Transcription
Perioperative Care ofOur Cath Lab Patients:Why what happens in the cath labshouldn’t stay in the cath labPaul Johnson, MD, FACCPiedmont Heart Institute - Athens
OverviewPre-OpEvaluation Consent CIN PreventionVascular Access Complicationprevention andmanagement Femoral vs. Radial
OverviewPre-OpEvaluation Consent CIN Prevention
Procedure Related Complications of Cardiac CatheterizationJ Am Coll Cardiol. 2012 Nov 13;60(20):2017-31
Informed Consent Overall risk of serious life threateningcomplication of death, myocardial infarction,or stroke is 0.1%. Informed Consent– Risks, benefits, alternatives– Ultimately the responsibility of the operator– If PCI is a possible outcome, this should beincluded in the consent– Not required to include all risks
Informed Consent Ultimately, it is the responsibility of theoperator to ensure this is done.
Contrast Induced Nephropathy CIN is a rise in serum Cr 0.5 mg/dL or 25%increase above baseline. Differential includes hypotension, renalatheroemboli, acute interstitial nephritis Time course– Rise in Cr occurs in 24-48 hours– Peaks at 3-5 days– Resolves over one week
Contrast Induced Nephropathy CIN is associated with adverse outcomes– 5 to 20 fold increase risk of early events In-hospital MITarget vessel occlusionProlonged hospital stayEarly mortality– Long term adverse associations include 11-foldincrease in ESRD, re-hospitalization, and 3-4 timesincreased risk of mortalityJAMA 1996;275:1489-94.Circulation 2011;123:409-16.Circulation 2002;105:2259-64.
Risk factors for Contrast-Induced NephropathyPatient FactorsChronic kidney diseaseCongestive heart failureAge greater than 70 years oldHypotension (at time ofprocedure)History of hypertensionAnemiaDiabetes mellitusNephrotoxic medicationsFemale genderProcedural FactorsVolume of contrastUse of intra-aortic balloon pumpUrgent or emergent procedureRepeat contrast exposure within72 hoursHyperosmolar contrastCathSAP 4
Predictive Model of CINJACC 2004; 44: 1393-9
Alternative Model of CINAm J Cardiol 2004; 93:1515-19Ann Int Med; 150:170-7
Preventing Contrast-Induced Nephropathy Identify risks– Higher risk – eGFR 60 mL/min/1.73m*m– Diabetes Manage medications– Hold nephrotoxic drugs (e.g., NSAIDS) Management intravascular volume– Hydrate with normal saline pre-cath– LVEDP guided post cath hydration Radiographic contrast– Minimize contrast volume– Use either low-osmolar or iso-osmolar contrast Follow-up: Obtain 48 hour creatinineBashore JACC 2012; 59: 2221-305
Preventing Contrast-Induced NephropathyCIN Prevention: Pre-Cath Hydration
Preventing Contrast-Induced NephropathyCIN Prevention: Post-Cath Hydration
OverviewPre-OpEvaluation Consent CIN PreventionVascular Access Complicationprevention andmanagement Femoral vs. Radial
Preventing Access Complications Step 1Recognize that vascularaccess is taken for granted,under-investigated, and overrepresented in complications.Image: https://www.researchgate.net/figure/224830285 fig1 Fig-1-Large-right-groin-and-forearm-hematomas
Most common: hematomaMost lethal: retroperitoneal hemorrhageLocal complications of FA access: 2-10% Hematoma (1-12%) Pseudoaneurysm (1-6%) AV fistula ( 1%) Vessel laceration ( 1%) Free bleeding Intimal dissection Ante- or retro-grade Retroperitoneal hemorrhage (0.2– 0.9%) Thickening of the perivasculartissues Neural damageInfectionVenous thrombosisPericatheter clotAcute vessel closure ( 1%) Thrombosis (small arterylumen)Complication rate has beenpersistent over manydecades
Usual Approach Keep poking untilyou get a gusher
Landmarks Used for Femoral PunctureAll Three1%Skin CreaseMaximum PulseBony rease40%Bone13%Pulse25%Grier D. Br J Radiol 1990;63:602.
This is NOT Normal AnatomyCFAPFASFA
Clinical Cardiology 34(11):700-2 · November 2011
Odds Ratio RPH 18:1
Preventing Access Complications IEAFH CenterlineCumulative Target ZoneStep 2:Choose a landmark. BIF
Preventing Access Complications Step 3Micropuncture
# Fold Increase in Blood Loss (Flow)18Preventing Access Complications16 14 Step 3Std needle (18g) 1.27 mm12Micropuncture (21g) .813 mm10Micropuncture In size 56%8645.9 fold inblood loss20020406080% Increase in Size of Residual Hole (Radius)100
Preventing Access Complications Step 4Good Closure Hold time– 15 minutes diagnostic– 30 minutes intervention– Bedrest 6 hours Hold location– Proximal– Over palpable pulse
Preventing Access ComplicationsRisk Factors for BleedingOddsRatioAge 75 vs. 552.59Heparin use postprocedure 2.46Severe renal impairment 2.25Age 65–74 vs. 552.18Female patient1.64Closure device use1.58Sheath size 7F–8 F vs. 6 1.53GP IIb/IIIa use1.39Longer procedure duration 1.2Risk cutaneous-coronary-interventions/Adapted from Doyle B, Ting HH, Bell MR, et al. Major femoral bleeding complications after PCI. JACC Cardiovasc Interv2008;1(2):202–209
Preventing Access ernal bleeding6.1Retroperitonealhematoma5.1Arterial thrombosis3.1Groin abscessMycotic aneurysm2.01.0Femoral Access ComplicationsRequiring InterventionsData from Lumsden AB, Peden EK, Bush RL, Lin PH. Complications of endovascular procedures atthe target site. In: Ouriel K, Katzen BT, Rosenfield K, editors. Complications in endovasculartherapy. New York: Taylor & Francis; 2006. p. 29–53.
Preventing Access ComplicationsPseudoaneurysmsProcedural FactorsCatheterization of both artery andveinCannulation of the superficial femoralor profunda femoris rather thancommon femoralInadequate compression postprocedureMore anticoagulation usedPatient FactorsObesityHemodialysisCalcified arteries Low puncture site Inadequate pressure Experience of -postcatheterization-pseudoaneurysms/
Preventing Access Complications Step 4Closure Devices? Patient comfort andconvenience– Early hemostasis– Early ambulation Decreasedcomplications?– NO!
Meta-analysis of Closure DevicesOR (95% CI)Heterogeneity testP-valueDx studies1.44 [0.43, 4.82]†0.66 [0.18/, 2.38]*0.00030.16PCI studies1.11 [0.94, 1.33]*1.35 [0.87, 2.11]*0.220.15Both Dx PCI studies1.83[1.15,2.90]†1.15 [0.67, 1.98]*0.0010.43All studies1.34 [1.01, 1.79]†1.30 [0.90,1.87]* 0.00010.190.1 0.2 0.5 1.0 2.0 5.0 10.0Favors ACDFavors ControlACC/AHA Class III indication to lower complication ratesNikolsky et al. JACC 2004.
Preventing Access Complications1. Don’t take access for granted2. Access the common femoral over the femoralhead3. Use micropuncture4. Quality hemostasis/closure5. GO RADIAL!
Registry Data: Transradial PCI in the UK33Katib et al. JACC Intv 2015.
Transradial Use for STEMI in the USBaklanov, et al. JACC 2013.
Large Associated BenefitKatib et al. JACC Intv 2015.
Oximetry PlethysmographyThe clamp sensor is applied to the thumbn 1,010 patientsNo damping of pulse tracingimmediately after radial arterycompression15%Damping of pulse tracing75%Loss of pulse tracing followedby recovery of pulse tracingwithin 2 minutes5%Loss of pulse tracing withoutrecovery within 2 minutes.5%Barbeau et al. Am Heart J 2004;147:489–93
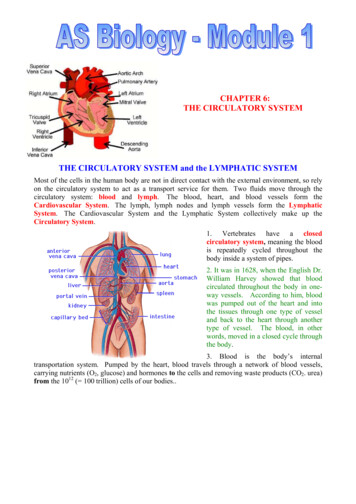
Arm is very well collateralized No correlation to hand ischemia & arterial lines1 Extensive radial CABG experience without ischemia Radial harvest with abnormal Allen’s Test is possible2Gunther von Hagens, Institute for Plastination, Heidelberg, Germany, www.bodyworlds.comTheoretical fears from an abnormal Allens Test is a poor excusefor a real risk of groin complications1. J Trauma 2006;206:468-702. Surg Today 2006;36(9):790-2.
TR band rochure.pdf
TR band management All patients with radial access will have TR bandand stabilization device (armboard) TR band deflation 1-2 hours after diagnostic cathand 2-4 hours for interventional cath Deflate air by 3 ml every 15 minutes until band isdeflated– If bleeding occurs, re-inflate band in 3 mL incrementsuntil bleeding stops Armboard for 24 hours or until discharge,whichever first
Hematoma or Swelling on Return to Room?
Hematoma or Swelling on Return to Room?transradial-summit.org
Managing a Perforation Early recognition Wrap potentialbleeding site Wrap forearmswelling not relatedto hemostasis deviceat any time
Conclusions Consent is a critical part of the procedure Think ahead to avoid contrast inducednephropathy Access is taken for granted, and is overrepresented in complications Radial access decreases bleeding, andmortality
Consent is a critical part of the procedure Think ahead to avoid contrast induced nephropathy Access is taken for granted, and is over-represented in compl