Transcription
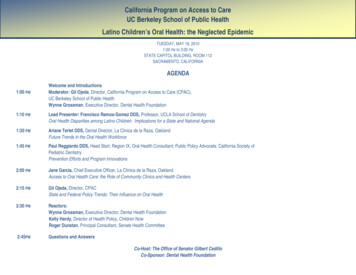
California Program on Access to CareUC Berkeley School of Public HealthLatino Children’s Oral Health: the Neglected EpidemicTUESDAY, MAY 18, 20101:00 PM to 3:00 PMSTATE CAPITOL BUILDING, ROOM 112SACRAMENTO, CALIFORNIAAGENDA1:00 PMWelcome and IntroductionsModerator: Gil Ojeda, Director, California Program on Access to Care (CPAC),UC Berkeley School of Public HealthWynne Grossman, Executive Director, Dental Health Foundation1:10 PMLead Presenter: Francisco Ramos-Gomez DDS, Professor, UCLA School of DentistryOral Health Disparities among Latino Children: Implications for a State and National Agenda1:30 PMAriane Terlet DDS, Dental Director, La Clinica de la Raza, OaklandFuture Trends in the Oral Health Workforce1:45 PMPaul Reggiardo DDS, Head Start, Region IX, Oral Health Consultant; Public Policy Advocate, California Society ofPediatric DentistryPrevention Efforts and Program Innovations2:00 PMJane Garcia, Chief Executive Officer, La Clínica de la Raza, OaklandAccess to Oral Health Care: the Role of Community Clinics and Health Centers2:15 PMGil Ojeda, Director, CPACState and Federal Policy Trends: Their Influence on Oral Health2:30 PMReactors:Wynne Grossman, Executive Director, Dental Health FoundationKelly Hardy, Director of Health Policy, Children NowRoger Dunstan, Principal Consultant, Senate Health Committee2:45PMQuestions and AnswersCo-Host: The Office of Senator Gilbert CedilloCo-Sponsor: Dental Health Foundation
Oral Health Disparities amongLatino Children: Implications for aState and National AgendaFrancisco Ramos-Gomez, DDS, MS, MPHProfessor UCLA Section Pediatric DentistryCenter to Address Children’s Oral Health DisparitiesHispanic Dental AssociationCPAC-UC California Program on Access to Carefrg@dentistry.ucla.eduCPAC Sacramento MAY 2010
Health Status of Latino Childrenand the Immigrant Paradox Low Birth Weight Infant Mortality Growth –Obesityand Stunting Asthma Dental Health Perceived HealthStatus
ASSOCIATIONS OF ORAL INFECTIONS AND MANY DISEASES13CV DiseasesHIVTraumaDiabetesECCPretermLBW babiesNutritionalproblemsCancer UCLA – Ramos-Gomez 2010
ECC in a Hispanic three year old UCLA – Ramos-Gomez 2010
SURGEON GENERAL REPORTTooth decayis the single most commonchronic childhood disease.Five times more common than asthmaSeven times more common than hay feverOral Health Status 2000 UCLA – Ramos-Gomez 20108
The effects of ECC Pain Infection Self-esteem Growth UCLA – Ramos-Gomez 2010First SmilesDental Health Begins at Birth
ORAL HEALTH AND LEARNING51 million school hourslost annually12 X lost days for childrenfrom low-income families10 UCLA – Ramos-Gomez 2010
Latino Demographics in CA One out of 3 Californians is Latino 44% of US Mexican immigrants live andwork in California San Diego has the largest binationalpopulation in the entire country11 UCLA – Ramos-Gomez 2010
12 UCLA – Ramos-Gomez 2010
Background and Significance Latino children have higher rates ofuntreated dental disease than any otherchildren in the country. Poor oral health has been associated withmultiple medical problems. Oral health problems can also lead to pain,poor nutrition and development, impairedspeech, loss of employment, time away fromschool, and low self-esteem UCLA – Ramos-Gomez 2010
UCLA – Ramos-Gomez 2010
Severe ECCChronic InfectiousDisease that istransmissible butPREVENTABLE UCLA – Ramos-Gomez 2010First SmilesDental Health Begins at Birth
Key Statistics (Dental) Latino children are at the highest risk of nothaving seen a dentist More than 50% of Latino children showeda “suboptimal” condition– 72% had dental caries– 26% had rampant dental caries(this figure is nearly twice the rate for nonHispanic whites)* 2006 California Smile Survey16 UCLA – Ramos-Gomez 2010
Poor children and children of color are morelikely to have tooth decay and suffer theconsequences of untreated disease.17 UCLA – Ramos-Gomez 2010
FindingsThe following factors contributed to theunmet dental needs of the Latinopopulation:1. Lack of dental insurance2. Lack of education about dental care3. Lack of diversity and cultural competencyamong dental providers4. Lack of access to dental care, includingtransportation and work leave time18 UCLA – Ramos-Gomez 2010
Prevalence of Dental DecayDental decay is the most commonchronic disease of childhood1 YearOlds8%92%2 YearOlds22%78%3 YearOlds35%65%4 YearOlds33%67%19 UCLA – Ramos-Gomez 2010
Can ECC be Prevented?Yes! Interventions withpregnant women andmothers of infantsInterventions withbabies and youngchildren UCLA – Ramos-Gomez 2010First SmilesDental Health Begins at Birth
MAYA PROGRAMCOLLABORATIONUCSF-UCLA WITHSYHCCANDO21 UCLA – Ramos-Gomez 2010
Perinatal & Infant Oral Carehttp://cdafoundation.org/library/docs/poh guidelines.pdf
PROMOTING INFANT ORALCARE VISITTWO IS TOO LATE !!!23 UCLA – Ramos-Gomez 2010
Policy Implications andRecommendationsCALIFORNIA STATE DENTALINFRASTRUCTURE AND OFFICECAN SET UP AN ORAL HEALTHLEGISLATIVE TASK FORCE TOCOORDINATE A COMPREHENSIVE PLANTO ADDRESS ORAL HEALTH PRIORITIESIN THE STATE OF CALIFORNIA24 UCLA – Ramos-Gomez 2010
National LegislativeOral Health Task ForceDental health areas in need for the State:****Implementing advocacy and policyprograms to improve the dental health ofLatinos focusing on pregnant women andtheir infants – AGE ONE VISITProviding culturally sensitive dentaleducation to Latino patients and providersExploring new dental services, researchand new access models for Latino FamiliesExpanding the dental health workforce toinclude more Latinos as providers.25 UCLA – Ramos-Gomez 2010
The costs andconsequencesassociated with unmetdental needs among ourLatino Childrenare too great to ignore !CARIES FREEGENERATION2000, 2010, 2020 ?26 UCLA – Ramos-Gomez 2010
Thank You!
Demographic Change Summary for LatinoChildren 1 in 4 US children will be Latino, and 1 of every 2new additions to the US populations is Latino. 60% or more of Latino children live in an immigrantfamily; one or both parents are foreign born– Risk Poverty Commonly with less than a high schooleducation Frequently not fluent in English– Strengths 70% have two parent families Multi-generational families. Pediatric Practices, general and subspecialties, willsee increasing numbers of Latino children andadolescents and most will live in an Immigrant family
Future Trends In OralHealth WorkforceAriane Terlet, DDSDental DirectorLa Clinica de La RazaMay 18, 2010
Current Models Private Practice: Solo PracticeDentist, Hygienist, Dental Assistants Community Health Center: GroupPractice
Challenges in TreatingChildren Children are not small adults Dental education programs primarilyfocus on adults Providers are not comfortable withtreating under 5 year olds
Workforce Challenges Improving efficiencies in delivery ofcare Changes in scope of practices Defining billable providers Flexibility in providing care in nontraditional settings Affordable educational programs
Necessity is the mother ofinvention There were not enough dental providerswilling to work at CHCs. No longer the casein this current economy. Dental Assistant scope of practice changedto allow dentists to be able to provide morecare to patients. RDHAP (Registered Dental Hygienist inAlternative Practice)
Many groups recognizedthe needs of providingcare to our patients National Pipeline ProjectThe California EndowmentFirst Five Oral Health CaliforniaPOHAP (Pediatric Oral Health AccessProgram)
Providing Care Outsidethe Box School based health centers Virtual Dental Home Residency Programs within healthcenters WIC Programs
Workforce EducationalPrograms Changing Changing dental education curriculums Spanish-Speaking Unity Council DentalAssisting Program Welcome Back Program
Identifying the Issues Every child taken to the OR for dentaltreatment went to every well-baby check Dental caries are a transmissible andpreventable disease. Dental education needs to include pre-nataland peri-natal care. Many dental schoolsdiscourage the treatment of pregnant women Children need to be seen at age 1
Conclusion Dental is an expensive service toprovide. We need to be efficient in ourdelivery systems and teams Prevention does work and is costeffective Coordination of services statewidewould benefit all
Future Many ideas No coordinated plan Legislative and economic challenges
Paul Reggiardo, DDSHead Start Regional Oral Health ConsultantMay 18, 2010
Head Start 101
History of Head Start Head StartEstablished in 1965 as an 8-weeksummer program to get children readyfor kindergartenFederally funded pre-school for lowincome children 3 – 5 years of age Early Head StartEstablished 1995 for children 0 – 3years of age. 10% of HS children are in EHS.
Head Start / Early Head StartProvides grants to local public andprivate non-profit and for-profitagencies to provide comprehensivechild development services toeconomically disadvantaged childrenand familiesPromotes school readiness byenhancing the social and cognitivedevelopment of children through theprovision of educational, health,nutritional, social and other servicesto enrolled children and families
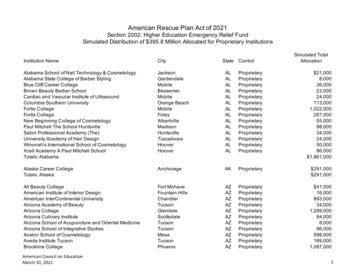
2008-2009 Program Statistics/U.S.ENROLLMENT1,055,674Ages:Number of 5 year olds & older3%Number of 4 year olds51 %Number of 3 year olds36 %Number under 3 years of age10 %Number of Pregnant Women1%
2008-2009 Program Statistics/U.S.Racial/Ethnic Composition:White40 %Hispanic / Latino34%Black/African American30 %Bi-Racial/Multi-Racial8%American Indian/Alaska Native4%Asian2%Hawaiian/Pacific Islander1%Unspecified/Other17 %
2008-09 Program Statistics# of Grantees(2007)1,604# of Centers18,875# of Classrooms51,933Avg. Cost/Child 7,727Paid Staff211,962Volunteers175,579
2008-2009 Program Statistics 93% of Head Start children had healthinsurance. 89% of those with health insurance wereenrolled in Medicaid EPSDT or S-CHIPprograms.
EligibilityHead Start is a child developmentprogram for preschoolers fromlow income families Birth to 3 (EHS) Ages 3-5 Meet family income Families receiving publicassistance (TANF or SSI)guidelinesregardless of income Slightly higher income ifspace available 10% of enrolled childrenmust be reserved for Children in foster careregardless of incomechildren with disabilities Children who arehomeless
2009 HHS Poverty Guidelines# inFamily48 ContiguousStates and DCAlaskaHawaii1 10,830 13,530 12,4602 14,570 18,210 16,7603 18,310 22,890 21,0604 22,050 27,570 25,3607 33,270 41,610 38,2608 37,010 46,290 42,560Source: Federal Register, Vol. 74, No. 14, January 23, 2009, pp. 4199-4201
Head Start Act The Head Start Act outlines the intent of the Congressfor the program, the types of services provided, thepopulation served, reporting and evaluationrequirements, and administrative requirements.Source: ead%20Start%20Act/headstartact.html
Head StartProgram Performance Standards The code of Federal regulations- 45 CFR PART 1304— contains the program performance standardsfor the operation of Head Start programs bygrantee and delegate agencies. The program performance standards are themandatory regulations that grantees and delegateagencies must implement in order to operate aEarly Head Start and/or Head Start program.
Head StartProgram Performance StandardsProvide Head Start grantee regulations for early childhood educationhealth and safetynutritiontransitionsocial and emotional developmentdisabilitiesparent involvementfamily partnershipscommunity partnershipsadministrative and financial management, and facilities
Head Start Oral Health Performance Standards Within 90 days of enrollment, each child must receivean examination by a licensed dentist All oral health needs identified on initial orsubsequent examinations must be resolved bycomprehensive, timely, appropriate treatment. All diagnostic, preventive and treatment servicesmust subsequently be provided according to the stateEPSDT schedule. If a child does not have a Dental Home (ACCESS),grantees must assist families in accessing a source ofcontinuous, comprehensive care.
California Head Start2007-08 PIR DataCAReg. IXUSAC16 Dental Home93%93%97%C17 Completed Professional Examination91%91%89%C17a Received Preventive Care94%84%85%C17b Needs Treatment31%32%24%C17c Received/Receiving Treatment91%91%84%
Denti-Cal Service UseBy Age Group (2007)HMA analysis of 2007 Medi-Cal data
Medi-Cal ChildrenReceiving EPSDTPreventive DentalServices , 2007HMA Analysis of MIS/DSS 2007 date extracted by JEN Associates
Among ethnic groups, thepercentage of Medi-Calbeneficiaries who useddental services in 2007ranged from 23% to 31%,with Latinos showing thelowest utilization rate.HMA Analysis of 2007 Medical Data
California Head Start2007-08 PIR DataCAReg. IXUSAC16 Dental Home93%93%97%C17 Completed Professional Examination91%91%89%C17a Received Preventive Care94%84%85%C17b Needs Treatment31%32%24%C17c Received/Receiving Treatment91%91%84%
California Head Start Enrollment, 2009RegionRegion 9Region 11 - AIANRegion 12 MSHSTotal Cumulative LatinoEnrollmentEnrollment% 76,15499.79%123,30988,34971.65%
California Head Start Programs, 2009RegionRegion 9Number ofProgramsPrograms with % Predominant50% LatinoLatinoEnrollmentEnrollment18614879.57%Region 11 - AIAN1300.00%Region 12 MSHS1111100.00%21015975.71%
California Head Start Staff, 2009RegionRegion 9Region 11 - AIANRegion 12 MSHSNon-Supervisory Hispanic Non% Hispanic Nonchild development Supervisory child Supervisory childstaffdevelopment staff development 0347,75359.48%
California Head Start Staff, 2009RegionRegion 9Region 11 - AIANRegion 12 MSHSNon-Supervisory Non-Supervisory % Nonchild development child development Supervisory childstaffstaff proficient in development staffa language other proficient in athan Englishlanguage otherthan 13,0347,39956.77%
AAPD / OHSDental Home Initiative
Access to Oral Health andthe Role of CommunityClinics and Health CentersJane GarciaCEO, La Clinica de la RazaMember, CPCA Board of DirectorsMay 18, 2010
Presentation Overview1. Background on CCHCs and Dental2. Challenges in Serving Children– State Budget Cuts– Workforce– Four Walls3. Opportunities on the Horizon forCCHCs– Health care reform– ARRA
La Clínica- Who we are? Service locations: 6 locations spanning 3 CountiesPatients: 22,573 patients seen in 2009Visits: 68,661 visits in 2009Chairs: 47Services offered: Dental Exams, Fluoride andSealant Treatment, Cleaning and Polishing, DentalHygiene, General Dentistry, Periodontics,Orthodontics, Pedodontics, Endodontics 18,833* of total patients seen under 100% of theFPL FY 2009- 12.9 Million Operating Budget
Community Clinics and Health Centers: TheSafety Net for California 825 clinics in CA Private andnonprofit Serve all whocome through theirdoors Primary care medical, dentaland mental health
Community Clinics and Health Centers: TheSafety Net for California CCHCs serve4,267,063patients 2,763,337 under100% of the FPL Most uninsured oron Medi-Cal Primarily womenand children 55% Hispanic 45% ESL
Community Clinics and Health Centersand Dental in California Dental primary care262 clinics offer dental1,355 dental FTEs1,457,207 dental encountersFQHCs cannot restrict to children
Challenges in Serving Children:Budget Cuts 2009-10 Budget– Elimination of Medi-Cal optionalbenefits Optional benefits include dental,optometry, podiatry, chiropractic– Elimination of funding for TraditionalClinic Programs Includes the Expanded Access to PrimaryCare (EAPC), Seasonal and AgriculturalMigratory Workers (SAMW), and RuralHealth Services Development (RHSD)programs
CCHCs and Adult Dental Results from CPCA’s survey ofmembership in Fall of 2009– 30 million in revenue lost– 77 dental providers laid off– 2 dental clinics closed– Expect to see worse results in futuresurveys
CCHCs and Adult Dental“We have heard that people are having a hardertime finding jobs because their teeth are sobad. Their perception is that they are notpresenting well in interviews.”“Unfortunately, our patients have to take the bruntof this situation. Our patients that previouslyreceived benefits that have now beeneliminated now have to pay out of pocket.Dental services are a necessity when ourpatients are in pain.”
Hope on the Horizon Health Care Reform– 11 billion for FQHCs– 1 billion to California FQHCs Health Information Technology– 36 billion for Medicare/Medicaidelectronic health records incentivefunds– 2 billion for supporting services Some concerns remain
Questions?
Oral Health Policy ImpactingLatino ChildrenIssues in California and the NationbyGilbert Ojeda, DirectorCalifornia Program on Access to CareUC Berkeley School of Public HealthFor Presentation at the State CapitolMay 18, 2010
I. Point of View CPAC established in 1997 by UC to create institute to improveknowledge base thru academic based thinking for California’s decisionmakers on access to health care for immigrants and the working poor. Monitor State initiatives including Medi-Cal, Healthy Families, andState based health care reform towards preserving and strengtheningservices for vulnerable populations. Serve as “incubator” for health care access initiatives, includingHealth Initiative of the Americas, Medicaid Research Institute, Stateonly programs, bi-national coverage, and non-profit care forvulnerable populations
II. Recent State Oral Health Policy Actions Greater take-up of dental care in Health Families under age of five;State coverage for immigrant children under State only programs. Preservation of Denti-Cal for children, despite elimination of adultDenti-Cal in 2008-09 State Budget; preserved for FY 2009-10. Maintenance of dental care for pregnant women through Medi-Caland State’s Prenatal Care Program, which serves predominantlyLatino immigrant women. Suspension of State’s Dental Disease Prevention Program for 300,000school children focused on oral health promotion and prevention. Mandating movement of Healthy Families children to capitated plansfor 1st two years, likely to lead to less access and preventive care. Imposing 1,500 yearly limit on dental care for Health Families kids.
III. Policies under Federal Health Care Acts Expansion of 1,000’s of National Health Service Corp positions,including for training of dentists, under recent ARRA legislation andthe Health Care Reform Act (HCR). The S-CHIP Re-Authorization (2009) requires states to provide dentalcoverage to enrollees, not allowing states to back-out of coverage. 2009 Act may also require HF to improve dental care to meet minimum requirements, if HF program survives the proposed elimination. Under HCR: state dental requirements mandated to include review ofadequacy of provider payments & improved oral health data collection Under HCR: there will be grants to states for school-based dentalsealant programs, which could lead to start-up of California’ssuspended Dental Disease Prevention Program. Under HCR: there will be 11 billion over 5 years for communityclinics- 9.5 B for expansion, 1.5 B for infrastructure. Also under HCR, CDC grants to improve outreach, oral health publiceducation campaigns, and mandated pediatric dental for health plans.
IV. State Budget: Past Years, Current Year The elimination of Medi-Cal’s adult dental program undercut dentalinfrastructure and core funding base of hundreds of clinics- public,non-profit and private providers, which have traditionally servedDenti-Cal patients. Last year’s State budget proposed the elimination of Healthy FamiliesProgram; it was saved at the 11th hour thru 1-time support derivedfrom private health insurers and the State First Five Commission. This year’s May Revise State Budget again calls for eliminating theentire Health Families Program serving over 900,000 children, over55% Latino. With bipartisan support for children and community clinics, it ishoped that another “last minute” compromise will be secured toprotect Health Families children.
V. New Initiatives for Tough Times In California, passage of a beverage/soda tax with directed funds toprevent obesity/diabetes, dental caries with an emphasis on parenteducation and funding for oral health care. In CA, new rules on the Free and Reduced Lunch Program in theschools; recipients, disproportionately Latino suffer from higher ratesof tooth decay. In CA, increased promotion of flouride varnishes and dental sealantsthrough both Medi-Cal and Healthy Families due to proven Statebudget cost savings; could attract demonstration project fundingthrough health care reform. Create incentives for private dentists thru HR expanded coverage tosign-up for the State’s public programs; declines in dental care forchildren thru Medi-Cal (31%) and Healthy Families (56%) thought tobe directly dependent on provider availability.
VII. What do we do now? In dire times we plan for better times We protect what we have in CA, and bring back what we can thrufederal opportunities and mandates under HCR We learn from other States, whether it be Washington with itsABDC program or Massachusetts with its Toothbrush Time in thepre-school and kintergarden. We do the simple things that don’t cost lots of public dollars, butthat save public dollars and wait for federal opportunities. Remember once HCR is in full gear in 2014 or even if CA opts forexpanded Medi-Cal in 2011 the opportunities for expanded publiccoverage will proliferate. We plan, we wait, we act
, Executive Director, Dental Health Foundation. 1:10 PM Lead Presenter: Francisco Ramos-Gomez DDS, Professor, UCLA School of Dentistry. Oral Health Disparities among Latino Children: Implications for a State and National Agenda . 1:30 PM Ariane Terlet DDS, Dental Director, La Clinica de la R