Transcription
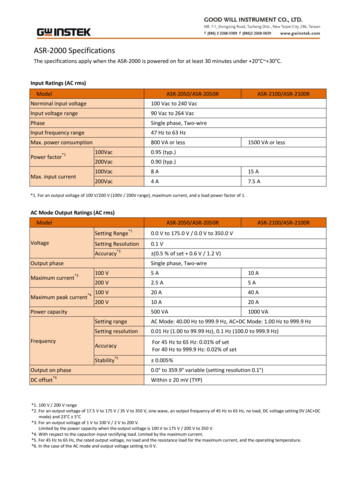
CHAPTER 42WOUND VAC: Tips and TricksAnnette Filiatrault, DPMINTRODUCTIONNegative pressure wound therapyAlternatively, a single-layered non-adherent mesheddressing such as Mepitel or dry Adaptic (not Xeroform, as(NP\(/D using the\7ound VAC (Vacuum-Assisted Closure@) system (KCI,San Antonio, TX) has become an importanr rreatmentmodality for a variety of wounds in numerous medicalfields and its indications and popularity have significantlygrown in the past few years. An excellent review ofVacuum-Assisted Closure in the lower extremity waspresented by J. Christopher Benson in the PodiatryInstitute's Update 2002.The purpose of this update is topresent some adjuncts to the normal application andprotocol of the \7ound VAC. such as methods to reducepain, prevent maceration, deal with a difficult location ofa wound, and the use of alternative dressings.PAINThere are difTerent methods available to help the sensatepatient that has pain either with the therapy itself or thefoam dressing changes. If the patient is experiencing paindespite attempted management with oral or venousanalgesics during the therapy, KCI recommends decreasingthe settings by 25 mm Hg increments until pain isresolved.' The Intermittent setting can sometimes bepainful for the sensate patient and changingtothecontinuous setting may cause less pain, although it maynot enhance granulation tissue as much as the intermittentsetting will.If the patient has pain with sponge dressing changesthan there are several techniques that can beused.Obviously, premedicating the patient prior to the dressingchange is the easiest measure that can be taken. The morenon-adherent white VersaFoam sponge may be usedinstead of the traditional black GranuloFoam sponge,which will overall be less painful to the patienr uponremoval, but again may not produce as rapid a rate ofgranulation tissue formation. Ensure that dressingchanges are performed at least every 48 hours for mostwounds, as decreasing the frequency of dressing changeswill allow ingrowth of granulation tissue into the spongeand therefore is more likely to cause pain upon removal.Daily dressing changes may be necessary for children asthey tend to have a rapid tissue response.'this is too oily) can be placed first into the wound andthen the sponge and drape are placed over this.3 Thesedressings will allow easier removal of the sponge from thewound. Another option would be to inject Xylocaine(without epinephrine) or a similar Iocal anestheticdirectly into the sponge a few minutes prior to removal orsoaking the sponge with saline prior to removal.' Topicallidocaine or EMLA@ after removal and actual injection oflocal anesthetic into the wound itself are less frequentlyused options. If there is pain from sharp debridement atbedside, consider oral analgesics and EMLA placedtopically under an occlusive dressing 30 minutes prior todebridement (not an FDA approved procedure, but anaccepted use in other countries).3 Sometimes pain can beelicited due to adherence of hair caught in the drape oradhesive, shaving the skin adjacent to the wound canalleviate this problem.MACERAIIONThe most common cause of macerated skin edges arounda wound receiving NPWT is lack of proper technique.Ensure that bleeding is controlled, the skin margins areclean and dry, the sponge does not extend onto the skinand is well within the wound, that there is a good overlapof the drape onto the skin (at least 4 cm), and that a skinadherent is used around the periphery of the wound.'Although Tincture of Benzoin and Mastisol have beenused in the past, most wound care staffhave converted tousing skin preparation materials that not only protect theskin, but also remove the oil from the skin enhancingadhesion of the drape. Examples of skin preps used areAllkare (Convatec, which has some alcohol in it and hasbeen know to sometimes cause a stinging sensation) and3M's or Smith & Nephewt "No-Sting" skin prep (whichlacks alcohol and therefore causes no stinging). Also, thephysician may also either stop the therapy for a few daysor increase the pressure setting to resolve maceration. Useof a skin barrier protectant such as Duoderm or nonadhesive bandage around the periphery and extending thedrape beyond these borders to better skin layers is anothermethod. If the toes must be included in the dressing
254CHAPTER 42of the location of the wound, place either castpadding or a small piece of sponge in berween the digits toprevent maceration. In a significantly exudative woundwith skin maceration, yeast can sometimes become aproblem which may require the use of topical Nystatinpowder, as well as better maceration control, for treatment.becauseLEAKAGEThe amount of drape material used should be kept toaminimum to prevent leaks or creases. For small leaks thatare hard to find, a skin prep may be lighdy spread over thedrape, this creates a film over the area and can sometimeseffectively enough, seal a small leak in the drape allowingfor proper suction. If trying to maintain suction and thetoes must be included because of the location of thewound, you can fold the drape from plantar to dorsal likea quesadilla and crimp the medial and lateral edges. Thistechnique may be useful when applying NPWT to adegloving foot injury. If it is difficult to locate the leak,methylene blue dye (1 mg diluted in 500 cc of sterilewater) may be applied onto the drape and rinsed after 3minutes. The blue dye will color the dressing at the site ofthe leak. This has been termed the "Maya Technique" byits originators.aSKIN FRAGILITYFragile skin or creased skin (such as at the anterior ankle)can also be protected with the use of wound care productssuch as Duoderm' or Tegasorbt, both of which the drapereadily sticks to. If these products are used, the drape mustextend past where they end to ensure a good seal. If the skinis becoming fragile or tender due to frequent sponge anddrape removal changes, KCI recommends cutting thedrape just around the sponge itself leaving the remainderof the drape on the skin, replacing the sponge and simplyapplying a new drape overtop of the old one for oneadditional dressing change only. KCI warns that morethan 2 drapes overlaid may impair vapor transmission ofthe drape.lSPONGE CONSIDERAIIONSAdapting the foam dimensions to mirror the wound is aneffective way to enhance granulation tissue formationusing NPWT. If there is an area in your wound of greaterdepth than the remainder of the wound, contour thesponge to be deeper at that one area and level with theremainder of the wound to enhance sponge contact tothis less responsive area. If dealing with a narrow tunnelor undermined wound, use the white VersaFoam materialand cut it to the same dimensions. It is not recommendedto use the black GranuloFoam sponge as it more fragileand there have been reported cases of portions of thefoam left in wounds causing foreign body reaction andinfection. The white VersaFoam sponge is more stableand does not break or pull apart comparatively, which isimportant for areas that may be difficult to visualize. Ona complex wound, it is recommended to document thenumber and location of separate foam pieces within thewound.' If more than one person is performing thesponge changes, this documentation can be written onthe drape itself to ensure foam pieces are not left withinthe wound. It is important that the wound not be overpacked with sponge material. Often it may be necessaryto split the sponge to half its width. Recently, KCI hasbegun offering more sponge dimension options thatalready are pre-cut to different sizes based on possiblewound dimensions.If a white VersaFoam sponge is used, understandthat it has less suction power the farther from the areathat the suction tube is applied to the sponge because it isa denser foam with higher tensile strength.r For example,if the suction is applied at the center of a circularVersaFoam sponge, the farther to the periphery of thesponge you go, the less negative pressure suction isachieved. However, the black GranuloFoam sponge hasreticulated or open pores, thereby ailowing equal suctionat every area of the foam irregardless of where the suctionis applied. To even out the suction when using a whiteVersaFoam sponge, either a layer of the GranuloFoammay be placed on top of the VersaFoam or a "zebra-stripe"of the black sponge may be layered over the white foamtoenhance the amountof suction at the periphery ofthe sponge.For wounds that are smaller than the T.R.A.C.rM pad,some modificationsin the application techniquearerecommended by KCI (Figure 1). Cut the foam to thewound dimensions, apply to the wound and drape as usual.Then cut a 2 cm hole in the drape over the foam, applyanother piece of foam l-2 cm beyond the dimensions ofthe T.R.A.C, pad on top of the first foam (the first drapeshould be of larger dimension than this second foam pieceto protect the skin). Lastly, apply the T.R.A.C. pad to theIarger piece of foam.'If the sponge is to be placed over sutures, staples, ora dehisced wound, KCI recommends covering these firstwith a non-adherent dressing prior to foam placement(Figure 2). This may protect the suture or staple frombecoming lodged into the GranuloFoam. Alternatively,
CHAPTER 42255Figure 2. Modified technique for dehisced rvounds. Apply a non-adherentdressing prior to loarn placement over the wound.'Figure 3. C-shaped cutting ofthe foam to bridge a plantar foot wound to thedorsal skin can transfer suction application to the dorsum ofthe foot.''%ar:r'ltr. .IJlt.t,d.r,. aiLFigure 1. Modified technique for wounds thatsmaller than the T.R.A.C.''' pad.'areVersaFoam may be used as it is more non-adherenr or placea piece ofdrape over the sutures as the first srep, rhen applythe foam dressings as usual.r It is also recommended toprotect the intact skin on either side of the incision linewith a KCI Drape or Tegaderm. Remove a drape usingsolvent when it has been placed over staples.Sponge placement may be combined also with aneiastic vessel loop shoelace technique for large soft tissueprogressive wound closure and augments the tensioncreated by NPWL Normal application of the foam isfollowed by utilizing a large elastic vessel loop that isstapled (staples perpendicular to skin edge with one end inepidermis and one in dermis) to the skin edges in ashoelace fashion over the foam and the drape is applied,The wound is re-evaluated every 48-72 hours and theskin-edges are approximated sequentially using theshoelace vessel loop technique until delayed primaryclosure is appropriate.t This technique can help avoidclosure by secondary intention or grafting.Figure 4. Depiction of bridged wounds, note the centralized applicatiorofsrrction.LBRIDGINGBridging between 2 sponges is a technique that may beuseful to either incorporate more than one wound to oneVA,C. unit or as a method to bring the suction from asite less assessable to a more convenient site, such astaking suction from a plantar wound to placing thesuction at the dorsum of the foot. This may also be auseful method to move tubing away from an area alreadycompromised to prevent breakdown from the tubingitself. Cutting the foam in a C-shape facilitates creation ofa plantar to dorsal bridge (Figure 3).'' Thke care to useeither a drape or a protective product such as Duodermunder the sponge bridge to protect the intact skin.u AIso,
256CFIAPTER 42apply the tubing or T.R.A.C. pad in a central location forequal suction to both wounds (Figure 4).' Do not bridgewounds if infection is suspected.BACTERIA, ODOR, AND IRRIGAIIONNP\7Thas not been shown to enhance bacterial clearanceoriginally thought, as evidenced by 2 recent studies in2004.'1j Alternatively, many physicians are using silverimpregnated wound care products at the surface of thewound as an adjunct to sponge placement and NP\VT.Acticoat (nanocrystalline silver-coated dressing, Smith &Nephew), Arglaes (silver powder or film, Medline), andSilversorb (silver gel, Medline) are just examples of whatsome physicians have used to decrease the bacterial countaswithin the wound while still providing NP\ML' If adressing is used, it must be meshed or fenestrated to allowadequate suction of the exudate. Recently, KCI hasintroduced a silver impregnated sponge called VA.C.GranuloFoam Silver. If the wound is infected and thephysician chooses to continue with NPWT, KCIrecommends changing the dressing every 12-24 hours,then resume the normal 48 hour intervals when CFU'sdrop below 105.' Obviously, sharp debridement of anynecrotic tissue during therapy should be performedwhen present.As frequent VA.C. users are aware, there is a uniqueodor associated with the interaction of the sponge and theexudates noted on dressing changes. Certainly, if there isa strong malodor one should first rule out an activeinfection. \found flushing at dressing changes or use of asilver product may decrease this odor and the bacterialIoad within the wound. Sometimes it is the machine, thecanister, or, in the case of the Freedom VA.C., thecarrying pouch that has absorbed this odor. Changing thecanister or, if need be, the machine may resolve this issue.Canisters are available with Isolysert which can reduceodor from the canister itself.' If the Freedom V.A.C.pouch has absorbed odor and is the cause of the badsmell, some have suggested placing a dryer sheet inthe pouch.Another available product is the Instili VA.C. thatprovides NP\fT while enabiing the physician to instillIocal anesthetic or antibiotic into the wound. \,XAiledifferent antibiotics have been used most recommendeither Clorpactin or a Sulfa preparation. The author hasnot personally used the Instill V.A,C. product; however,many of the wound care staff do not favor this modalitycompared to the standard NP\7T products in terms ofeaseofuse.If irrigation of the woundwithNP\7!is desiredin conjunctiona soft red rubber catheter (10 French) can beimbedded into the sponge and clamped off duringNPWT. Therapy may be briefly stopped and the woundmay be flushed with saline daily utilizing the catheter.Others have advocated using an angio-catheter tocontinuously instill saline during therapy itself at a rate ofaround 20 cclhour. Intermittent flushing or continuousflow of saline into the wound is by no means a standardpractice or normally necessary other than at dressingchanges. However, some physicians use this as an adjunctto break-up more viscousprevent optimal NP\ru.exudate that might otherwiseMINIMAL CHANGEIN \rOUND DIMENSIONSIfthe wound appears stalled over a 7 to 2 week period,re-evaluate the wound for infection or adequate pressureoff-loading and assess the nutritional status of thepatient.l Additionally, KCI recommends cutting the foamslightly smaller than the wound, performinga."therapeutic pause" of therapy for l-2 days beforere-initiating therapy, changing the Continuous orIntermittent setting to the opposite setting, or removingany epithelial cells from the wound surface if presentprior to full-granulation of the wound.'PRESSURE SETTINGSFor most foot and ankle wounds using the standardGranuloFoam black sponge, the pressure setting is placedat 725 mm Hg Continuous for the first 48 hours thenchanged to Intermittent therapy of 5 minutes on and 2minutes off; as Intermittent therapy has shown to increaserate of granulation tissue formation.l If using theVersaFoam, the pressure may need to be increased up to775 mm Hg if there is more drainage. Increasing thesetting in 25 mm Hg increments may be advantageouswith excessive drainage, large volume wounds, tunneledwounds, or with a tenuous seal. Decreasing the sefiing by25 mm Hg increments can be performed if there isbruising in the wound bed, pain, an elderly patient,excessive bleeding, peripheral vascular disease, or excessivegranulation tissue formation.' Start with a lower settingsuch as 50-75 mm Hg if the patient is emaciated, elderly,on anticoagulants, or over exposed tendon.e A setting of75 mm Hg Continuous is more typical when the NP\[Tis used in conjunction with skin or bio-engineered tissuegrafts (5-7 days post-placement of the graft) or as a settingin areas requiring less suction such as adjacent to tendons(like a dehisced Achilles tendon repair incision). Keep thesetting on Continuous if dealing with a tunneling wounduntil the tunnel is closed.'
257CHAPTER 42Settings and protocol compliance are easilymonitored in an inpatient situation. tX/hen treating anACKNOIUTLEDGMENToutpatient, the Freedom V.A.C. has an hour log that youcan check to see if your patient is being compliant at homeand you also have the ability to lock-out the patient fromthe device and manipulating the settings on their own.Most of these tips and tricks have been passed to the authorfrom the wound care staff at Piedmont Hospital (Atlanta,GA) who deal with complicated wounds and \foundVA.C. applications every day in a variety of medicalspecialties. Additiona,lly, much of the provided informationcan be found in KCI's "V.A.C.@ Therapy ClinicalLITERAIURE UPDAIEGuidelines," which is also available on their website.Until the past fewtolittle research had been performedascertain the mechanism by which VAC therapyyears,REFERENCESachieved its positive clinical outcomes. Chen et al recentlypublished an experimental study that showed that vacuum1.assisted closure promotes blood circulation and reduces2.edema by increasing capillary caliber and blood volume,stimulating angiogenesis, narrowing endothelial space andrestoring capillary basement membrane integriry.'o Saxenaet al used a technique called finite element modeling toshow that the VAC created tissue microdeformations thatmay promote cell proliferation, cell division, angiogenesis,and a local increase in growth factors." Bacterial load3.4.5.6.however, does not decrease with VAC therapy as waspreviously thought, as shown in rwo articles in 2004, andtherefore is excluded as a mechanism by which the VAC7.8.improves wounds.''nCONCLUSIONNPWTaccelerates wound healingina varieqy of wound9.10.Closure devices. Ostomy Wound Manag 2002;48:38-43.Bar-Mejr E, Tamir J, \Winkler E. Maya technique for Vacuum-assistedClosure Sealing. Plast Recon Surg 2005 116:931.Mora SG, \Tindham ST, Cross JM, Melton SM, Rue L\(. Vacuumassisted complex wound closure with elastic vessel loop augmentation: anovel tcchnique. / 'Vound Care 2003;72:212-3.Greer SE, Duthie E, Cartolano B, Koehler KM, Maydick-Youngberg D,Longaker MT. Techniques for applying subatmospheric pressure dressing to wounds in diflicult regions of anatomy. J\Y/OCN 1999;26:250-3.\Weed T, RatliffC, Drake DB.Quantifting bacterial bioburden duringnegative pressure wound therapy. Ann Pldx Surg2004;52:276-9.MouEs CM, Vos MC, VanDenBemd, GJ, Stilnen T, Hovius ER.Bacterial load in relation to vacuum-assisted closure wound therapy: aprospectir.e randomized trial. \Yound Repair and Regeneration200412:1L-7.Sibbald RG, Mahoney J, and The VAC@ Therapy Canadian ConsensusGroup. A consensus report on the use of vacuum-assisted closure inchronic, difficult-to-heal wounds. Oxom/rYound Manag 2003;49:52-66.Chen SZ, Li J, Li XY, and Xu LS. Effects ofvacuum-assisted closure onwound microcirculation: an experimental sudy. Asiantypes and clinical situations. Adapting to new applications,adjuncts, products, and complications enables physiciansto provide the best qualiry ofcare to their patients.V.A.C. Therapl. Clinical Guidelines manual, Iiterature #2-B-128. KCILicensing, Inc. San Antonio, Texas; 2004.Venturi ML, Attinger CE, Mesbahi AN, Hess DL, Graw KS.Mechanisms and clinical applications of the Vacuum-Assisted Closure(VAC) device. Am J Clin Dermatol2005:6:185-94.Krasner DL. Managing wound pain in patients with Vacuum-Assisted11.JSurg 2005:28:2ll-7.Suena V, Hwang C\W, Huang S, Eichbaum Q. Ingber D, Orgill DP.Vacuum-assisted closure: microdeformations of wounds and cellproliferation. Pks Recon Surg 2004;14:1086-9 6.
effectively enough, seal a small leak in the drape allowing for proper suction. If trying to maintain suction and the toes must be included because of the location of the wound, you can fold the drape from plantar to dorsal like a quesadilla and crimp the medial and lateral ed