Transcription
Home HealthValue-Based Purchasing(HHVBP)OASIS Measure:Improvement in DyspneaMarch 23, 2017Prepared for CMS by the HHVBP Technical Assistance, contract number HHSM-500-2014-0033I. If youhave suggestions for additional topics, please email the helpdesk at HHVBPquestions@cms.hhs.gov.
HHVBP Learning Event StructureHHVBP Model CurriculumQualityImprovementHHVBP ovementin Dyspnea2
Agenda Review the OASIS-based qualitymeasure of Improvement in Dyspnea Discuss clinical and operationalprocesses and interventions to impactthis measure Provide resources and support for qualityimprovement Highlight high performing HHAs forcollaborative learning3
Handouts & QuestionsHandouts Presentation slides COPD Zone Tool (Patient Self-Management Tool) Improvement in Dyspnea Care Path Available via the green “Resources” widget for livepresentations and on HHVBP Connect if viewing arecordingQuestions Questions may be submitted through the Q&A feature onyour screen OR HHVBP Help Desk atHHVBPquestions@cms.hhs.gov4
Webinar Console Overview5
Important Updates and Reminders New Measures Data Submission» April 1st (12:01am ET) through- April 17th (3:00 AM ET) 1st quarter of 2017 (data collection for January 1, 2017 –March 31, 2017)– Advance Care Plan– Herpes Zoster Annual reporting (data collection for October 1, 2016through March 31, 2017)– Influenza Vaccination Coverage for Home HealthCare Personnel Help Desk Assistance» Hours: Monday- Friday, 8:30am-7:30-m ET» Closed weekends and federal holidays6
Questions to Consider1.What are your current strategies formanaging patients with dyspnea?2.What are ways in which your currentstrategies for managing patients withdyspnea could improve?7
Measure Review:Improvement in Dyspnea
TPS & Annual PaymentAdjustmentsImprovement in Dyspneameasure is used tocalculate your TPS17 QualityMeasureResults(OASIS, Claims,HHCAHPS –basedmeasures)QuarterlyInterimPerformanceReport (IPR)TotalPerformanceScore (TPS)AnnualPaymentAdjustment9
Improvement in DyspneaMeasure Description Percentage of home health episodes of care duringwhich the patient became less short of breath ordyspneic.NumeratorNumber of home health quality episodes where thedischarge assessment indicates less dyspnea atdischarge than at start (or resumption) of careDenominatorNumber of home health quality episodes ending with adischarge during the reporting period, other than thosecovered by generic or measure-specific exclusions.Measure-specificExclusionsHome health quality episodes for which the patient, atstart/resumption of care, was not short of breath at anytime, episodes that end with inpatient facility transfer ordeath.OASIS-C2 Item(s)Used(M1400) When is the patient dyspneic?10
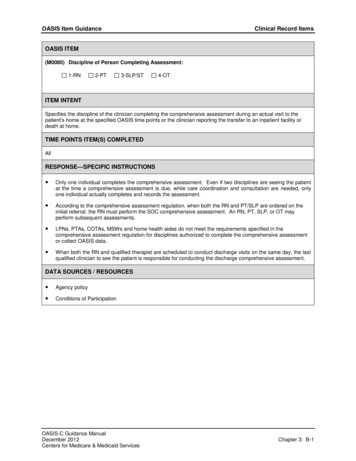
OASIS Guidance:Improvement in DyspneaCollectedatSOC/ROC& DischargeOASIS ITEM(M1400) When is the patient dyspneic or noticeably Short of Breath?0 - Patient is not short of breath1 - When walking more than 20 feet, climbing stairs2 - With moderate exertion (e.g., while dressing, using commode or bedpan, walking distancesless than 20 feet)3 - With minimal exertion (e.g., while eating, talking, or performing other ADLs) or with agitation4 - At rest (during day or night) Level of Exertion Causing Dyspnea» Report what is true on the day of assessment 24 hours immediately preceding the home visit and the time spent bythe clinician in the home» Refer to examples included in response to determine the amountof effort it took to cause dyspnea (examples are illustrative, notabsolutes)11
OASIS Guidance:Improvement in Dyspnea (cont.) Oxygen Use» If patient uses oxygen continuously, assess with oxygen» If oxygen is used intermittently, assess without oxygen» Assessment based on patient’s use of oxygen, not physician'sorder Modifications of the Patient’s Environment» Environment may have been modified to address dyspnea: E.g., Sleeps in recliner or sleeps with two pillows» If patient has not demonstrated or reported shortness of breathduring the “day of assessment” timeframe,” select “0” eventhough the environment or patient activities were modified inorder to avoid SOB12
What We Need to Succeed?Measure: Improvement in Dyspnea“IMPROVEMENT Achieved”Discharge OASIS score is numerically lowerwhen compared to SOC/ROCExample: SOC – “2” and DC – “1” Improvement13
Measure Improvement Strategies
Measure Improvement Strategies(cont.)Basic Clinical EducationTools and InterventionsPeer-to-Peer Collaboration15
Measure Improvement Strategies:Basic Clinical EducationBasic Clinical EducationTools and InterventionsPeer-to-Peer Collaboration16
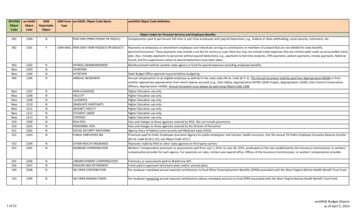
Sample Clinical Staff EducationResourcesTopicSample Resource1. Measure Specifics CMS Home Health Quality MeasureTables2. OASIS Data Accuracy OASIS C-2 Guidance Manual OASIS Q&As3. Basics of ChronicDisease Management 4. Clinical Best Practices 5. Teach-Back HHQI Basics of Chronic DiseaseManagement Course (free with CEUs)VNAA Blueprint for Excellence: ClinicalConditions & Symptom Management:Chronic Obstructive PulmonaryDisease—COPDCOPD Zone Tool10 Elements of Competency for UsingTeach-Back17
1. CMS Home HealthQuality Measure Tables
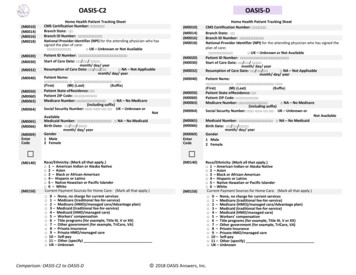
2. CMS OASIS GuidanceOASIS-C2Guidance ManualOASIS Q&As19
3. Basics of Chronic DiseaseManagement20
4. VNAA Blueprint for Excellence21
5. COPDZone Tool22
6. 10 Elementsof Competencyfor UsingTeach-backEffectively23
Measure Improvement Strategies:Tools and InterventionsBasic Clinical EducationTools and InterventionsPeer-to-Peer Collaboration24
Clinical Best Practices:Sample Paths to Improvement25
SamplePatientWorkbook26
Care Path &InterventionExamples27
Care Path & Intervention Examples(cont.)23128
4Consider: Is the patientshort of breath or at riskfor having issues withshortness of breath.5Care Path
Care Path (cont.)67
78Care Path:Interventions
Care Path:Interventions(cont.)
Home-Based Pulmonary Rehab:What does it look like? Aerobic trainingØØØØSet goal for walking distanceRecord distance using a pedometer30 minutes, 5 times per weekRecord completion in home diary Upper and lower limb strength trainingØ Functional tasks: stair training, sit to stand from chair, etc.Ø Free weight training Patients contacted by clinician (weekly, e.g., forapprox. 7 weeks)ØØØØØReview the home diaryProgress the exercise prescriptionDeliver disease-specific self-management trainingExplore and build motivation for changeMove towards commitment and action33
Today’s DiscussionBasic Clinical EducationTools and InterventionsPeer-to-Peer Collaboration34
Nemaha County Home CareJere Gravatt, RN, DirectorNemaha County Home CareAuburn, Nebraska35
Elite Home Health and HospiceSheri Osburn, Director of Clinical ServicesElite Home Health and HospiceClarkston, Washington36
Discussion!37
Resources & Reminders38
Mark Your CalendarsUpcoming Learning EventTopicDateTimeOASIS and HHCAHPSMeasure: Improvement inMedication-Related MeasuresApril 6, 20172:00 PM ETLearning from the Literature:Highlights from theEnvironmental ScanApril 20, 20172:00 PM ETAll learning events will be held at 2 PM, Eastern Time.Please register via the HHVBP Connect Calendar.39
QuestionsDo you have questions about the HHVBP Model?Contact the HHVBP Model Help Desk atHHVBPquestions@cms.hhs.gov.If you are experiencing technical issues withgaining access to the HHVBP Secure Portal orHHVBP Connect, please call:(844) 280-5628.Stay on the line until your issue is resolved.40
HHVBP Connect Chatter Join the discussion!» Engage with your peers on HHVBP Connect by liking andcommenting on their posts If you would like to ask a question of your peers:» Log into the HHVBP Connect site unityLogin» On the Chatter page, select “Post” at the top and type in yourquestion and post to the group To request access to HHVBP Connect, visit the HHVBPConnect site and select the new user registration link» Follow the on-screen instructions» The CMMI Help Desk will contact you to complete the registrationprocess
Thank you!Prepared for CMS by the HHVBP Technical Assistance, contract number HHSM-500-2014-0033I. If youhave suggestions for additional topics, please email the helpdesk at HHVBPquestions@cms.hhs.gov.
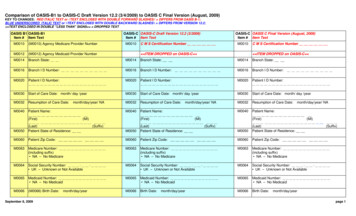
2. OASIS Data Accuracy OASIS C-2 Guidance Manual OASIS Q&As 3. Basics of Chronic Disease Management HHQI Basics of Chronic Disease Management Course (free with CEUs) 4. Clinical Best Practices VNAA Blueprint for Excellence: Clinical Conditions & Symptom Management: Chron