Transcription
TEXAS MEDICAID MANAGED CAREQUALITY STRATEGY2012 - 2016
CONTENTSI.INTRODUCTION . 3A.Background . 3B.Texas Health Care Transformation and Quality Improvement Program . 3C.Managed Care Program Goals and Objectives . 5STAR and STAR PLUS Program Objectives . 5Medicaid Dental Program Objectives . 7D.Managed Care Program Management Strategy . 7E.External Quality Review Organization . 8II.ASSESSMENT. 8A.Quality and Appropriateness of Care and Services . 8Race/Ethnicity, and Primary Language . 9HHSC Overarching Goals and Performance Improvement Projects . 9Performance Indicator Dashboards for Quality Measures . 9Quality Assessment and Performance Improvement (QAPI) . 9Clinical Practice Guidelines . 10Encounter Data . 10Evidence-Based Care and Quality Measurement . 10B.Level of MCO Contract Compliance. 11Access to Care . 11Provider Network . 11Service Coordination for STAR PLUS . 12Continuity of Care for STAR and STAR PLUS . 12Utilization Management. 12Member Complaint and Appeal Process . 13Provider Complaints and Appeals . 13Encounter Data Requirements. 13Health Plan Management . 14Provider Incentives . 14Performance Based At-Risk Capitation and Quality Challenge Award . 15
Texas Medicaid Managed Care Quality StrategyQuality Assessment and Performance Improvement (QAPI) . 17MCO Administrator Tool . 17C.III.A.MCO Monitoring . 18IMPROVEMENT. 18Initiatives . 18Potentially Preventable Events Report Series . 18Texas Healthcare Learning Collaborative Initiative . 18Use of Quality Metrics across Delivery Systems . 19Assessment of Member Experiences with Their Medical Homes . 19Dual Eligible STAR PLUS Focus Study . 20Rider 50 Initiative: Behavioral Health Quality of Care . 20Senate Bill 7 Initiative: Quality-Based Premium Payments and Performance. 21First Dental Home Initiative . 21STAR PLUS Home and Community-Based Services (HCBS) Program . 22Money Follows the Person . 23Money Follows the Person Demonstration Initiative . 23B.IV.Evaluation . 24REVIEW OF QUALITY STRATEGY . 24A.MCO Reporting Requirements . 24B.EQRO Reporting Requirements . 24C.CMS Reporting Requirements . 24V.ACHIEVEMENTS AND OPPORTUNITIES . 24A.Potentially Preventable Events. 24Potentially Preventable Admissions (PPAs) . 24Potentially Preventable Readmissions (PPRs). 25Potentially Preventable Emergency Department Visits (PPVs). 26B.Patient-Centered Medical Homes . 27C.Medicaid Incentives for Prevention of Chronic Disease Project . 272
Texas Medicaid Managed Care Quality StrategyI.INTRODUCTIONA.BackgroundIn response to rising health care costs and national interest in cost effective ways to providequality health care, the Texas Legislature in 1991 directed the state to establish Medicaidmanaged care pilot programs in Travis County and the Gulf Coast area. These pilots were initiallyknown as the LoneSTAR (State of Texas Access Reform) Health Initiative. Later shortened toSTAR, it is the primary managed care program serving low-income families, non-disabledchildren, and pregnant women in Texas. In 1995, Texas lawmakers authorized the Health andHuman Services Commission (HHSC) to seek an 1115 waiver to fundamentally restructureMedicaid service delivery and funding in Texas. At that time the STAR Program was expanded toinclude certain blind and disabled Medicaid clients (SSI/SSI-related) on a voluntary basis whenthe expansion occurred.As Texas gained more experience with managed care, the state implemented STAR PLUS in1998. The program began as a pilot project in Harris County to integrate acute and long-termservices and supports for clients who are age 65 and older or have disabilities. The goal was toaddress the complex needs of these populations in a more coordinated, comprehensive manner,thus resulting in both increased quality of care and decreased Medicaid costs. A year later in1999, the state implemented a mental health and substance abuse program called NorthSTAR inthe Dallas service area that integrates funding and delivery of services to Medicaid and indigentclients, providing a continuum of care across public funding sources.In 2005, the Texas Legislature directed HHSC and the Department of Family and ProtectiveServices (DFPS) to develop a statewide health care delivery model for children in foster care.This program, known as STAR Health, became operational in 2008 and was designed to providecomprehensive, cost-effective medical services to meet the physical and behavioral health needsof the Texas foster care and kinship population.B.Texas Health Care Transformation and Quality ImprovementProgramThe Texas Legislature, through the 2012-2013 General Appropriations Act and Senate Bill 7,instructed HHSC to expand its use of risk-based Medicaid managed care to achieve programsavings, while also preserving locally funded supplemental payments to hospitals. The State ofTexas submitted a section 1115 Demonstration proposal to CMS in July 2011 to expand managedcare statewide consistent with the existing STAR section 1915(b) and STAR PLUS section1915(b)/(c) waiver programs, and thereby replace existing Primary Care Case Management(PCCM) or fee-for-service (FFS) delivery systems. The State sought a section 1115 Demonstrationas the vehicle to both expand the managed care delivery system and to operate a funding pool,supported by managed care savings and diverted supplemental payments, to reimburseproviders for uncompensated care costs and to provide incentive payments to participatinghospitals that implement and operate delivery system reforms.The 1115 Demonstration sought managed care organizations (MCOs) to operate the STAR andSTAR PLUS in service areas throughout the state (the “joint procurement”). The jointprocurement did not include the STAR PLUS Dallas and Tarrant service areas or the CHIP ruralservice area. These areas operate under separate agreements with MCOs. The jointprocurement included two major changes to Medicaid managed care. First, it expanded STAR toall service areas in the State, and STAR PLUS to all areas except the Medicaid Rural Service Area(MRSA). The joint procurement also carved outpatient pharmacy benefits into managed care.HHSC awarded a total of 21 contracts to Medicaid MCOs with a September 1, 2011 effective date3
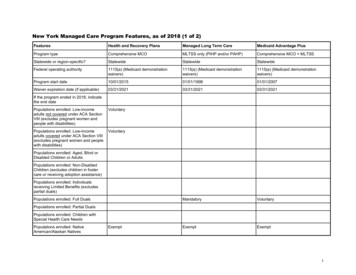
Texas Medicaid Managed Care Quality Strategyand March 1, 2012 operational start date. For consistency across service areas, the State alsoamended its MCO agreements for the STAR PLUS Dallas and Tarrant service areas to includeoutpatient pharmacy benefits, also effective March 1, 2012. Table 1 below lists the MCOsawarded STAR and STAR PLUS managed care contracts by service area.Table 1. MCOs by Service Area and ProgramServiceSTARAreaBexarAetna Better HealthAmerigroup TexasCommunity First Health PlansSuperior HealthPlanDallasAmerigroup TexasMolina Healthcare of TexasParkland Comm. Health PlanEl PasoEl Paso First Health PlanMolina Healthcare of TexasSuperior HealthPlanHarrisAmerigroup TexasCommunity Health ChoiceMolina Healthcare of TexasTexas Children’s Health PlanUnitedHealthcare Community PlanHidalgoDriscoll Children’s Health PlanMolina Healthcare of TexasSuperior HealthPlan NetworkUnitedHealthcare Community PlanJefferson Amerigroup TexasCommunity Health ChoiceMolina Healthcare of TexasTexas Children’s Health PlanUnitedHealthcare Community PlanLubbockAmerigroup TexasFirstCare HealthPlansSuperior HealthPlanMRSAAmerigroup Ins. Co.CentralScott & White Health PlanSuperior HealthPlan NetworkMRSAAmerigroup Ins. Co.Northeast Superior HealthPlan NetworkMRSAAmerigroup Ins. Co.WestFirstCare HealthPlansSuperior HealthPlan NetworkNuecesCHRISTUS Health PlanDriscoll Children’s Health PlanSuperior HealthPlanTarrantAetna Better HealthAmerigroup TexasCook Children’s Health PlanSTAR PLUSAmerigroup TexasMolina Healthcare of TexasSuperior HealthPlanMolina Healthcare of TexasSuperior HealthPlanAmerigroup TexasMolina Healthcare of TexasAmerigroup TexasMolina Healthcare of TexasUnitedHealthcare Community PlanHealthSpring Life & Health Ins. Co.Molina Healthcare of TexasSuperior HealthPlanAmerigroup TexasMolina Healthcare of TexasUnitedHealthcare Community PlanAmerigroup TexasSuperior HealthPlanN/AN/AN/ASuperior HealthPlanUnitedHealthcare Community PlanAmerigroup TexasHealthSpring Life & Health Ins.4
Texas Medicaid Managed Care Quality StrategyTravisHealth Care Services Corp./BCBSSendero Health PlansSeton Health PlanSuperior HealthPlanAmerigroup TexasUnitedHealthcare Community PlanHHSC also expanded managed care dental services to Medicaid beneficiaries under the age of 21.The goal was to provide quality, comprehensive dental services to eligible recipients in a mannerthat improves the oral health of members through preventative care and health education.HHSC awarded three statewide contracts to the following dental maintenance organizations(DMOs):Delta Dental Insurance CompanyDentaQuest USA Insurance Company, Inc.MCNA Insurance CompanyThe contracts have a September 1, 2011, effective date and March 1, 2012, operational startdate. Although CHIP dental services were provided through managed care prior to March 1,2012, the award marked the first time Medicaid dental services would be provided through acapitated model.Through this Medicaid Demonstration, the State aims to:Expand risk-based managed care statewide.Support the development and maintenance of a coordinated care delivery system.Improve outcomes while containing cost growth.Protect and leverage financing to improve and prepare the health care infrastructure toserve a newly insured population.Transition to quality-based payment systems across managed care and hospitals.C.Managed Care Program Goals and ObjectivesHHSC’s mission is to create a customer-centered, innovative, and adaptable managed caresystem that provides the highest quality of care to clients while at the same time ensures accessto services. HHSC seeks to accomplish its mission by contracting for measurable results that:Improve member access, satisfaction, and quality of care.Maximize program efficiency, effectiveness, and responsiveness.Limit operational costs.STAR and STAR PLUS Program ObjectivesUnder the terms of the STAR and STAR PLUS managed care contracts, MCOs providecomprehensive health care services to qualified Medicaid recipients through a managed caredelivery system. HHSC prioritizes desired outcomes and benefits for the managed careprograms and focuses its monitoring efforts on the MCOs’ ability to provide satisfactory results inthe following areas.1. Network adequacy and access to careAll members must have timely access to quality of care through a network of providers designedto meet the needs of the population served. The MCO is held accountable for creating andmaintaining a network capable of delivering all covered services to members. The MCO mustprovide members with access to qualified network providers within the travel distance andwaiting time for appointment standards defined in the managed care contracts2. Quality5
Texas Medicaid Managed Care Quality StrategyHHSC is accountable to Texans for ensuring that all members receive quality services in the mostefficient and effective manner possible. Accordingly, the MCO is responsible for providing highquality services in a professional and ethical manner. HHSC expects the MCO to implement newand creative approaches that ensure quality services, cost-effective service delivery, and carefulstewardship of public resources.3. Timeliness of claim paymentThe MCO’s ability to ensure that network providers receive timely and fair payment for servicesrendered is a key component of their success in the STAR and STAR PLUS programs. The MCOmust have the ability to comply with HHSC’s claims adjudication requirements in a timelymanner. Therefore, HHSC requires strict adherence to claims adjudication standards during theterm of the Contract. HHSC also encourages MCOs to provide a no-cost alternative for providersto allow billing without the use of a clearinghouse and to include attendant care payments aspart of the regular claims payment process.4. Timeliness with which prenatal care is initiatedSTAR Program data has revealed that 83% of pregnant women received prenatal care in the firsttrimester or within 42 days of enrollment. While this rate approximates the Medicaid managedcare national average, HHSC believes that the high prevalence of births in the STAR populationwarrants efforts to improve timeliness of prenatal care initiation.5. Behavioral health servicesMembers must have timely access to medically necessary behavioral health services, such asmental health counseling and treatment, as well as timely and appropriate follow-up care.6. Delivery of health care to diverse populationsMember populations in Texas are as diverse as those of any state in the nation. Health careservices must be delivered without regard to racial or ethnic factors. HHSC expects the MCO toimplement intervention strategies to avoid disparities in the delivery of health care services todiverse populations and provide services in a culturally competent manner.7. Disease management requirementsEach MCO must provide a comprehensive disease management program or coverage for DiseaseManagement (DM) services for asthma, diabetes, and other chronic diseases identified by theMCO, based upon an evaluation of the prevalence of the diseases within the MCO’s membership.8. Service CoordinationThe integration of acute care services and community-based long-term services and supports isan essential feature of STAR PLUS. A STAR PLUS MCO must demonstrate that there aresufficient levels of qualified and competent personnel devoted to service coordination to meetthe everyday needs of STAR PLUS members, including dual eligible members.9. Continuity of CareHHSC expects that established member/provider relationships, existing treatment protocols, andongoing care plans will not be impacted significantly when a client moves into managed care.Transition to the MCO must be as seamless as possible for members and their providers.To achieve these goals, the State has established a number of public and private partnerships.First and foremost the State fosters both a contractual and collaborative relationship with itsMedicaid MCOs. Statewide medical and hospital associations are strategic implementationpartners as well. The State solicits input and advice from community-based organizations andregional advisory committees to further support and improve the State’s local efforts. Other6
Texas Medicaid Managed Care Quality Strategycritical implementation partners include the State’s eligibility and enrollment contractor, theTexas Medicaid claims administrator contractor for fee-for-service claims, and stakeholder stateagencies.Medicaid Dental Program ObjectivesHHSC contracts with dental managed care organizations to provide customer-centered andquality-driven dental services to Texas Medicaid recipients less than 21 years of age. HHSC’sobjectives are to:D.1.Provide quality, comprehensive dental services through qualified and accessible Texas dentalproviders.2.Provide dental care in a manner that improves oral health of members through preventivecare and health education initiatives and activities.3.Provide intervention strategies to avoid disparities in the delivery of dental services todiverse populations, and to provide dental services in a culturally competent manner.Cultural competency means the ability of individuals and systems to provide serviceseffectively to people of various cultures, races, ethnic backgrounds, and religions in amanner that recognizes values, affirms and respects the worth of individuals and protectsand preserves their dignity.4.Provide Dental Program recipients with a choice of dental plans.Managed Care Program Management StrategyHHSC’s fundamental commitment is to contract for results. HHSC defines a successful result asthe generation of defined, measurable, and beneficial outcomes that satisfy the Contractrequirements and support HHSC’s missions and objectives. The managed care contracts describewhat is required of the MCO in terms of services, deliverables, performance measures, andoutcomes, and unless otherwise noted, places the responsibility for how they are accomplishedon the MCO.HHSC has focused its performance measurement efforts by developing a Performance IndicatorDashboard, which is a series of measures that identify key aspects of performance to ensure theMCO’s accountability. The Performance Indicator Dashboard is not an all-inclusive set ofperformance measures; HHSC measures other aspects of the MCO’s performance as well.Rather, the Performance Indicator Dashboard assembles performance indicators that assessmany of the most important dimensions of the MCO’s performance, and includes measures that,when publicly shared, will also serve to incentivize excellence.In addition to the Dashboard, HHSC develops two overarching goals and negotiates a third goalsuggested by the MCO each year for health care quality improvement. The MCO must identifyand propose annual MCO Performance Improvement Projects (PIPs) related to these overarchinggoals. These projects are highly specified and measurable and reflect areas that presentsignificant opportunities for performance improvement. Once finalized, the MCO is committedto making its best efforts to achieve the established goals.HHSC also recognizes the importance of applying a variety of financial and non-financialincentives and disincentives for demonstrated MCO performance. It is HHSC’s objective torecognize and reward both excellence in performance and improvement in performance withinexisting state and federal financial constraints. It is likely that this approach will be modified overtime based on several variables, including accumulated experience by HHSC and the MCO,changes in the status of state finances, and changes in each MCO’s performance levels.7
Texas Medicaid Managed Care Quality StrategyThe incentives and disincentives are linked to some of the measures in the Performance IndicatorDashboard. The MCO’s performance relative to the annual PIPs may also be used by HHSC toidentify and reward excellence and improvement by the MCO in subsequent years.Finally, HHSC plans to improve methods for sharing information regarding the Texas MedicaidProgram with all of the MCOs through HHSC-sponsored workgroups and other initiatives.E.External Quality Review OrganizationThe Balanced Budget Act of 1997 requires State Medicaid agencies to provide for an annualexternal independent review of the quality outcomes, timeliness of, and access to servicesprovided by Medicaid managed care organizations.To ensure HHSC meets CMS requirements for quality in managed care and to provide HHSC withanalysis and information to effectively manage its Medicaid Managed Care Program, HHSCcontracts with the Institute for Child Health Policy (ICHP) at the University of Florida as theExternal Quality Review Organization (EQRO).The Centers for Medicare and Medicaid Services (CMS) requires the EQRO to perform thefollowing three functions:Validation of performance improvement projects.Validation of performance measures.A review to determine MCO compliance with certain federal Medicaid managed careregulations.In Texas, the EQRO also performs the following:Focused quality of care studies.Encounter data validation.Assessment or validation of member satisfaction.Provides assistance with rate setting activities.In collaboration with the EQRO, HHSC evaluates, assesses, monitors, guides, and directs theMedicaid managed care programs and organizations for the State.II.ASSESSMENTA.Quality and Appropriateness of Care and ServicesThe MCO must provide for the delivery of quality care with the primary goal of improving thehealth status of members or, where the member’s condition is not amenable to improvement,maintain the member’s current health status by implementing measures to prevent any furtherdecline in condition or deterioration of health status. The MCO must work in collaboration withproviders to actively improve the quality of care provided to members, consistent with theQuality Assessment and Performance Improvement (QAPI) Program and all other requirementsof the Contract. The MCO must also provide mechanisms for members and providers to offerinput into the MCO’s quality improvement activities.To help HHSC monitor performance, the MCO must provide all information necessary to analyzethe MCO’s provision of quality care to members using measures determined by HHSC inconsultation with the MCO and the EQRO. Such measures must be consistent with Health PlanEmployer Data Information System (HEDIS) or other externally based, reliable and valid measuresor measurement sets that involve collection of information beyond that present in enrollmentand encounter data.8
Texas Medicaid Managed Care Quality StrategyRace/Ethnicity, and Primary LanguageThe State obtains race, ethnicity, and primary language from the enrollment form completed bythe recipient. Applications are processed through the Texas Integrated Eligibility RedesignSystem (TIERS) and routed to a third-party enrollment broker. The enrollment broker transmits afile containing the race/ethnicity and primary language of each enrollee to the MCOs monthly.The EQRO provides additional support by identifying enrollee composition by MCO and byprogram and assesses MCO risk groups using the encounter data.HHSC Overarching Goals and Performance Improvement ProjectsBased on Medicaid managed care members’ outcomes and quality of care performance results,calculated using data from member surveys, and enrollment, eligibility, claims, and encounterfiles, HHSC establishes two overarching goals and negotiates a third goal suggested by the MCO.These goals enable the MCOs to target specific areas for improvement that will impact thegreatest numbers of enrollees. The 2012 overarching goals established by HHSC for STAR are:Improve treatment for ambulatory care sensitive conditions (ACSCs) through reduction ofemergency department visits.Improve access to specialty care.For STAR PLUS, they are:Improve member understanding and utilization of service coordination.Reduce Nursing Facility admission rates.The MCO must identify and propose annual Performance Improvement Projects ( PIPs) related tothe overarching goals. The MCO is required to provide three PIPs per MCO Program; at least onePIP must be related to an overarching goal established by HHSC. When conducting PIPs, MCOsare required to follow the ten-step CMS protocol.HHSC will work with the DMOs to establish overarching goals and Performance ImprovementProjects for Children’s Medicaid Dental Services in 2013.Performance Indicator Dashboards for Quality MeasuresHHSC tracks other key aspects of MCO and DMO performance through the use of PerformanceIndicator Dashboards for Quality Measures (see Uniform Managed Care Manual, Chapter 10.1.7,and Uniform Managed Care Manual, Chapter 10.1.10 for a complete list of MCO qualityperformance indicators for STAR, STAR PLUS, and Medicaid Dental Services). HHSC updates thePerformance Indicator Dashboard for Quality Measures annually based on MCO submissions,data from the EQRO, and other data available to HHSC.Quality Assessment and Performance Improvement (QAPI)Each MCO must develop, maintain, and operate a Quality Assessment and PerformanceImprovement (QAPI) Program that meets state and federal requirements. The MCO mustapproach all clinical and non-clinical aspects of quality assessment and performanceimprovement based on principles of Continuous Quality Improvement (CQI)/Total QualityManagement (TQM) and must:Evaluate performance using objective quality indicators.Foster data-driven decision-making.Recognize that opportunities for improvement are unlimited.Solicit member and provider input on performance and QAPI activities.Support continuous ongoing measurement of clinical and non-clinical effectiveness andmember satisfaction.9
Texas Medicaid Managed Care Quality StrategySupport programmatic improvements of clinical and non-clinical processes based on findingsfrom ongoing measurements.Support re-measurement of effectiveness and member satisfaction, and continueddevelopment and implementation of improvement interventions as appropriate.Clinical Practice GuidelinesThe MCO must adopt not less than two evidence-based clinical practice guidelines for eachapplicable MCO Program. Such practice guidelines must be based on valid and reliable clinicalevidence, consider the needs of the MCO’s members, be adopted in consultation with networkproviders, and be reviewed and updated periodically, as appropriate. The MCO must developpractice guidelines based on enrollees’ health needs and opportunities for improvementidentified as part of the QAPI Program.E
Amerigroup Texas UnitedHealthcare Community Plan . The MCO’s ability to ensure that network providers receive timely and fair payment for services rendered is a key component of