Transcription
Gordon’s Functional Health PatternMaj Nusrat BashirRN,RM,BScN,MScN
Nursing processAlfaro defines the nursing process as ―anorganized, systematic method of givingindividualized nursing care that focuses onidentifying and treating unique responses ofindividuals or groups to actual or potentialalterations in health.‖
Nursing processBasically, the nursing process provides each nurseaframework to utilize in working with the patient. Theprocess begins at the time the patient needsassistance withhealth care, and continues until the patient nolonger needsassistance to meet health-care maintenance.The nursing process utilizes the cognitive(intelligence, critical thinking, and reasoning),psychomotor (physical), and affective (emotion andvalues) skills and abilities a nurse needs to plan
ROLE IN PLANNING CAREFirst, the patient has a right to expect that thenursingcare received will be complete, safe, and of highquality. Ifplanning is not done, then gaps are going to exist inthe care,impacting patient outcomes.
NURSING PROCESS STEPSThere are five steps, or phases, in the nursingprocess: assessment, diagnosis, planning,implementation, and evaluation.These steps are not different; rather, they overlapand build oneach other. To carry out the entire nursing process,you mustbe sure to complete each step accurately and thenbuild uponthe information in that step to complete the nextone.
ASSESSMENTThe first step, or phase, of the nursing process isassessment.During this phase, you are collecting data (factualinformation)from several sources. The collection andorganizationof these data allow you to:1. Determine the patient’s current health status.2. Determine the patient’s strengths and problemareas(both actual and potential).3. Prepare for the second step of the process—
Data Sources and TypesThe sources for data collection are numerous, but it isessentialto remember that the patient is the primary data source.No one else can explain as accurately as the patientcan the start of the problem, the reason for seekingassistance or theexact nature of the problem, and the effect of theproblem onthe patient.Other sources include the patient’s family or significantothers; the patient’s admission sheet from the admittingoffice; the physician’s history, physical, and orders;laboratory and x-ray examination results; informationfrom
Assessment data can be further classified as typesofdata. the data types are subjective, objective,historical, and current.Subjective data are the facts presented by thepatientthat show his or her perception, understanding,and interpretation of what is happening. Anexample of subjective data is the patient’sstatement, ―The pain begins in my lower back andruns down my left leg.‖
Objective data are facts that are observable andmeasurable by the nurse. These data are gatheredby thenurse through physical assessment, interviewing,and observing, and involve the use of the senses ofseeing, hearing,smelling, and touching. An example of objectivedata is themeasurement and recording of vital signs.Objective dataare also gathered through such diagnosticexaminations as
Historical data refer to health events thathappenedprior to this admission or health problem episode.An exampleof historical data is the patient statement, ―The lasttimeI was in a hospital was 1996 when I had anemergencyappendectomy.‖
Current data are facts specifically related to thisadmission or health problem episode. An exampleof thistype of data is vital signs on admission: T 99.2F, P78, R 18,BP 134/86. Please note, that just as there isoverlapping ofthe nursing process steps, there is also overlappingof thedata types. Both historical and current data may beeithersubjective or objective. Historical and current data
First is the overall admission assessment, whereeach pattern is assessed through the collection ofobjective and subjective data. This assessmentindicates patterns that need further attention, whichrequires implementation of the second level ofpattern assessment. The second level of patternassessment indicates which nursing diagnoseswithin the pattern might be pertinent to this patient,which leads to the third level of assessment, thedefining characteristics for each individual nursingdiagnosis.
A primary advantage in using this type ofassessment is the validation it gives the nurse thatthe resulting nursing diagnosis is the most accuratediagnosis. Another benefit to using this type ofassessment is that grouping of data is alreadyaccomplished and does not have to be a separatestep.
Data GroupingData grouping simply means organizing theinformation intosets or categories that will assist you in identifyingthepatient’s strengths and problem areas. A variety oforganizingframeworks is available, such as Maslow’sHierarchy ofNeeds, Roy’s Adaptation Model, Gordon’sFunctionalHealth Patterns, and NANDA Taxonomy . Each ofthe
DIAGNOSISDiagnosis means reaching a definite conclusionregardingthe patient’s strengths and human responses. Thisdiagnosticprocess is complex and utilizes aspects ofintelligence, thinking,and critical thinking.
Nursing DiagnosisThe North American Nursing Diagnosis AssociationInternational (NANDA-I), formerly the NationalConference Group for Classification of NursingDiagnosis, has been meeting since 1973 to identify,develop, and classify nursing diagnoses.
Nursing diagnosisNursing diagnosis is a clinical judgment aboutindividual, family, or community responses to actualor potential health problems/life processes. Nursingdiagnoses provide the basis for selection of nursinginterventions to achieve outcomes for which thenurse is accountable.
PLANNINGPlanning involves three subsets: setting priorities,writingexpected outcomes, and establishing target dates.Planningsets the stage for writing nursing actions byestablishingwhere we are going with our plan of care. Planningfurtherassists in the final phase of evaluation by definingthe standardagainst which we will measure progress.
Expected OutcomesOutcomes, goals, and objectives are terms that arefrequentlyused interchangeably because all indicate the endpoint we will use to measure the effectiveness ofour planof care.
Expected outcomes1. Expected outcomes are clearly stated in terms ofpatientbehavior or observable assessment factors.EXAMPLEPOOR Will increase fluid balance by time ofdischarge.GOOD Will increase oral fluid intake to 1500 mLper24 hours by 9/11.2. Expected outcomes are realistic, achievable,safe, andacceptable from the patient’s viewpoint.
EXAMPLEMrs. Ahmed is a 28-year-old woman who has delayedhealing of a surgical wound. She is to receive dischargeinstructions regarding a high-protein diet. She is awidowwith three children under the age of 10. Her only sourceof income is husband pension.POOR Will eat at least two 8-oz servings of steakdaily. [unrealistic, unachievable, unacceptable,etc.]GOOD Will eat at least two servings from the followinglist each day:Lean ground meat, Eggs ,Cheese , beans ,Peanutbutter ,Fish ,Chicken
IMPLEMENTATIONImplementation is the action phase of the nursingprocess.Recent literature has introduced the concept ofnursing interventions, which are defined astreatments based on clinicaljudgment and knowledge that a nurse performs toenhancepatient outcomes.Nursing action is defined as nursing behavior thatserves to help the patient achieve the expectedoutcome.Nursing actions include both independent and
Independent activitiesIndependent activities are those actions the nurseperforms, using his or her own optional judgment,thatrequire no validation or guidelines from any otherhealthcarepractitioner. An example is deciding whichnoninvasivetechnique to use for pain control or deciding whento teachthe patient self-care measures.
Collaborative activitiesCollaborative activities are those actions thatinvolve mutual decision making between two ormore health-care practitioners. For example, aphysician and nurse decide which narcotic to usewhen meperidine is ineffective in controlling thepatient’s pain, or a physical therapist and nursedecide on the most beneficial exercise program fora patient. Implementing a physician’s order andreferral to a dietitian are other common examples ofcollaborative actions.
EVALUATIONEvaluation simply means assessing what progresshas beenmade toward meeting the expected outcomes; it isthe mostignored phase of the nursing process. Theevaluation phaseis the feedback and control part of the nursingprocess.Evaluation requires continuation of assessment thatwasbegun in the initial assessment phase.
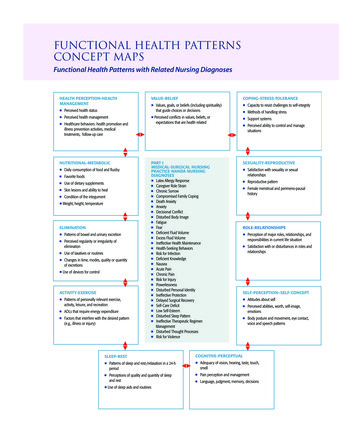
Gordon’s Functional Health PatternMarjorie Gordon (1987) proposed functional healthpatterns as a guide for establishing acomprehensive nursing database.a method used by nurses in the nursingprocess to provide a comprehensive nursingassessment of the patient.Taxonomy II of NANDA Nursing Diagnosisclassification is based on Gordon's functional healthpatterns.Gorden's functional health pattern includes 11categories which is a systematic and standardizedapproach to data collection.
These 11 categories make possible a systematicand standardized approach to data collection, andenable the nurse to determine the following aspectsof health and human function.
1- Health Perception and Management2- Nutritional metabolic3 -Elimination4- Activity exercise5 -Sleep rest6 -Cognitive-perceptual7 -Self perception/self concept8 -Role relationship9 -Sexuality reproductive10 -Coping-stress tolerance11 -Value-Belief Pattern
Health Perception and HealthManagementData collection is focused on theperson's perceived level of healthand well-being, and on practicesfor maintaining health.
Health Perception and HealthManagement Habits that may be harmful to health are alsoevaluated, including smoking and alcohol or druguse. Actual or potential problems r/t safety & health management needs for modifications in the home or needs forcontinued care in the home.
HEALTH PERCEPTION ANDHEALTH MANAGEMENT PATTERNHow has the general health been? How do you rate yourown health?2.What do you consider healthy about you? What are yourhealth goals?3.What are traditional concepts of health and illness?Beliefs and practices?4.Do you have routine physical examination? If yes howoften?5.Perform self-breast examination? (female)6.In the past year how many times have you seen a healthcare provider? For what reasons?7.In the past, has it been easy to find ways to follow thingsnurses/doctors suggest?8.What safety practices do you follow?9.Most important things to keep health? You think thesethings will make a difference to health/ (include family/folk1.
HEALTH PERCEPTION ANDHEALTH MANAGEMENT PATTERN 10. Personal hygienic practices: Describe how doyou take care of your body? Bath, hand washing,trimming of fingernails, wearing of slippers, use ofdeodorant/cologne, brush teeth, flossing, dentalvisits? 11. Substance abuse: Use of cigarette, alcohol,drugs? Kind, amount, frequency? Reasons? Aware ofeffects? Passive smoking? 12. Environmental condition: adequacy of lighting,and ventilation. 13. Environmental sanitation practices: water supply,toilet facilities, waste management, food preparation,presence of vectors, health hazards.
ADMISSION ASSESSMENTOBJECTIVE1. Mental Status2. Vision3. Hearing4. Taste5. Touch6. Smell7. General appearance
SUBJECTIVEHow would you describe your usual health status?Good Fair Poor2. Are you satisfied with your usual health status?Yes No Source of dissatisfaction:3. Tobacco use? No Yes Number of packs per day?4. Alcohol use? No Yes How much and what kind?5. Street drug use? No Yes What and how much?6. Any history of chronic disease? No Yes Describe:1-
Nutrition and MetabolismAssessment is focused on the pattern of food and fluid consumption relative tometabolic need. The adequacy of local nutrient supplies isevaluated. Actual or potential problems related to fluidbalance, tissue integrity, and host defenses maybe identified as well as problems with thegastrointestinal system.
B. Nutrition/ MetabolismPrior: Eats more of fruits and vegetables Eats her meals 3x a day with snack in between Can drink up to 1.5L of water or 4-5 glasses a day Drinks coffee in the morning and in the afternoon Claimed to be allergic on shrimps and claimed tohave good appetite
During:Weight: 41 kgHeight: 4 ft and 10 inNormal Body Mass Index; BMI 18.89 kg/m2Average Body Temperature is 360 C Able to fast in preparation for surgicalprocedure On NPO
Patientusuallyeats Patient were placed on an Foods and fluids are restrictedvegetables, meat and fish NPO status.6-8 hours prior to surgery.alternately. She’s also fond ofeating native delicacies likeAn individuals health statuspotato and meat. She drinksgreatly affects eating habitan average of 6-8 glasses ofand nutritional status.water per day, a cup of teawith bread at breakfast and 2(Fundamentals of Nursing by Kozier, pp 1178)glasses of juice during snacktime. She has difficulty inchewing and swallowing.
Sleep and RestAssessment is focused on the person's sleep, rest,and relaxation practices. Dysfunctional sleeppatterns,fatigue, and responses to sleep deprivation may beidentified.
The pattern is based on a 24-hour day and looksspecifically at how an individual rates or judges theadequacy of his or her sleep, rest, and relaxation interms of both quantity and quality. The pattern alsolooks at the patient’s energy level in relation to theamount of sleep, rest, and relaxation described bythe patient as well as any sleep aids the patientuses.
PATTERN ASSESSMENT1. Does the patient report a problem falling asleep?a. Yes (Disturbed Sleep Pattern)b. No (Readiness for Enhanced Sleep)2. Does the patient report interrupted sleep?a. Yes (Disturbed Sleep Pattern)b. No (Readiness for Enhanced Sleep)3. Does t
Marjorie Gordon (1987) proposed functional health patterns as a guide for establishing a comprehensive nursing data base.a method used by nurses in the nursing process to provide a comprehensive nursing assessment of the patient. Taxonomy II of NANDA Nursing Diagnosis classification is based on Gordon's functional health patterns.