Transcription
H. W. Anselm WiskottFIXED PROSTHODONTICSPRINCIPLES AND CLINICSLondon, Berlin, Chicago, Tokyo, Barcelona, Beijing, Istanbul, Milan,Moscow, New Delhi, Paris, Prague, São Paulo, Seoul and Warsaw
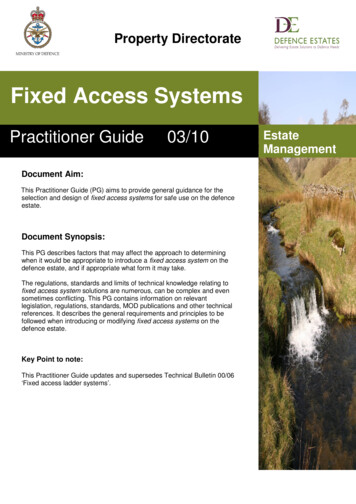
ForewordThis book was written for dental students. It is intendedto guide the prospective practitioner towards a scholarly approach to clinical problems. As such, it deals withthe principal concepts and clinical steps of fixed prosthodontics.The text was laid out to provide the reader with abroad view of the field and then concentrate on the essentials of restorative dentistry using fixed prostheses.It also involves the interrelationships between basicsciences (as discussed in Oral Environment), the clinical disciplines of periodontics, orthodontics, operativedentistry and implantology (in Preprosthetic Phase) andthe realm of fixed prosthodontics (in Prosthetic Phase).In the chapters we will discuss the scientific backgroundfirst and then move to clinical applications. In analogywith other human endeavors, prosthetic dentistry can beconducted at the strategic, the operational and the technical levels. We will address all three levels, but qualifiedas follows. First it is recognized that while the underpinning scientific evidence is quite homogenous, the strategic options at the planning stage are often numerous.This equally applies to the operational decisions duringthe development of a treatment sequence and to thetechnical level, that is, the clinical techniques appliedduring execution. Second, a textbook should be both alearning and a teaching aid, thereby implying that it mustprovide the teacher with something to teach. It is therefore recommended that the workflows described in theclinical sections be adapted to optimally suit individualneeds. Third, the present text does not recommend anyspecific brands but only describes procedures using generic terminology. This acknowledges the availability ofmany products of superior quality without the need foran author to direct the clinician to a specific make.Besides the scientific background and the clinicalsteps, many chapters also include a historical perspectiveon the topics presented. As a medical discipline, Dentistry has a long and distinguished history in which a hostof researchers and clinicians built the body of evidencethat supports contemporary scientifically-based treatment options. In this author‘s opinion, paying tribute toour predecessors and acknowledging their merits shouldbe part of an academic approach to dental education.Texts that aim at conveying organized knowledgemust be laid out in a methodical fashion. The subjectmatter and the terminology must be introduced to thereader in an orderly sequence. In this regard, attentionwas focused on structuring the chapters so that laterchapters build upon the information that was providedin earlier sections. In line with to this principle, the text isabundantly cross-referenced. In the few instances wherebreaks were included into logical sequencings, those areclearly indicated to the reader.This text aims at conveying sometimes arduous andcomplex notions to clinicians in the early phases of theirprofessional development. At times this may requirethat first order approximations be made and that notall idiosyncrasies, exceptions, or clinical intricacies beconsidered individually – there is a limit to the amountof information that can be included in a chapter withoutblurring the message. Also, the author considers himself a friend of proper terminology. Therefore wheneverapplicable, the Glossary of Prosthodontic Terms will beused as reference – streamlining terminology helps inavoiding confusion and misunderstanding. Still, terminology should not be unnecessarily complex – referring to ‘airborne particle abrasion‘ for a process whichthe entire world calls ‘sand-‘ or ‘grit-blasting‘ imposesunnecessary wordiness to the reader. Similarly, denoting an artificial crown by the word string ‘single unitfixed dental prosthesis‘ may be correct according tosome authorities but needlessly burdens a text. Further,whenever applicable, the reader will be provided withsynonyms for a given term. ‘Synonym‘ is used throughout as it is understandable to the broad readership,although ‘alias‘ or ‘AKA‘ (‘also known as‘) might be preferable, as they do not imply a 100% duplication of themeaning but still allow some leeway between the different exceptions.Principles and clinical situations are all explainedusing diagrams and it is fully acknowledged that thoseare idealized views of an often more complex reality. Onthe upside though, schematic views are ideally suited todirect the reader‘s attention onto specific elements asextraneous aspects are largely out of focus.Last, with the exception of chapter 3 (it is difficult toexplain color in whiter shades of pale), the artwork is keptin black and white format. This is to reduce printing coststo a bare minimum and to allow a wide distribution ofthe book among students.V
AcknowledgementsFirst and foremost, I am indebted to my wife Yolande –my companion and friend for many years. Besides beinga superb mother to our two daughters, her love and enduring support have been most rewarding. Second, mygratitude is expressed to Drs Marie-Christine and PeterDulguerov for their indefectible friendship. The friendlyworking atmosphere in their company has been an enjoyable experience throughout.This text reflects years of lectures, conversation anddebate with teachers, colleagues and friends (not necessarily mutually exclusive). While it would be impossibleto name them all, it is the author’s wish to acknowledgethe direct or indirect contribution of the following individuals.First, Dr Robert Faucher to whom this book is dedicated for his questioning, his incisiveness and his healthydisrespect for any form of dogma. Then the late Dr Sigurd Ramfjord and Dr Raul Caffesse at the University ofMichigan in Ann Arbor. My gratefulness extends to bothfor developing and maintaining a graduate program inperiodontics, of which an important part consisted inconveying the importance of structured literature surveys. I am also indebted to the late Dr Robert Moyers whospent countless hours teaching me the nuts and boltsof orthodontic bracket placement and wire bending. Mygrateful appreciation is extended to Drs Edith Morrison,Gunnar Svanberg and Walter Loesche for sharing theirinsights on experimental microbiology. Special thanksalso to Dr Joseph Clayton for his rocky but fruitful introduction to occlusal concepts and applications.The author was fortunate to spend three further yearsunder the guidance of Dr Ralph Yuodelis and Jack Nicholls at the University of Washington in Seattle. The education was both practical and theoretical, and definitivelyestablished the relationships between fixed prosthodontics, periodontics and material science and engineering.The teaching staff was knowledgeable, open minded andVIhelpful. My deep gratitude specifically goes to the lateDrs Saul Schluger and William Ammons.A number of other individuals have brightened myprofessional career. In this regard, I am indebted to DrsSusanne Scherrer and Claude Crottaz for their unyieldingsupport; to the late Dr Jean-Noël Nally and Dr JacquesHolz for demonstrating leadership and steadfastness; toDr Hans Thiel for introducing me to real world of dentistry, and to Messrs Alwin Schönenberger and RogerRenevey for their meticulous laboratory work. My gratitude is extended to Dr Urs Belser for suggesting that thisbook be written.My appreciation also goes to our colleagues at thelaboratory of applied mechanics at EPFL in Lausanne,Switzerland.A variety of websites were used during the writingof this text. Besides “general purpose” sites such as www.thefreedictionary.com and www.wikipedia.org, a numberof other sites devoted to more specific aspects also provided information. The author expresses his gratitudeto all those who have selflessly constructed websitesto share their knowledge with the internet community(whenever feasible, they are referenced in the bibliography). A special mention goes to Dr Martin Spiller (www.doctorspiller.com) for his unconventional approach andrefreshing tone when bringing dental medicine to thegeneral public.Many thanks also to all those who have contributedphotographs.The text is unquestionably more readable due to theeditorial changes of Mrs Lotika Singha, who was able toconvert the author’s convolute, intricate, and at timesconfused sentences into a phrasal stream that is pleasant to read.Likewise the friendly support of the editorial staff atQuintessence during the layout and proofreading stagesis greatly appreciated.
ContentsINTRODUCTIONCHAPTER 1The Prosthodontic Environment1.1Introduction1.2Scope of chapterPart 1 Lost and defective teeth1.3Prevalence and causes of tooth loss1.4Defective teeth1.5The need and demographics of fixed versusremovable prosthodonticsPart 2 The realm of fixed prosthodontics1.6Prosthetic dentistry and its subspecialties1.7Elementary principles of fixed prosthodontics1.8The fixed prosthodontic workflow1.9In fine References1122289121213171818ORAL ENVIRONMENTCHAPTER 2Anatomy and Pathophysiology2.1Scope of chapter2.2Terminology2.3Teeth and periodontal support2.4Dental arches2.5HeadReferences21212122323541Part 1 Constructing a smile3.5Objective3.6Constraints3.7Setting the maxillary central incisors3.8Tooth arrangement3.9Incisors3.10 Gingival esthetics3.11 SummaryPart 2 Color3.12 Light and color perception3.13 Color spaces3.14 The color of teeth3.15 Measuring color3.16 The role of 65CHAPTER 4Forces and Mastication694.1Introduction4.2Scope of chapter4.3Mastication4.4Neurological controls4.5Forces generated during clenching and chewing4.6Bruxism4.7Long-term forces4.8Clinical implicationsReferences696970768387889192CHAPTER 5Mandibular Movements andFunctional Occlusion97CHAPTER 3Esthetics and Color3.13.23.33.4IntroductionScope of chapterEsthetics, cosmetics, and normal anatomyEsthetic parameters as perceived bypatients and dentists43434444455.1Introduction5.2Scope of chapterPart 1 Functional anatomy of thetemporomandibular joint5.3The disc5.4Articular surfaces5.5Synovial membrane5.6Ligaments and capsule97989898100101101VII
Contents5.7Joint remodeling102Part 2 Jaw movements1025.8Envelope of motion1025.9Posterior guidance – temporomandibular joints 1045.10 Anterior guidance – anterior teeth, disclusion1085.11 Mandibular positions1085.12 Interarch occlusal contacts1115.13 Vertical dimension of occlusion117Part 3 Historical perspective1195.14 Early authors (1800–1960)1195.15 The advent of anterior disclusion mechanics1215.16 Gnathology1215.17 In fine 123References123CHAPTER 6Materials and Structures6.1Introduction6.2Scope of chapterPart 1 Structures6.3Tooth as a supporting structure6.4Fracture6.5Strength6.6Models and modelingPart 2 Biologic compatibility6.7Testing for biocompatibility6.8Prevalence of adverse reactions6.9Biocompatibility of metals6.10 Biocompatibility of resin-based materials6.11 Biocompatibility of ceramic materials6.12 In fine 59160161TREATMENT PLANCHAPTER 7Treatment PlanningPart 1 Introduction7.1Indications for fixed dental prostheses7.2Scope of chapter7.3Project managementPart 2 Diagnosis7.4General diagnosisVIII1671671671691701711717.5Dental diagnosisPart 3 Treatment objectives7.6General principles7.7Setting treatment objectives for single teeth7.8Setting treatment objectivesfor small edentulous spaces7.9Compounding factors7.10 Setting treatment objectivesfor multiple missing teethPart 4 Treatment sequence7.11 Establish preprosthetic arches:preprosthetic phase7.12 Construct the prosthesis: prosthetic phasePart 5 Prospective diagnosis7.13 Diagnostic wax-up7.14 Intraoral diagnostic aids7.15 Computer imagingPart 6 Documentation and communications7.16 Written treatment plan7.17 Treatment plan presentation7.18 Written 03204204206206206206206207207PREPROSTHETIC PHASECHAPTER e of chapterPeriodontal surgeryPrinciples of osseous surgerySurgical crown exposure (crown lengthening)Augmenting soft tissue volumeCovering a local gingival recession(connective tissue and pedicle flap)8.8In fine References209209218219223227237243250251CHAPTER 9Orthodontics9.19.29.3IntroductionScope of chapterIndications for prerestorative tooth movement257257258259
Contents9.4Preliminary diagnostics9.5The physiology of orthodontic movementsPart 2 Clinics9.6Mechanics9.7Active elements9.8The downsides of orthodontic movements9.9Basic workflow9.10 ER 10Operative Dentistry10.1 Introduction10.2 Scope of chapterPart 1 Bleaching10.3 Adjustments of crown color – bleaching10.4 In-office bleaching10.5 Home bleaching10.6 Walking bleach10.7 MicroabrasionPart 2 Foundation restorations10.8 Foundation restorations10.9 Clinics10.10 In fine 32Part 1 Perspective11.1 Early developments11.2 The principles of implant surgery as per 198011.3 Scope of chapterPart 2 The biology of osseointegration11.4 Titanium11.5 Implant design features11.6 Osseous healing11.7 The morphology of the implant emergencePart 3 Bone as a self-optimizing structure11.8 Bone mass optimization11.9 Internal repair11.10 Adaptation to increased stressPart 4 Clinics11.11 Scope of section11.12 Diagnostics and planning11.13 Implant placement technique11.14 Implant placement with bone augmentation11.15 In fine ReferencesCHAPTER 12Tooth-anchored CementedRestorations38912.1 Introduction12.2 Scope of chapterPart 1 Function and design of tooth-anchoredfixed dental prostheses12.3 Applications12.4 Basic components and terminology12.5 Design principles12.6 FDP function under load12.7 FDP framework design12.8 External FDP configuration12.9 Dowel crownsPart 2 Clinics12.10 Diagnostics and planning12.11 Abutment design12.12 Clinical abutment preparation12.13 Preparation workflow12.14 In fine 22428436437CHAPTER 13CHAPTER 11Endosseous ImplantsPROSTHETIC 364364368377382382Implant Prosthodontics44113.113.2Part 113.313.413.513.613.7IntroductionScope of chapterPrinciplesSubmerged and transgingival systemsBasic componentsConnectorsFundamentals of screw-clampingChewing with natural teeth versus chewingwith implantsPart 2 Clinics13.8 Full-arch screw-fastened FDPs13.9 Contemporary designs13.10 Multiunit FDPs in partially edentulous arches13.11 Single-unit FDPs13.12 Impressions13.13 Angled abutments13.14 Evaluating framework fit13.15 Screw-retention versus cementationPart 3 56460462464465468469470472473IX
ContentsCHAPTER 14Adhesive RestorationsCHAPTER 1647714.114.2Part 114.314.414.514.614.7Part 214.814.914.1014.1114.1214.13Part 314.14IntroductionScope of chapterPrinciples of bondingBonding to enamelBonding to dentinThe clinics of dentin bondingPrinciples of dentin bonding revisitedThe chemistry of dentin bonding polymersLaminate veneersIntroductionApplicationsPrinciples of preparations for laminate veneersColor corrections using laminate veneersPatient appraisals and long-term outcomesThe clinics of laminate veneersBonded multiunit prosthesesField of application, advantages, limitations,contraindications14.15 Abutment design and frameworks14.16 Long-term survival of resin-bondedfixed dental prostheses14.17 The clinics of resin-bonded fixeddental prostheses14.18 Alternative frameworks14.19 Long-term survival of FR-FDPsReferencesAppendix: Bonding monomers, polymerizationadditives, etchants, and 49950616.1 Introduction16.2 Scope of chapterPart 1 Principles16.3 Concepts and definitions16.4 Materials16.5 TraysPart 2 Clinics16.6 Overview of materials and techniques16.7 ‘One step, double mix‘ technique16.8 Clinical workflowReferences50850817.117.217.3Part 117.417.517.617.7510510511516517521CHAPTER 15Provisional Restorations15.115.2Part 115.3529IntroductionScope of chapterPrinciplesObjectives and indications of provisionaltreatment15.4 Drawbacks of provisional restorations15.5 Materials for provisional restorationsPart 2 Clinics15.6 Workflow for fabricating provisional restorations15.7 Provisional restorations for laminate veneers15.8 Adapting and repairing provisional 578CHAPTER 17Occlusal RelationshipsIntroductionScope of chapterPrinciples governing occlusal schemesInstruments and proceduresArticulatorsFacebowsRecording interarch relationshipsEffects of articulator settings onocclusal anatomyPart 2 The clinics of conformative restorations17.8 Overview17.9 Workflow for conformative occlusionsPart 3 The clinics of reorganized restorations17.10 Workflow for reorganized occlusions17.11 Design and location of occlusal 8600607607610613CHAPTER 18Laboratory Procedures18.1 Introduction18.2 Scope of chapterPart 1 Working models18.3 The production of working models18.4 General considerations on working models18.5 Technical workflow in model fabrication18.6 In fine 615615615616616616621627
ContentsPart 2 Waxing, investing, and casting metalframeworks18.7 Introduction18.8 Metals18.9 Waxes18.10 Investing18.11 Casting18.12 Technical workflow for waxing, investing, andcastingPart 3 Fabricating frameworks using CAD-CAMmachining18.13 Introduction18.14 CAD-CAM procedures and components18.15 Scanning three-dimensional objects18.16 The computer interface18.17 The fabrication unitPart 4 Ceramic veneering18.18 Introduction18.19 Materials18.20 Ceramic layers18.21 Technical workflow for layering ceramics18.22 Layering and firing a porcelain veneerPart 5 Communicating with a dental laboratory18.23 General principles, records, and documents18.24 Color selectionReferences62762762863263663819.119.2Part 119.319.419.5Part 219.619.719.8IntroductionScope of chapterTry-in proceduresFramework try-inBisque-bake try-inFinal try-inCementationFamilies of dental cementsApplication guidelinesBiologic 51652656656656661665671672672674677CHAPTER 19Try-In and Cementation19.9 Physical propertiesPart 3 Clinics19.10 Temporary cementation19.11 Permanent cementation19.12 Conventional cementation19.13 Adhesive cementation19.14 96FOLLOW-UPCHAPTER 20Maintenance72120.1Part 120.220.320.4IntroductionConceptsMaintenance procedures – terminologyPreventing diseasePreventing the recurrenceof disease20.5 Calculus and saliva20.6 Brushing, scaling/curetting, and power-driveninstrumentation20.7 The effects of removing bacterial plaque20.8 Antiseptics20.9 FluoridesPart 2 Clinics20.10 The overall scheme:re-evaluation and cleaning sessions20.11 Intermediary cleaning sessions20.12 Re-evaluation sessions20.13 Setting a recall interval20.14 Personal oral hygiene20.15 In fine 1731735735737738738743XI
About the authorH.W. Anselm Wiskott DMD, MS, MSD, PhDDr Wiskott graduated in 1977. After three years of privatepractice and internship he earned a doctorate in dentalmedicine. He then transferred to the United States andin 1982 he received a Master of Science degree in periodontics from the University of Michigan. In 1989 he wasawarded a Master of Science in Dentistry degree fromXIIthe University of Washington, specializing in fixed prosthodontics, and in 1998 a PhD degree in biomaterials. DrWiskott is the author of about 100 scholarly articles. Heteaches and practices dentistry in Geneva, Switzerland.He and his wife Yolande have two daughters: Alexa-Seaand Kim-Aurora.
CHAPTER1The ProsthodonticEnvironment1.1 IntroductionToday, a large proportion of the aging population is motivated to “stay young”. Besides alluding to physical fitness and attractiveness, this attitude also includes themaintenance of a functional and cosmetically appealingdentition. In this context, losing one or several teeth is atraumatic event and many people experience difficultiesin coming to terms with their loss. The immediate consequences of tooth loss are functional (the person is unableto chew or speak properly) as well as cosmetic (facial appearance is adversely affected). In the long term, toothloss often impairs the person’s self-image, emotional balance, and overall quality of life.Tooth loss is not a disease per se. Still, it often leadsto disabilities of varying degrees of severity. Therefore affected individuals should be considered as persons withFig. 1-1a,b Fixed versusremovable prosthesesa The classic fixed restoration ispermanently cemented ontoconically prepared abutmentteeth.b Removable prostheses derivetheir support from bases andflanges. They are stabilized byclasps on the remaining dentalarch segments.aa disability who seek a prosthodontist’s help to re-establish the original morphology and functional capabilitiesof their dentition.Prosthodontics may be primarily regarded as the discipline of dentistry concerned with the replacement ofmissing teeth. It is commonly subdivided into fixed andremovable prosthodontics. As the name implies, removable prosthodontics refers to treatment modalities using prosthetic devices that can be removed from themouth for cleansing and maintenance procedures. Fixedprosthodontics encompasses those modes of treatmentin which the replacement teeth are permanently placedin the oral cavity (Fig. 1-1).The nature of a discipline involving prosthetics (as opposed to regenerative approaches) entails that lost tissues are replaced with artificial substitutes. This in turnimplies that ‘alloplastic’, that is, non-biologic, materialsb1-1 Fixed vs. removable1
8Periodontics66/( ,167/(6667 ,1& abdcFig. 8-54a–d Harvest the transplanta Position the tinfoil and scribe the outline.b Dissect the superficial mucosa to about 0.5 to 1 mm in thickness. Lift the “trap door”.c Incise to the bone and remove the connective tissue.d Suture the superficial flap back into place.Fig. 8-55 Position the transplant onto the recipient bed2488-55 Recession-548-57 Recession-53Step #7 Suture the transplant Now suture the transplant onto the bone bed and the roots. Start by passingthe needle in palatobuccal direction between the twopremolar crowns and place a first bite inside the fibersin the apical aspect of the flap (Fig. 8-56a). The needleis then threaded between the first premolar and thecanine and the suture tied on the palatal aspect of thefirst premolar. Proceed in the same fashion with a second thread, which is centered on the canine (Fig. 8-56b).These sutures should not be overly tight as you do notwant to cut off lateral diffusion inside the connectivetissue. Their sole purpose is to stabilize the transplantduring the initial days of healing. The palatal knots areshown in Figure 8-57b.
8.7 Covering a local gingival recession (connective tissue and pedicle flap)a8bFig. 8-56a,b Suture the transplanta Apically the sutures are hooked into the loose fibers that were left bare during initial flap preparation.b Large sling sutures are placed and tied on the palatal aspects. These sutures should not be over-tightened to allowproperdiffusion of8-56Recession-55nutrients into the transplant.abFig. 8-57a,b Suture the flapa To adequately cover the transplant, the flap is sutured coronal to its original location.b Palatal aspect and view of the sutures stabilizing the transplant.Step #8 Suture the flap Last the flap is sutured asshown in Figure 8-57, that is, coronal to its original position (note the differences in height of the mucogingivalline). For suturing, the flap will be stretched somewhatbut not “overstretched”. This requires that it be well mobilized at its base so that it can be moved around freelyand no major backward pull is perceivable. Use interrupted knots and 3-0 or 4-0 suture material.8-57 Flaps-568.7.4 Class II recessionsThe treatment of class II recessions requires doublepedicle flaps (Fig. 8-58a). These flaps are actually a moreadvanced variant of the technique demonstrated above(steps #1 to #8). The essential differences are as follows.First the tissue is incised along the lines shown in Figure 8-58a in which we are actually preparing two flaps:the distal flap (centered on the premolar recession) andthe mesial flap. The incision around the canine recession249
13Implant ProsthodonticsHence two of the most tedious aspects of impression taking of natural teeth are eliminated. First, there is no needfor exposing the margin by gingival deflection and, second, the risk of moisture contamination during the procedure is minimal.Before starting, the clinician needs to determinewhether an open or a closed tray technique will be used.13.12.1 Open tray techniqueThe open tray technique is the traditional method of securing impression copings to the implant head. In thisapproach, the copings are screw-fastened to the implantheads, which, in turn, requires that the copings be unfastened before the impression is removed from the mouth(as in Fig. 13-21). Removal is made possible by using atray provided with openings located on top of the screwheads, thereby providing access for screw release andtray removal (hence the name ‘open tray technique’).aProcedure The procedural steps are illustrated in Figure 13-34. Figure 13-34a shows the screw-fastening oftwo transfer copings on the implant heads. Note how thetransfer copings fit onto the implant heads in a malefemale keying relationship. On Figure 13-34b the operator checks that the opening in the tray allows appropriateaccess to the screw heads. Then the opening is closedwith a sheet of wax, the tray is filled with impression material and seated onto the arch (Fig. 13-34c). After theimpression material has set, the wax sheet is removedand the transfer copings are unscrewed from the implantheads (Fig. 13-34d).13.12.2 Closed tray techniquebFig. 13-33a,b First molar edentulous space The implant shouldbe placed either mesially or distally to allow the design of a crownas in (b) rather than a flaring restoration as in (a).The basic steps of the impression procedure are:1. Secure the transfer coping to the implant head.2. Take an impression using an elastomeric material.3. Releasethe coping fromthe implant head and13-33 Restorativeoptions-6remove the tray.4. Turn the tray upside down and fasten an implantanalog to the “underside” of the transfer coping.5. Pour the impression and fabricate a working model.466The open tray technique is somewhat tedious in that theimpression tray must be specially prepared. Thereforemost manufacturers have designed copings that will securely snap onto the implant heads without the need foradditional screw-fastening. Since no perforation of thetray is necessary, this method has been termed ‘closedtray technique’. Both techniques are similar in their duplicating accuracy.73Procedure The closed tray technique is illustrated inFigure 13-35. First a snap-on element that reversiblybraces around the implant collar is clipped onto the implant head and then an antirotational element (i.e., thepositioning cylinder) is inserted into the octagonal keyof the connector. The combined action of both elementsfirmly positions the implant analog during subsequentpouring of the impression.Independent of the type of connector, accurately positioning the transfer coping onto the implant head is a
13.12 Impressionsabpositioning cylinderimpression copingcdFig. 13-34a–d Open tray techniquea The transfer copings are screw-fastened into position.b The tray’s opening provides access to the coping screws.c The opening is sealed with a wax plate and the impression is taken.d The transfer copings are unscrewed from the implant heads and the impression is removed.13-34 Impressions-1positioning cylinderimpression copingFig. 13-35 Closed tray technique The impression coping isclipped onto the implant headand the positioning cylinder isseated. After the impression material has set, the coping snapsoff the implant head during trayremoval.13-35 Impressions-246713
18Laboratory ProceduresTemperature [ C]800furnaceatmospherecenter ofinvestment600400200Minutes0020406080Fig. 18-36 Thermal inertia The investment accumulates energyduring heating of the oven (i.e., heat soaking), hence the delay intemperature increase in the center ofthe investment.Datainertiafrom18-36ThermalJelenko Corp.16 to 19 g/cm3 range for high gold and in the 10 to 15 g/cm3 range for low gold alloys (the specific value must beprovided by the manufacturer). As a rule we will use 50%of the required amount as new and 50% as recycled alloyfrom previous castings.We are now ready to proceed with alloy melting andcasting. The various heating methods have been discussed previously. The casting machines may be subdivided into two groups: centrifugal and air-pressure driven devices.Centrifugal casting As the name implies, these machines will drive the molten alloy into the mold usingcastingringcradlecruciblemeltcentrifugal force.115 Thus they feature a rotating beamthat spins around a vertical axle with the crucible affixedto one end. They are built so that they start spinningbriskly thereby applying a high force during the initialturns. Rotation is generated by a coil which is rewoundprior to the procedure and released at the time of casting.The beam itself has a clever design in that it is made oftwo articulating parts (technical term: broken arm). Ifblowtorch heating is used, this allows the operator toposition the crucible in line with the flame, thereby facilitating the melting of the alloy. The design and workingprinciple of a centrifugal casting machine are shown inFigure 18-37.Whenever a dental alloy is brought to melting temperature in ambient air, a pellicle
dentistry and implantology (in Preprosthetic Phase) and the realm of !xed prosthodontics (in Prosthetic Phase). In the chapters we will discuss the scienti!c background !rst and then move to clinical applications. In analogy with other human endeavors, prosthetic dentistry can be conducted