Transcription
Laboratory Guide: Methodologies forAntimicrobial Susceptibility TestingAPEC Sub-Committee on Standards and ConformanceMay 2020
APEC Project: CTI 24 2017AProduced byLisette LaPierre / Javiera Cornejo / Arantxa AsunFaculty of Veterinary Science University of Chile (FAVET)Av. Santa Rosa 11735, La Pintana ChileConstanza Vergara / Diego VarelaChilean Food Quality and Safety Agency (ACHIPIA)Nueva York 17, Piso 4, Santiago ChileForAsia-Pacific Economic Cooperation Secretariat35 Heng Mui Keng TerraceSingapore 119616Tel: (65) 68919 600Fax: (65) 68919 690Email: info@apec.orgWebsite: www.apec.org 2020 APEC SecretariatAPEC#220-CT-03.2
erial Isolation, Identification and StorageChapter 1:Chapter 3:How it worksMediaInoculumAntimicrobial diskControl plateIncubationReading and measurement of zones of inhibitionInterpretation of resultsRejection criteriaManual SystemE-test AdvantagesLimitationsAutomated Broth Microdilution SystemsVITEK Systems (Classic, VITEK 2 )MicroScan WalkAway Becton Dickinson Phoenix Sensititre ARIS 2X SystemAdvantages and Disadvantages of AutomatedSystemsDisk Diffusion MethodChapter 2:Minimal InhibitoryConcentration TestHow it worksMediaInoculumInoculationControl PlateIncubationReading the MIC valuesCommercial SystemsChapter 4:Quality ControlQuality Assurance Program for ASTQC StrainsAcceptable RangesStorageFrequency of TestingQuality SystemsAnnexesGlossaryReferencesAMR Antimicrobial ResistanceAST Antimicrobial SurveillanceATCCAmerican Type Culture CollectionCFU Colony-Forming UnitCLIAClinical Laboratory Improvement AmendmentsCLSIClinical and Laboratory Standards Institute (formerly NCCLS)EUCASTEuropean Committee on Antimicrobial Susceptibility TestingFDAFood and Drug AdministrationMHA Mueller-Hinton AgarMHB Mueller-Hinton BrothMICMinimal Inhibitory ConcentrationQA Quality AssuranceQC Quality ControlQS Quality System
IntroductionBacteria present in our environment may cause several diseases and mortality in farm animals, for this reasona wide range of antimicrobials are used to keep animals healthy. Antimicrobials in the last decades havebeen misused as some treatments have not been followed through, wrong dosage was used, or the sameantimicrobial was used in several therapies without alternating active ingredients, which has led to longerrecovery times from the diseases, and overall less effective and costlier treatments. More importantly, lackof veterinary guidance or ignorance regarding antimicrobials may increase the prevalence of transferenceof resistance genes to bacteria in the environment, rendering current antimicrobials ineffective. Resistantfoodborne bacteria are capable of transmitting resistance genes to commensal bacteria in humans andto zoonotic bacteria, for this reason testing bacteria isolated from food samples is practical not only forits importance yielding useful information for animal welfare, but also because of its importance in publichealth.There are several antimicrobials used in farm animals worldwide, therefore testing for susceptibility andresistance of bacteria to different drugs needs to be conducted to assess the effectivity of said antimicrobialsagainst zoonotic and pathogenic bacteria. It is important to perform these tests to choose the rightantimicrobial for each therapy and with that help reducing the likelihood of resistance.Susceptibility and resistance can be assessed through different methods and each laboratory determinesthe method they use that better fits their practice, for this reason at this moment in time it is difficult tocompare results between countries or regions of the world that use different antimicrobial susceptibilitymethods or breakpoints. Therefore, harmonized techniques and breakpoints along with comparability ofresults is needed to reach a higher level of antimicrobial resistance surveillance worldwide.As for in vitro methods to determine susceptibility against antimicrobials, disk agar diffusion test is one of thetwo main techniques, this method consists of disks impregnated in antibiotic used with an agar medium. Thesecond widely used in vitro method is the dilution technique in which the microorganism tested is exposedto increasing concentrations of an antibiotic in broth or agar.Disk diffusion is a relatively inexpensive, easy to use and flexible agar-based method which provides qualitativeresults for rapidly growing aerobic bacteria (Schwalbe, et al., 2007). However, very few antimicrobials haveveterinary-specific interpretive criteria for this susceptibility method, which forces practitioners to usehuman interpretive criteria for most antibiotics.The agar and broth dilution susceptibility-testing methods are used for the determination of the minimalinhibitory concentration (MIC) of an antimicrobial agent required to inhibit the growth of a microorganism(Schwalbe, et al., 2007). This method is used to measure quantitatively the in vitro activity of antimicrobials,which allows for the determination of the minimum concentration of the drug needed to inhibit or eliminatethe microorganism.In this guide we will also review commercial systems, both manual and automated focusing on the automatedMIC methods, which offer greater sensitivity with microbroth dilution and produces reproducible and accurateresults with some to full automation. See Annex 4 for a summary of all methods reviewed in this manual.Bacterial Isolation, Identificationand StorageThe first approach to susceptibility testing is bacterial isolation, along with purification and identification. Toget pure bacterial cultures the isolation process must be carried out and identification needs to take placeto begin purification. With purified cultures different aspects of bacteria strains can be studied; such asmorphology, physiology and antimicrobial susceptibility.The obtention of reliable and reproducible results falls on the use of standardized methods throughout thewhole process and having quality control within the laboratory and all the materials used. It’s important tocheck the quality of the batches of test bacteria, its media and the overall performance of the assay protocol.Pure cultures can be obtained through different methods, some of the best are solid media, streak plate andthe pour plate method. Streak plate tends to be the most practical one, in which the inoculum is placed closeto the border of the plate with agar medium and then spread on the upper part of the plate with parallelstrokes. The inoculum is also streaked on other parts of the plate to observe isolated colonies.To have a clear diagnosis and achieve effective antimicrobial treatments, identification of bacterial agentsis of importance. Different species of bacteria have distinctive morphological, physiological and biochemicalcharacteristics, identification can be accomplished by testing for such characteristics.Bacterial cultures must be stored in appropriate medium and there are different ways to do so, one of themethods is by sub-culturing or by transferring the purified culture into fresh solid medium with minimumnutrient content to prevent bacterial overgrowth. Another method is by freezing the bacterial culture,stocked in a broth medium with glycerol, which is added to prevent bacterial desiccation. (Ruangpang andTendencia, 2004).It is important to note that cultures should be properly labelled with permanent markers before storing,adding pertinent information such as sample source, date of isolation and identification.
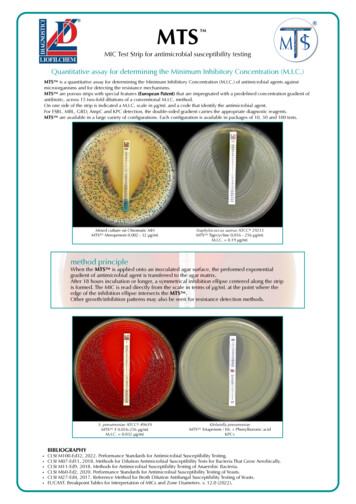
Disk Diffusion MethodHowit worksMaterialsThis method consists of inoculating the isolated bacteria onto a MuellerHinton agar plate, followed by placing antibiotic-impregnated paper diskson the surface of the agar. By incubating this plate, antibiotics will diffuseinto the agar in a gradient, the antibiotic concentration will decrease asthe distance from the disk increases. Antibiotic susceptibility is determinedby measuring the diameter of the zones of bacterial inhibition around theantibiotic disks and comparing the diameter with disk diffusion interpretivecriteria (Schwalbe, et al., 2007).3.4.5.6.See Annex 1.17.MediaMueller-Hinton agar (MHA) is preferred for this method because of itsreproducible results and its low sulfonamide, trimethoprim and tetracyclineinhibitors which gives satisfactory growth of most bacteria, but other mediasuch as MHA supplemented with blood may also be used as some bacteriahave special requirements. Tryptic soy broth or 0.9% saline solution aresuitable broths used for the inoculum of the disk diffusion method.After sterilization, check the pH of thepreparation which should be 7.2-7.4 atroom temperature.Cool the agar medium to 40-50 C.Pour the agar into a sterile petri dish toa depth of 4mm.Allow the agar to solidify.Dry plates at 30-37 C in an incubator,with its lid slightly ajar until excessmoisture has evaporated. Media mustbe free of water droplets so otherbacteria don’t contaminate the agarand get inaccurate results.Test a couple of samples fromeach batch of plates for sterility byincubating at 35 C for 24 hours orlonger. Discard these samples aftertesting.Storage1.Preparation of Agar Medium1.2.Prepare MHA medium according tomanufacturer’s instructions. Mediamust be prepared with distilled wateror deionized water.Bring to a boil agitating throughoutthe process until completely issolved.Sterilize in an autoclave at 121 C for15 minutes.Plates can be stored in a refrigeratorif they are not used shortly after theyare prepared. Plates are to be stored inairtight plastic bags or containers at2-8 C for up to 4 weeks.2.Media which has not been poured on aplate can be stored in a sealed bottleunder the conditions specified by themanufacturerControlBefore using the prepared plates, make sure the agar can support growth of control strains (such asEscherichia coli, Pseudomonas aeruginosa, Staphylococcus aureus) by streaking the cultures on the medium.
Inoculum andinoculationPreparation1.3.Inoculate the agar by streaking the swabagainst the plate.4.Rotate the plate by 60 and repeat the steptwice, for an even distribution of inoculum.From the prepared pure bacterialcultures, take 4-5 colonies with aninoculation loop.2.3.4.Transfer colonies to 5 ml of Trypticsoy broth or 0.9% saline solution5.Incubate broth or solution at 35 C (oroptimum growth temperature for bacterialstrain tested) until 0.5 McFarland standardturbidity is achieved or exceeded. Thestandardized inoculum has a concentrationof 1-2 108 CFU/ml.Compare turbidity of test bacterial suspension with0.5 standard McFarland (shaken vigorously before use)against a white background with a contrasting blackline.Note: Alternatively, turbidity can be measured with a photometric device calibratedagainst 0.5 McFarland standard according to the manufacturer’s instructions.Allow the surface to dry for 3-5 minutesbut no longer than 15 so excess moisture isabsorbed.Antimicrobial disksSelectionA limited number of antimicrobials should be tested, preferably choosing only one representative of eachgroup of drugs. Antimicrobials of veterinary use and those used for epidemiological or research purposesshould be the priority. Only use antibiotic disks purchased from reliable manufacturers, expired disks mustnot be used.To properly store disks, use airtight containers with a desiccant at 2-8 C.Inoculation of plates1.2.Within 15 minutes of adjustingturbidity, dip a sterile cotton swab intothe standardized bacterial suspensionPress the swab against the tubewall (above the fluid level) toremove excess inoculum.Application1.With the help of a sterile forceps ordisk dispenser, place antibiotic disk onthe dried plate2.Lightly press down the disk to makesure it is in contact with the surface ofthe plate. Do not move the disk once ithas been placed, since some diffusionmight happen.
3.Reading and Measuring Zones ofInhibitionPlace disks in a way that between twocenters of antibiotic disks there is atleast 24 mm, and no less than 10-15 mmfrom the edge of the plate. A maximumof 6 antibiotic disks can be placed in a 9cm petri dish. Number of disks must bereduced per plate if overlapping zones ofinhibition are found.The “zone of inhibition” is a point at which no bacterial growth is visible to an unaided eye.Reading1.Read and register the diameter ofzones of inhibition preferably using aVernier scale (or a ruler graduated to0.5 mm).Control PlateOne plate inoculated with a control strain ATCC is to be included in every batch of inoculated plates.Incubation1.2.Invert the plates and incubatethem at 35 C or at an optimumgrowth temperature for the testedmicroorganism.3.The zone of inhibition may beobserved after incubation.Incubate for 16-18 hours. Eachlaboratory must check requirementsfor the tested bacterial strain as somehave special requirements.2.Interpretation of Results1.Compare the diameter of the zoneof inhibition of the test isolates withthose of the interpretive criteria forveterinary pathogens from CLSI (seeAnnex 3).2.3.1. Antibiotic disc, 2. Agar medium, 3. Bacterial growth, 4. No bacterial growth (zone of inhibition)Round up the zone measurement tothe nearest millimeter.Report results as Resistant (R),Intermediate (I) or Susceptible (S).Example of Results Reporting:Antimicrobial agents not yetlisted with their own interpretivecriteria are to be interpreted onlyqualitatively (presence or absence ofa definite zone of inhibition) until itsinterpretative zones are established.Disk used: Chloramphenicol, 30 µg (C-30)Zone of inhibition: 16 mmResult/Interpretation: Intermediate(Note: Based on CLSI interpretive criteria)(Ruangpan and Tendencia, 2004)
Rejection Criteria1.Do not read plates which haveisolated colonies or with lessthan uniform growth.2.Do not read zones of inhibition inwhich two disks have overlapped.Minimal InhibitoryConcentration TestHow it worksThe minimal inhibitory concentration (MIC) is the lowest concentration of an antibiotic that inhibits thegrowth of a microorganism. This method can be performed on agar or liquid medium. The traditionalmethod to determine the MIC is with a broth dilution technique, in which serial dilutions of antibiotics areincorporated into the broth. Each tube or well contains a different concentration of the antimicrobial agentand is inoculated with a fixed amount of the test bacteria. After incubation, the lowest concentration thatshows no visible growth is considered the MIC. This is a quantitative test, in which the results are expressedin μg/ml (Schwalbe, et al., 2007).3.Do not read zones of inhibition whichare not circular or have distortion.4.Reject all information from a batchif the zones of inhibition from acontrol strain plate are not within theappropriate limits.The minimal inhibitory concentration (MIC) is the lowest concentration of an antibiotic thatinhibits the growth of a microorganism. This method can be performed on agar or liquid medium.The traditional method to determine the MIC is with a broth dilution technique, in which serialdilutions of antibiotics are incorporated into the broth. Each tube or well contains a differentconcentration of the antimicrobial agent and is inoculated with a fixed amount of the testbacteria. After incubation, the lowest concentration that shows no visible growth is consideredthe MIC. This is a quantitative test, in which the results are expressed in μg/ml (Schwalbe, et al.,2007).(A) Weight (mg) (Volume (ml) Concentration (μg/ml))/(Potency (μg/mg))TroubleshootingSee Annex 2.or(B) Volume (ml) (Weight (mg) Potency (μg/mg))/(Concentration (μg/ml))
MaterialsSee Annex 1.2Inoculum Preparation1.Media2.Grab 3-5 well-isolated colonies from a pureovernight bacterial culture and subculture itto a tube containing 4-5 ml of a suitable brothmedium such as tryptic soy broth.Different media can be used for the MIC test, but MHA is the preferred medium for routine susceptibilitytesting because it has good reproducibility and is low in sulfonamide, trimethoprim, and tetracyclineinhibitors, which gives an effective growth of most bacterial pathogens. (CLSI, 2005)Preparation of antimicrobial agentstock solution1.2.3.Weigh appropriate amount of thepowdered antimicrobial agent.4.Prepare intermediate (10x)antimicrobial agent solutions bymaking successive (two-fold) 1:2, 1:4,and 1:8 dilutions into sterile diluent.Dissolve antimicrobial agentpowder in solvent as indicated bymanufacturer to make a concentrationof at least 1,000 μg/ml or at least 10times the highest concentration to betested.Dispense small volumes of thesterile stock solutions into sterileglass, polypropylene, polystyrene, orpolyethylene vials. Carefully seal andstore preferably at 60 C or below.Note: Vials may be thawed and usedthe same day. Any unused stocksolution should be discarded at theend of the day.5.Set aside for now.3.Incubate the broth culture at 35 2 C until itachieves or exceeds a McFarland turbidity of 0.5Adjust turbidity of the inoculum with sterilesaline or broth to achieve a turbidity of a 0.5McFarland standard. Use a photometric deviceor adequate light to compare the inoculumtube and the 0.5 McFarland standard against apaper with white background and contrastingblack lines.Note: this results in a suspension containingapproximately 1-2 108 CFU/ml.
Agar DilutionIn this technique, antimicrobial agents are incorporated into the agar medium with each different platecontaining different concentrations of the drug. The inoculum can be applied effortlessly with an inoculatoror manually.Preparation of AntimicrobialAgar Plates1.2.3.4.5.6.Label each empty plate to be able toidentify the antimicrobial agents and theirconcentrations.InoculationDilution of Inoculum SuspensionCultures adjusted to the 0.5 McFarland standard contain approximately 1-2 x 108 CFU/ml with most species,and the final inoculum required for a 5-8 mm spot is 104 CFU/spot.»When using replicators with 3 mm pins that deliver 2 μl, dilute the 0.5 McFarland suspension1:10 in sterile broth or saline to obtain a concentration of 107 CFU/ml which will give a finalinoculum on the agar of approximately 104 CFU per spot.»When using replicators with 1 mm pins that deliver 0.1-0.2 μl, do not dilute the initialsuspension.»When doing manual inoculation dilute the 0.5 McFarland suspension 1:10 in sterile broth orsaline and deliver 10 μl of the suspension.Plan on a reference paper the arrangement ofnumbered bacterial strains, which will be usedto read the results later.Prepare MHA medium according tomanufacturer’s instructions, keep it in a waterbath at 45-50 C until used.SequenceThe first plate to inoculate must be the control plates, to avoid contamination of the plates withantimicrobial agents. It is important to include the drug-free plate at the beginning of the inoculationprocess.Add appropriate dilutions of antimicrobialsolution (previously prepared in “Preparationof antimicrobial agent stock solution”) tomolten test agars.1.Mix the agar and antimicrobial solutionthoroughly and pour into Petri dishes on alevel surface to result in an agar depth of 3 to4 mm.2.Allow the agar to solidify at room temperatureand use the plates immediately after the agarsurface has dried completely, avoid excessivedrying.Note: use the plates either immediately orstore them in sealed plastic bags at 2-8 C forup to five days for reference work, or longer forroutine tests.Arrange the tubes containing the adjusted anddiluted bacterial suspensions (107 CFU/ml) inorder in a rack.On a fully dried agar plate inoculate thespecified amount described on “Dilutionof Inoculum suspension”, with an inoculumreplication device or standardized loops orpipettes.Note: final concentration of spots should be104 CFU/spot.3.Allow the inoculum to be absorbedinto the agar before incubation.
Control Agar PlatesAntibiotic free plate: pipette MHA into a sterile petri dish, without any antimicrobial agent.Growth-control plate: Inoculate a growth-control plate (no antimicrobial agent).Mixed cultures plate: streak a sample of each inoculum on a suitable non-selective agar plate and incubateovernight to detect mixed cultures.Allow the inoculated plates to rest at roomtemperature until no moisture from theinoculum is visible or until all spots are dry.Place the agar plates on a non-reflectiveblack surface and observe bacterial growthwithout visual aids. Use the reference paperpreviously made on Step 2 of “Preparationof Antimicrobial Agar Plates” to locate theposition of the test bacteria.2.Incubation1.Reading MIC Values1.2.Incubate the plates in an inverted positionat 35 2 C for 16-20 hours (or for longer,depending on the tested microorganism).Note: do not incubate the plates in anatmosphere with increased CO2 when testingnon-fastidious organisms as the surface pHmay be altered.3.4.5.Control StrainsWhen testing samples, the corresponding QC organism should be tested concurrently. To consider a resultvalid, the MIC of the QC organism must fall within the acceptable ranges for quality control strains stated inthe CLSI guidelines.Check bacterial growth on the control plates,reject results if no growth is detected in somecontrol plates as the test must be repeated.Register the MIC (lowest concentration ofantibiotic that completely inhibits bacterialgrowth) detected without visual aid.Compare the MIC breakpoint of the testisolates with those of the interpretive criteriafor veterinary pathogens from CLSI (see Annex3).Report result as Resistant (R), Intermediate (I)or Susceptible (S).Example:Antibiotic: OxytetracyclineMIC breakpoint: 0.2 μg/mLInterpretation: Susceptible(Ruangpan and Tendencia, 2004)
Broth MicrodilutionControlPreparing and Storing DilutedAntimicrobial Agents1.Inoculum and Inoculation1.3.This method involves the use of small volumes, hence the name “microdilution”. The broth is dispensed insterile plastic microdilution trays for which each well should contain 0.1 ml of broth.Make intermediate two-fold dilutions ofantimicrobial agent volumetrically in brothor sterile water.Note: use one pipette for measuring alldiluents and then for adding the stockantimicrobial solution to the first tube. Foreach subsequent dilution step, use a newpipette.2.3.Prepare a standardized inoculum as directedin “Inoculum Preparation”2.Within 15 min of preparation, dilute coloniesin broth, water or saline so after inoculation,each well contains approximately 5 105 CFU/ml (2-8 105 CFU/ml)Note: the dilution procedure to obtain thisfinal inoculum varies according to the methodof delivery of the inoculum to the individualwells and it must be calculated for eachsituation.Within 15 minutes of inoculumstandardization, inoculate each well of amicrodilution tray.»Inoculator device: use it so it delivers avolume that does not exceed 10% of thevolume in the well (e.g., 10 μl of inoculumin 0.1 ml antimicrobial agent solution).»Micropipette: if a 0.05 ml pipette is used,it results in a 1:2 dilution of the contentsof each well (containing 0.05 ml).Dispense the antimicrobial-broth solutionsinto the plastic microdilution trays.Use a multichannel pipette for preparingmicrodilution trays as it is the mostconvenient method. Antimicrobial dilutionsmade in at least 10 ml of broth should beused.Note: the dispensing device then delivers0.1 ( 0.02) ml into each of the 96 wells of astandard tray4.Each tray should include a growth control well and a sterility (uninoculated) well.Compare the MIC breakpoint of the test isolateswith those of the interpretive criteria forveterinary pathogens from CLSI (see Annex 3).Example: If the volume of broth in the wellis 0.1 ml and the inoculum volume is 0.01ml, then the 0.5 McFarland suspension(1 108 CFU/ml) should be diluted 1:20 toyield 5 106 CFU/ml. When 0.01 ml of thissuspension is inoculated into the broth,the final test concentration of bacteriawill be 5 105 CFU/ml approximately (or5 104 CFU/well)4.Perform a purity check of the inoculumsuspension by subculturing an aliquot onto anonselective agar plate for incubation.IncubationIncubate the inoculated microdilution trays within 15 minutes of adding the inoculum at 35 2 C for 16 to20 hours in an ambient air incubator (or more depending on needs of the microorganism).Note: to maintain the same incubation temperature for all cultures, do not stack more than four microdilutiontrays.
Control Strains:When testing samples, the corresponding QC organism should be tested concurrently. To consider a resultvalid, the MIC of the QC organism must fall within the acceptable ranges for quality control strains stated inthe CLSI guidelines.Reading MIC Values1.2.3.Wells containing QC strains must bechecked to ensure their MIC values arewithin acceptable rangesCompare the MIC breakpoint of the testisolates with those of the interpretive criteriafor veterinary pathogens from CLSI (see Annex3).Antibiotic-free wells must be checked toensure bacterial growth is present.Broth control wells must remain clear (nogrowth).Note: growth in this well is an indicative ofcontamination, if growth is found the testmust be repeated as its results are invalid.4.5.Compare wells with the negative controlincluded in the test, the MIC is detected whenthere is lack of visual turbidity, matching thenegative control. A spectrophotometer can alsobe used.6.Report result as Resistant (R), Intermediate (I) orSusceptible (S).Example:Antibiotic: OxytetracyclineMIC breakpoint: 0.2 µg/mlInterpretation: Susceptible(Ruangpan and Tendencia, 2004)COMMERCIAL SYSTEMSThe FDA in its “Guidance and Review Criteria for Assessment of Antimicrobial Susceptibility Devices” describesthe requirements to be met by manufacturers of susceptibility test systems to become “FDA-cleared”. Therequirements are comparable results to those of CLSI reference methods, overall performance meeting theFDA criteria and the ability of the system to be monitored in the laboratory following the recommendedquality control procedures. In this chapter we will review the most widely used commercial systems.Manual SystemsE test The E-test consists of a nonporous plastic strip immobilizedwith a predefined gradient of a given antimicrobial agenton one side and a printed MIC scale on the other side. Thestability of the gradient is maintained for up to 18 to 20 hours,which covers the critical times of a wide range of pathogens,from rapid growing aerobic bacteria to slow growing fastidiousorganisms, including anaerobes. When placed on an inoculatedagar plate, a continuous antimicrobial gradient is establishedalong the side of the strip. After incubating, the MIC value(µg/ml) can be read from the MIC scale printed on the strip.(Schwalbe, et al., 2007)Advantages: Easy to perform and requires minimal training for optimal test performance.Contamination can be easily recognized.Minimum labour involved, compared to broth dilution methods.Flexible methodology (antimicrobial agent, media, incubation time and inoculum size can beadjusted depending on the microorganism tested).E-test can be easily set up for a small number of clinical isolates.Limitations: The main limitation is its cost.
Automated Broth MicrodilutionSystemsInstrumentalization helps laboratories standardize end points and generally produce results faster thanmanual AST methods. The FDA has approved a limited amount of automated antimicrobial susceptibilitysystems, which provide semi-automation to full-automation depending on the system and results withinshort term incubations ( 16 hours) to overnight incubation. System manufacturers offer different settings fortheir instruments in terms of panels and panel capacity, system specific features and specialized softwarewhich enable laboratories to analyze data with ease or report results faster.The advantages of automated AST systems include reduced labour time, reproducibility, data managementwith analytical software, and generating results rapidly.Effective communication of the results to clinicians and pharmacists is essential to maximize the benefitsof rapid testing.VITEK Systems (Classic, VITEK 2 )Instrumentalization helps laboratories standardize end points and generally produce results faster thanmanual AST methods. The FDA has approved a limited amount of automated antimicrobial susceptibilitysystems, which provide semi-automation to full-automation depending on the system and results withinshort term incubations ( 16 hours) to overnight incubation. System manufacturers offer different settings fortheir instruments in terms of panels and panel capacity, system specific features and specialized softwarewhich enable laboratories to analyze data with ease or report results faster.The advantages of automated AST systems include reduced labour time, reproducibility, data managementwith analytical software, and generating results rapidly.Effective communication of the results to clinicians and pharmacists is essential to maximize the benefitsof rapid testing.MicroScan WalkAway This system developed by Siemens consists of two major type of AST panels, conventional panels whichread turbidimetrically after overnight incubation and rapid panels that read fluorometrically after 3.5-15h of incubation. The panels are conventional 96-well microdilution trays which include MIC panels, MICcombination panels (some wells used for identification) and breakpoint combination panels which are foridentification with a limited range of antimicrobial agent dilutions for qualitative results of susceptible,intermediate or resistant.MicroScan comes with a data management computer and software that can be used to interpret, store andreport data.Becton Dickinson Phoenix BD Phoenix is a fully automated susceptibility testing system; which uses chromogenic and fluorogenicsubstrates in the same panel. This system holds up to 100 panels that contain 136 wells, using standardizedinoculums, panels are manually inoculated and placed in the instrument for incubation and reading. Thepanels are read every 20 minutes until testin
The agar and broth dilution susceptibility-testing methods are used for the determination of the minimal inhibitory concentration (MIC) of an antimicrobial agent required to inhibit the growth of a microorganism (Schwalbe, et al., 2007). This method is used to measur