SOC/ROC – enter how many were noted at the time of most recent SOC/ROCF1. Unstageable: Deep tissue injury Number of unstageable pressure injuries presenting as deep tissue injury [If 0 – Go to M1324]F2. Number of these unstageable pressure ulcers that were present at most recent SOC/ROC – enter how many were noted at the time of most recent SOC/ROC4422
11/06/2018M1311 Current Number of UnhealedPressure Ulcers/Injuries at Each StageITEM INTENT This item identifies the number of pressure ulcers/injuries ateach stage (Stage 2, 3, and 4) and designated as Unstageable,that are observed on assessment. At discharge, this item also identifies if each pressureulcer/injury present on the discharge assessment was observedat the same stage at the time of the most recent SOC/ROC. Stage 1 pressure injuries and all healed pressure ulcers/injuriesare not reported in this item.TIME POINTS ITEMS COMPLETED Start of Care Resumption of Care Follow-up Discharge from agency – not to inpatientfacility45M1311 Current Number of UnhealedPressure Ulcers/Injuries at Each StageDetermining “Present at the most recent SOC/ROC” to answer M1311 For each pressure ulcer/injury observed and coded in items M1311A1-F1 on Discharge,determine whether that pressure ulcer/injury was observed at the same stage at the time ofthe most recent SOC/ROC, and did not form during this home health quality episode. If the pressure ulcer/injury was unstageable at SOC/ROC, but becomes numerically stageablelater, when completing the Discharge assessment, its “Present at the most recent SOC/ROC”stage should be considered the stage at which it first becomes numerically stageable. If it subsequently increases in numerical stage, do not report the higher stage ulcer as being“present at the most recent SOC/ROC” when completing the Discharge assessment. The general standard of practice for patients starting or resuming care is that patientassessments are completed as close to the actual time of the SOC/ROC as possible. For example, if a pressure ulcer/injury that is identified on the SOC date increases in numericalstage within the assessment time frame, the stage of the pressure ulcer/injury at the first skinassessment completed would be reported in M1311X1 at the SOC.4623
11/06/2018M1311 Current Number of UnhealedPressure Ulcers/Injuries at Each StageEXAMPLE 1The RN assesses Mr. J’s skin at the SOC and identifies a DTI with intact skin onhis left heel.This DTI remains unchanged until the RN skin assessment 10 days later,which reveals open skin pres
Understand OASIS M-item coding instructions to accurately code new and revised OASIS items Identify available resources for implementing OASIS-D 2. 11/06/2018 2 Why OASIS-D? Improving Medicare Post-Acute Care Transformation Act of 2014 Bipartisan bill signed into law by President Obama October 6, 2014