Transcription
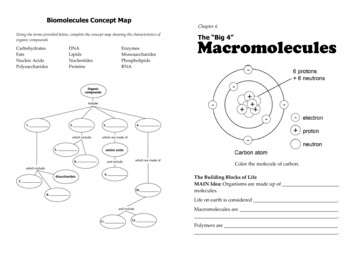
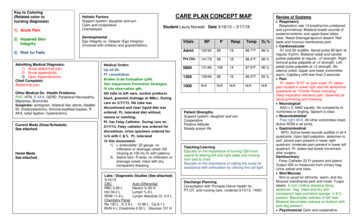
Key to Coloring(Related color tonursing diagnosis)1) Acute PainHolistic FactorsSupport system- daughter and sonCalm and cooperativeUnemployed2) Impaired SkinIntegrityDevelopmentalEgo Integrity vs. Despair (Ego Integrity)(Involved with children and grandchildren)CARE PLAN CONCEPT MAPStudent Laura Norwalt Date 3/16/13 – 3/17/183) Risk for FallsAdmitting Medical Diagnosis:1) Acute abdominal pain2) Acute appendicitis3) Open AppendectomyChief Complaint:Abdominal painOther Medical Dx. /Health Problems:PVD, HTN, R AKA, GERD, Peripheral Neuropathy,Migraines, BronchitisSurgeries: aortogram, bilateral iliac stents, bladderlift, cholecystectomy, femoral popliteal bypass, RAKA, tubal ligation, hysterectomyCurrent Meds (Dose/Schedule)See attached.HomeMedsSurgicalHistory:See attached.Review of SystemsMedical OrdersUp ad lib.PT consultation.Braden Scale Evaluation q24h.Skin Impairment Prevention Strategies.IV site observation q4h.NG tube to left nare, suction producesblack, greenish drainage at 400cc. Duringcare on 3/17/13, NG tube wasdiscontinued and clear liquid diet wasordered. Pt. tolerated diet withoutnausea or vomiting.Pt. has Foley Catheter. During care on3/17/13, Foley catheter was ordered fordiscontinue. Urine specimen ordered forU/A with C & S. Pt. tolerateddiscontinuationwell.IV Site Assessment:1) L antecubital- 22 gauge, noinfiltration or drainage noted; NSinfusing at 100 mL/hr with patency2) Saline lock- R wrist, no infiltration ordrainage noted; intact with dry,transparent dressingLabs / Diagnostic Studies (See attached)3/15/13CBCAuto DifferentialRBC 3.59 LNeutro % 83 HHct 34.2 LLymph % 8 LRDW 11.9 LLymph Absolute Ct. 0.4 LChemistry PanelNa 130 L K 2.9 L Cl 96 L Ca 8.1 LBUN 4 L Creatinine 0.52 L Glucose 157 HVitalsBPPAdmit152/9288Pre Clin.141/790800RespTempO2 %1898.7 F98 %961898.4 F98 %131/661081497.9 F96 %1200136/69881698.3 F95 %1600N/AN/AN/AN/AN/APatient StrengthsSupport system- daughter and sonCooperativePositive AttitudeSteady prayer lifeTeaching/LearningEducate on the importance of turning Q2H fromsupine to altering left and right sides and movingfrom bed to chair.Educate on the importance of calling the nurse forassistance with ambulation by utilizing the call light.Discharge PlanningConsultation with Pinnacle Home Health forPT,OT, and nursing care. (ordered 3/15/13- 1400) RespiratoryRespiration rate 14 breaths/min,unlaboredand symmetrical. Bilateral breath sounds ofposterior/anterior and upper/lower lobesclear. Nasal drainage/sputum absent. Nailbeds and mucous membranes pink. CardiovascularS1 and S2 audible. Apical pulse 80 bpm atregular rhythm. Bilateral radial and carotidpulses palpable at regular, 2 strength. Rightfemoral pulse palpable at 2 strength. Leftpedal pulse palpable at 2 strength. Noedema noted. Upper and lower extremitieswarm. Capillary refill less than 3 seconds. PainPt. states “9/10” on pain scale. Pt. statespain located in lower right and left abdominalquadrants as “Charlie Horse cramping.”Deep inspiration worsens pain, observed asfacial grimacing and frowning. NeurologicalAAO x 3. MAE equally. No complaints ofnumbness or tingling. Speech is clear. MusculoskeletalPast right AKA. All other extremities intact.Active ROM in all joints. GastrointestinalNPO. Active bowel sounds audible in all 4quadrants. Upon light palpation, abdomen issoft, severe pain present in lower rightquadrant, moderate pain present in lower leftquadrant. Pt. states last bowel movementafter surgery.GenitourinaryFoley Catheter 22 Fr present and patent.Output 500 cc measured from urinary bag.Urine yellow and clear. Skin/MucosaSkin is usual for ethnicity, warm, and dry.Mucous membranes pink and moist. Turgorelastic. 6 inch midline dressing alongabdomen. Dsg. intact and dry withtransparent tape and black sponge. V.A.C.present. Blanchable redness of left heel.Bilateral blanchable redness on buttock withpink dsg present. Psychosocial Calm and cooperative.
History of Present Illness: Pt. presented to ER on 3/13/13 with acute abdominal pain. Cat scan was performed of abdomen and pelvis with oral and IV contrast. Diagnostic imaging confirmed acuteappendicitis diagnosis. Procedures performed include exploratory laparotomy, lysis of adhesions, appendectomy, washout closure of abdomen, and wound V.A.C. placement. Pt. is stable, NPO, and in pain.Nursing ProblemsNursing Care/InterventionsRationaleExpected Outcomes1) Acute pain related to tissuedamage secondary to surgicalintervention AEB pt. states “9/10”on pain scale that is described as“Charlie horse cramps” ofabdomen.1) Administer morphine as needed based on patient’sstated pain level on pain scale. Nurse will follow – upwithin one hour of morphine administration.- Rationale: pain medication acts on opioidreceptors to decrease pain impulse; appropriatedosage is needed for stated pain level on painscale2) Cluster nursing tasks together, such as medicationadministration, vital signs, and bathing, to promoterest and relaxation for patient throughout shift.- Rationale: By clustering tasks together, this allowsthe patient to have long periods where she can tryto fall asleep.3) Promote comfort measures, such as prayer andvisitation from son, 2 daughters, and grandchildthroughout shift.- Rationale: Positive support system allows thepatient to focus on her family which may decreaseher perception of pain. Positive support systemalso promotes healthy healing.Rationale Reference: Ackley 600-6051) One hour after morphine administration,patient will state less than a 7/10 on thepain scale.2) Pt. will report taking a restful half hournap before 1200.Pt. stated “7 out of 10” on pain scale after morphineadministration.Pt. stated “took a 20 minute nap” at 1000.1) Educate the patient on the importance of turning Q2Hfrom supine to altering left and right sides during shift.The nurse will be available to assist in turning Q2H.- Rationale: By changing the patient’s position, thisremoves continuously pressure on these siteswhich will prevent development of pressureulcers. By educating the patient on the reasoningbehind activities, this allows her to be part of herown care.2) Monitor reddened areas for blanching q4h during shift.- Rationale: The development of pressure ulcers isprominent in populations who have limitedmobility. When redness becomes non-blanchable,this sign indicates stage I of a pressure ulcerdevelopment.1) Patient’s reddened areas on bilateralbuttocks and left heel will remainblanchable and free of further skinbreakdown during shift.2) After teaching session, patient will state2 reasons for the importance of turningq2h and getting up into chair at leastonce per day.3) Patient will sit up in chair at least onceduring 8 hour shift.Patient’s redness areas on buttocks and left heelremain free of further skin breakdown and futurecomplications during shift.Patient stated 2 important reasons for turning andmoving from bed into chair, “doesn’t want to get apressure ulcer and wants to relieve heel.”At 1100, patient sat up in chair for one hour duringshift.2) Impaired skin integrity related tolimited mobility and prolonged bedrest AEB bilateral blanchableredness of both buttocks and leftheel blanchable redness.Evaluation
Nursing ProblemsNursing Care/InterventionsRationaleExpected OutcomesEvaluation3) Encourage the patient to sit up in chair at least twice aday under physician’s order of up ad lib during shift.- Rationale: When pt. is sitting up in chair with legsup, this removes pressure on the left heel.Rationale Reference: Ackley 7703) Risk for falls related to side effectsof opioid analgesic (morphine) andlimited gait (right AKA) AEB pt.appears drowsy and needsmoderate assistance duringambulation from bed to chair.1) Keep call light in reach of patient, bed rails up x2, and 1) After teaching session on safety, patientbed in lowest position throughout shift.will state 2 situations in which she should- Rationale: These safety measures prevent fallscall the nurse or CNA for assistance.that could easily be prevented by rolling out of2) Patient will remain free of falls during 8bed.hour shift.2) Place a bedside commode next to patient’s bed forvoiding during shift.- Rationale: The placement of the bedsidecommode prevents a fall that could result from thepatient trying to ambulate to the restroom.3) Educate the patient on the importance of calling thenurse for assistance with ambulation by utilizing thecall light during shift.- Rationale: By having the nurse or CNA present forambulation, the patient is less likely to experiencea fall.Rationale Reference: Ackley 355Patient stated she would call the nurse when sheneeded to void and when she moved from bed tochair.Patient remained free of falls during 8 hour shift.
Medical DiagnosisPathophysiologyClinicalManifestations1) PVD ( Gould 310)-Refers to anyabnormality in thearteries or veinsoutside of the heart;due to atherosclerosisoccurring in arteries orveins resulting in anartheroma that obstructblood flow ultimatelyleading to hypoxia andtissue death2) HTN (Gould 308)-Increase in bloodpressure in thearteries; greater than orequal to 140/90 mmHg3) Peripheral Neuropathy (Gould556)4) Right AKA (Gould 667)--Degeneration occursin both unmyelinatedand myelinatednerve fibersRemoval of right lowerextremity from foot tomid-thigh; as a result ofPVD-Diagnostic StudiesComplicationsIncreasing fatigue,intermittent claudication(leg pain), sensoryimpairment (tingling,burning, and numbness),peripheral pulses distalto occlusion may beweak or absent;appearance of skin andfeet and legs- pallor orcyanosis, dry andhairless, toenails thickand hard, poorlyperfused areas of thelegs or feet feel coldRarely with symptoms;may have headaches,lightheadedness, vertigo,tinnitus, changes invision-Doppler studies and arteriography;plethysmography measures size oflimbs and blood volume in organs ortissues-Amputation, gangrenous ulcers, frequentinfections-Measurement of blood pressurethrough sphygmomanometer-MI, CVA, aneurysm, heart failure, kidneydisease, metabolic syndromeImpaired sensation,numbness, tingling,weakness, musclewasting-CT scan, MRI, blood test (vitamin andblood sugar; function of thyroid, liver,and kidney), electromyography, nervebiopsy-tissue trauma, infection
5) GERD (Gastroesophageal refluxdisease) (Gould 398)-6) Osteoarthritis (Gould 180)7) Migraines (Gould 207)--Periodic flow of gastric contents into theesophagus due todecrease in loweresophageal sphincteror an increase in intraabdominal pressureDegeneration ofarticular cartilage injoints; cartilagebecomes thin anderosion occur whichimpairs jointmovement and causepainAbnormal changes inblood flow andmetabolism in thebrain; proposedreactions:- increase neuralactivity spreadsover areas of thebrain initiating painstimuli in thetrigeminal system,which are thenconducted to thethalamus and paincenters in thesensory cortex- reduction inserotonin that maycause the releaseof neuropeptide,which travel tomeninges coveringthe brain- neuropeptides acton the smoothmuscle of theblood vessels inthe meninges,causing stretchingand inflammationheartburn (burningsensation in the chest),chest pain, dysphagia,dry cough, hoarseness,regurgitation, sensationof lump in the throatpain, swelling, stiffness,loss of flexibility, gratingsensation, bone spursdescribed as throbbingand severe pain;dizziness, nausea,abdominal discomfort,fatigue-X- ray of upper digestive system,ambulatory acid (pH) probe test,endoscopy-Inflammation and ulceration of mucosathat can lead to fibrosis and stricture in theesophagus-X-ray, MRI-Immobilization due to pain and stiffness-CT scan, MRI, lumbar puncture (ifsuspect meningitis)-If take OTC medications such as ibuprofencan result in abdominal problems (pain,bleeding and ulcers), rebound headaches(if used over long period of time),serotonin syndrome (take migrainemedication triptans with antidepressants)
Teaching Learning eaching StrategiesPatient has blanchable redness onAfter teaching session, pt. will state 2Information on risk for pressure ulcerTaught son about how to assistbilateral buttocks and left heel. Pt. hasreasons for the importance of turningdevelopment.with turning side to side by usingsupportive device to left heel. Pt. hasand moving from bed to chair.foam mobilizer and using bed rails.dry, intact pink dsg. on bilateral buttocks.Pt. will move from bed to chair at leastTaught patient about the risk forShe has a past right AKA and has limitedonce during 8 hour shift.pressure ulcer development.mobility. She states “bruised feeling” onDuring shift, pt. will turn Q2H fromleft heel. Pt. is ordered to turn Q2H andsupine to altering left and right sidesup ad lib. Son or daughter stays atwith or without nurse assistance.bedside throughout two 8 hour shifts.Pt. will continue to have blanchableredness of left heel and bilateralbuttocks during 8 hour shift.EvaluationPatient stated 2 important reasonsfor turning and moving from bedinto chair, “doesn’t want to get apressure ulcer and wants relieffrom heel.”At 1100, pt. sat up in chair for onehour during shift.Patient’s redness areas onbuttocks and left heel remain freeof further skin breakdown andfuture complications during shift.
Medications SheetMedication, Dose, Route,Classification and ActionFrequencyRational for AdministrationMajor Side EffectsNursing Implications(Explain why the patient isreceiving the medication)H2 histamine receptor1) Famotidine- 200mg 2 mL, IVpush, sol, Q12H(Skidmore-Roth 515)GERDantagonistMOA- competitively inhibitsheadache, dizziness, seizures,dysthymias, QT prolongation,constipation, thrombocytopenia,aplastic anemia, pneumoniahistamine at H2 receptor site,thus decreasing gastricAssess for ulcers, pH, blood counts( watchfor low platelets), bleeding, hematuria, blooddyscrasisPerform and Provide – cool environment,increase bulk and fluids in diet to preventconstipation, evaluate therapeutic responsesecretion while pepsin remainsTeach- don’t double dose, report bleeding,brui
CARE PLAN CONCEPT MAP nursing diagnosis) Respiration Student Laura Norwalt Date 3/16/13 – 3/17/18 clear. Nasal drain Admit Up ad lib car lift, Pt. has Foley Catheter. During care on Foley Catheter Chemistry Panel Key to Coloring (Related color to 1) Acute File Size: 260KBPage Count: 13