Transcription
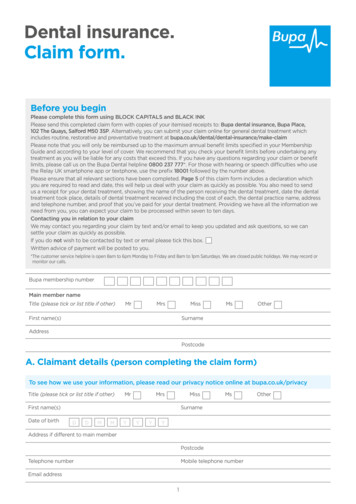
,-llgK ATEIMedicalIndemnity FundMIF Claim Submission GuidanceOctober 2019MIF Claim Submission Guidance – Provider ClaimsOverviewBelow are claim submission guidelines for providers submitting claims to the Medical Indemnity Fund (MIF).This guidance will be updated periodically to address common questions and concerns relating to MIF claimsubmission. The guidance below assumes all applicable authorizations have been obtained.If you have any questions about obtaining authorizations or submitting claims, please contact us:MIF@health.ny.gov or call 1-855-NYMIF33 (1-855-696-4333).Overall Submission requirementsDue to the standardization of provider claims, it is preferable and more expedient if providers acceptpayment directly from the MIF and submit their claims directly to the MIF for reimbursement. If you are amember submitting a claim, please refer to the MIF Claim Submission Guidelines for Members availableon the MIF website.All completed claims are required to be received by the MIF within 90 days from the date services arerendered or purchased.Provider ClaimsoYou are required to submit an IRS Form W9 and a list of providers who will be billing with theTIN/SSN listed on the W9 before payment can be made.oYou can submit your claims electronically or by mail.o Electronically: The Fund offers two options for submitting Electronic Data Interchange(EDI) claims. With the appropriate option in place for your electronic workflow, electronicbilling results in fewer errors, lower costs and increased efficiency for businesses on bothends of the transaction. These options are detailed below: Clearinghouse Submitters: Standard 837 file submission through aclearinghouse using the Fund’s receiver ID, NYDFS. This PIN is the identifierat the Clearinghouse to route claims directly to the Claims OperationDepartment. Direct Submitters: This option is for providers who choose to create their own837 file and submit that file directly to the MIF portal. If you wish to requestonline access, you can send a request via email with your Tax ID and groupNPI to MIF@health.ny.govoMail: Claims that are mailed must be submitted on completed CMS1500 or CMS1450(also known as a UB04). Mail to:Medical Indemnity Fundc/o Public Consulting Group, Inc.P.O. Box 784Greenland, NH 03840-0784Phone: (855) NYMIF33 (855) 696–4333oFor Claims submitted via certified mail, mail to:Medical Indemnity Fundc/o Public Consulting Group, Inc.P.O. Box 784Greenland, NH 03840-0784Note: Photographs and faxes of claims are not acceptable and will not be processed.oLegible, handwritten claims are acceptable; however, typed claims are preferred for more accurate1and expedient processing.MIF@health.ny.gov 1-855-NYMIF33 (1-855-696-4333)
,-llgK ATEIMedicalIndemnity FundMIF Claim Submission GuidanceOctober 2019oCorrect usage of CPT and HCPC procedure codes (and when applicable Revenue and DRGcodes) and ICD10 diagnosis codes. Using miscellaneous codes when there is a specific codeavailable for the service or item being billed will result in a denial and a corrected claim will berequired.oAnesthesia claims require the start and end times of the procedure.oAmbulance and Non Emergency Transportation claims require address of origin and destination.oPlease see Appendix A below for further MIF claims requirements for 1500 Professional Formsand Appendix B below for MIF Claims Requirements for UB Institutional Forms.oSupporting documentation must accompany claims:o Durable Medical Equipment (DME) claims for items that don’t have a specific procedurecode and are billed with a miscellaneous procedure code require a manufacturers invoice(shipping and handling are not covered).o Claims for patients with primary commercial insurance coverage require a copy of theprimary carrier explanation of payment or denial.o All respite and home care efforts require a summary of activities provided to or for themember for each day and/or time-period being billed. Nursing duty notes are acceptable.MIF@health.ny.gov 1-855-NYMIF33 (1-855-696-4333)2
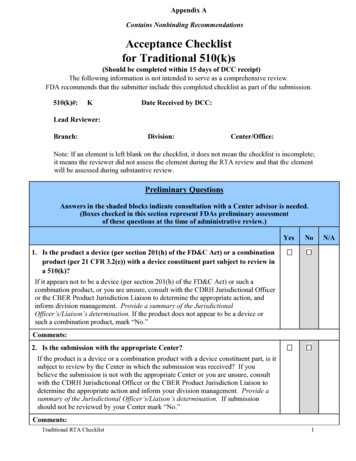
,-llgK ATEIMedicalIndemnity FundMIF Claim Submission GuidanceOctober 2019Appendix A MIF Claims Requirements for 1500 Professional Form: claims received withmissing required elements will be rejectedField #Field NameInstruction11aCarrier TypeInsured’s ID NumberOptionalRequired2Patient’s NameRequired3Patient’s Date of Birth/SexRequired4Insured’s NameOptional5Patient’s AddressRequired6Patient’s Relationship to InsuredOptional789Insured AddressReservedOther Insured’s ptionFormattingRequirement12 alpha numericMMDDYYYYF or M or UOptionalDO NOT USERequired (if box11d is Yes)Other Insured’s Policy or GroupRequired (if boxNumber11d is Yes)ReservedDO NOT USEReservedDO NOT USEInsurance Plan Name or Program Required (if boxName if Applicable11d is Yes)Is Patient’s Condition Related to:EmploymentRequired(if applicable)Auto AccidentRequired(if applicable)Other AccidentRequired(if applicable)ReservedDO NOT USEInsured’s Policy Group or FECA Required(if applicable)NumberInsured’s Date of BirthRequiredMMDDYYYY(if applicable)Other Claim ID designated by Required(if applicable)NUCCInsurance Plan Name or Program Required(if applicable)NameIs there Another Health Benefit RequiredPlan?Patient’s or Authorized Person’s RequiredSignature(MedicalRecords/Information Release) andDateInsured’s or Authorized Person’s RequiredSignature (Assignment of Benefits)Type of InsuranceInsured's MIF ID Number - Enter the member'sMIF number as it appears on the ID card.Enter the member’s name as is indicated on theID card.Patient's Birth date - Enter member's date ofbirth and check the box for male or female.Insured's NamePatient's Address - Enter member’s completeaddress and telephone number.Patient's Relationship to InsuredInsured AddressOther Insured's Information NameOther Insured's Information Policy/GroupNumberOther Insured's Information Employer/SchoolName, Insurance Plan/Program NameCheck Yes or NoCheck Yes or NoCheck Yes or NoInsured's Information - Policy/Group NumberInsured’s Date of BirthInsured's Information - Plan/Program NameCheck Yes or NoSignature and DateInsured's or Authorized Person's SignatureMIF@health.ny.gov 1-855-NYMIF33 (1-855-696-4333)3
,-llgK ATEIMedicalIndemnity FundMIF Claim Submission GuidanceOctober 2019Appendix A MIF Claims Requirements for 1500 Professional Form Continued: claimsreceived with missing required elements will be rejectedField #Field NameInstruction14Date of Current Illness, Injury,Pregnancy, QualifierOptional15Qualifier, First Date of Onset ofSame/Similar IllnessDates Unable to Work in nOptional161717aLegacy Referring17bReferring Physician NPI#18Qualifier/HospitalizationRelated to Current Services19AdditionalClaimdesignated by NUCC20Outside CCYYMMDDYYMMDDCCYYRequired(if applicable)Required(if applicable)Required(if applicable)Dates Optional10 digit numberMMDDYYMMDDCCYYInformation OptionalMMDDYYMMDDCCYYOptionalDescriptionor Date of Current - Illness (First Symptom) ORInjury OR Pregnancy (LMP) - Enter the date ofonset of the member's illness, the date ofaccident/injury or the date of the last menstrualperiod.If patient had same or similar illness give firstdateor Dates Patient Unable to Work in CurrentOccupationName of Referring Provider or Other Source Enter the full name of the Referring Provider. Areferring/ordering provider is one who requestsservices for a member, such as gical tests, physical or other therapies,pharmaceuticals or durable medical equipment.ID Number of Referring Physician - Enter StateMedical License number.Enter Referring Provider's NPI number.or Hospitalization Dates Related to CurrentServices - Enter the date of hospital admissionand discharge if the services billed are related tohospitalization. If the patient has not beendischarged, leave the discharge date blank.Reserved for Local Use - Use this area foror procedures that require additional information,justification or an Emergency CertificationStatement. This section may be used for an unlistedprocedure code when explanation is requiredand clinical review isrequired. If modifier “-99” multiple modifiers is enteredin section 24d, they should be itemized in thissection. All applicable modifiers for each lineitem should be listed. Claims for “By Report”codes and complicated procedures should bedetailed in this section if spacepermits. All multiple procedures that could bemistaken for duplicate services performedshould be detailed in thissection. Anesthesia start and stop times. Itemizationof miscellaneous supplies, etc.Check "yes" when diagnostic test wasperformed by any entity other that the providerbilling the service. If this claim includes chargesfor laboratory work performed by a licensedlaboratory, enter and "X". "Outside Laboratoryrefers to a laboratory not affiliated with thebilling provider. State in Box 19 that a specimenwas sent to an unaffiliated laboratory.MIF@health.ny.gov 1-855-NYMIF33 (1-855-696-4333)4
,-llgK ATEIMedicalIndemnity FundMIF Claim Submission GuidanceOctober 2019Appendix A MIF Claims Requirements for 1500 Professional Form Continued: claimsreceived with missing required elements will be rejectedField #Field NameInstruction21Diagnosis or Nature of Illness or RequiredInjury22Resubmission Code:Requiredforcorrectionorvoiding of a claimonly23Prior Authorization Number24aDate of Service, From and ToRequired(if applicable)Required24bPlace of ServiceRequired24c24dEmergency ServiceProcedures, Services or SupplyCode including modifiers ifapplicable NDC numbersOptionalRequired24eDiagnosis PointerRequired24fChargesRequired24gDays or UnitsRequiredFormattingRequirement10 digit AlphaNumericMMDDYY orMMDDYYYY2 digit numberDescriptionEnter all letters and/or numbers of the ICD-10code for each diagnosis, including fourth andfifth digits if present. The first diagnosis listedin section 21.1 indicates the primary reason forthe service providedEnter:7 for a corrected claim8 for a voided claimANDOriginal Reference Code:Enter the Claim ID number of the claim you arerequesting to correct or void.Both Data elements above are required.Enter prior authorization or referral number.Enter the date the service was rendered in the“from” and “to” boxes in the MMDDYYformat. If services were provided on only onedate, they will be indicated only in the “from”column. If the services were provided onmultiple dates (i.e., DME rental, hemodialysismanagement, radiation therapy, etc), the rangeof dates and number of services should beindicated. “To” date should never be greaterthan the date the claim is received by the HealthPlan.Enter one code indicating where the service wasrendered.Check box and attach required documentation.Enter the applicable CPT and/or HCPCSNational codes in this section. Modifiers, whenapplicable, are listed to the right of the primarycode under the column marked “modifier”. Ifthe item is a medical supply, enter the two-digitmanufacturer code in the modifier area after thefive-digit medical supply code. Reminder:Payment modifiers should be in first position.Enter the diagnosis code number from box 21that applies to the procedure code indicated in24D.Enter the charge for service in dollar amountformat. If the item is a taxable medical supply,include the applicable state and county sales tax.Enter the number of medical visits orprocedures, units of anesthesia time, oxygenvolume, items or units of service, etc. Do notenter a decimal point or leading zeroes. Do notleave blank as units should be at least 1.MIF@health.ny.gov 1-855-NYMIF33 (1-855-696-4333)5
,-llgK ATEIMedicalIndemnity FundMIF Claim Submission GuidanceOctober 2019Appendix A MIF Claims Requirements for 1500 Professional Form Continued: claimsreceived with missing required elements will be rejectedField #Field NameInstruction24hEPSDT Family PlanOptional24i24j25ID QualifierProvider ID Number TaxonomyRendering Provider NPI NumberFederal Tax ID NumberOptionalOptionalRequiredRequired10 alpha numeric10 digit number9 digit number26Patient’s Account NumberRequiredLength 20 max.2728Accept AssignmentTotal ChargeRequiredRequired29Amount PaidRequired(if applicable)3031ReservedSignature of Practitioner orSupplier and DateDO NOT USERequired32Service Facility Location/Location Requiredwhere services were rendered32aService Facility NPI if differentfrom Billing Provider NPIOther IDRequired(if applicable)Optional33Billing Provider/Supplier’s Name,Address, & Telephone Number asit appears on your W-9Required33ABilling Provider/Supplier’sNumberOther ID32b33bNPI RequiredOptionalDescriptionFormattingRequirement10 digit number10 digit numberEnter code “1” or “2” if the services renderedare related to family planning (FP). Enter code“3” if the services rendered are Child Health andDisability Prevention (CHDP) screening relatedEnter “X” if billing for emergency services.Enter the Rendering Provider's NPI numberEnter the Federal Tax ID for the billingprovider.Enter the patient’s medical record number oraccount number in this field. This number willbe reflected on Explanation of Benefits (EOB) ifpopulated.Check Yes or NoEnter the total for all services in dollar andcents. Do not include decimals. Do not leaveblank.Enter the amount of payment received from theOther Health Coverage or member. Enter thefull dollar amount and cents. Do not enterMedicare payments in this box.The claims must be signed and dated by theprovider or a representative assigned by theprovider in black pen. An original signature ispreferred. Stamps are also acceptable. Initialsand other facsimiles are not acceptable.Enter the provider name. Enter the provideraddress, without a comma between the city andstate, and a nine-digit zip code, without ahyphen. Enter the telephone number of thefacility where services were rendered, if otherthan home or office.Enter the NPI of the facility where the serviceswere rendered.Enter the provider number for an atypicalservice facility.Enter the provider name. Enter the provideraddress, without a comma between the city andstate, and a nine-digit zip code, without ahyphen. Enter the telephone number.Enter the billing provider’s NPI.Used for atypical providers only. Enter theprovider number for the billing provider.MIF@health.ny.gov 1-855-NYMIF33 (1-855-696-4333)6
,-llgK ATEIMedicalIndemnity FundMIF Claim Submission GuidanceOctober 2019Appendix B MIF Claims Requirements for UB Institutional Forms: claims received withmissing required elements will be rejectedField #123a3bField NameProviderName,Address, and PhonePay-to Name, addressandSecondaryIdentification FieldsPatient Control NumberRequired(If different than 1)DescriptionFormattingRequirementDo not use P.O. Enter the provider name, address and zip codeboxesand telephone number this section.Enter the provider name, address and zip codeand telephone number this section.RequiredLength 20 max.RequiredRecord Optional4Medical/HealthNumberType of Bill5Federal Tax Number6InstructionPay-to-provider Billing ProviderStatementCoversPeriod (From-Through)Required4 digit codeRequired9 digit number.RequiredMMDDYYThis number is reflected on the Explanation ofBenefits for reconciling payments ifpopulated.This number will not be reflected on EOB ifpopulated.Enter the appropriate four-character type ofbill code.Enter the Federal Tax ID for the billingfacility.Enter the “From” and “Through” dates ofservices covered on the claim if claim is forinpatient services.78aNot UsedPatient’s NameDO NOT USERequired8bPatient IdentifierRequiredEnter patient’s last name, first name andmiddle initial if known.9a-eRequiredEnter Patient Address10Patient’sAddress,State, and Zip CodePatient’s Date of BirthRequiredMMDDYYYYEnter the patient’s date of birth in an eightdigit format, Month, Date, Year(MMDDYYYY) format.11Patient’s SexRequiredF or M12Admission DateRequired(if applicable)MMDDYYUse the capital letter “M” for male, or “F” forfemale.Enter in a six-digit format (MMDDYY), enterthe date of hospital admission.13Admission HourRequired(if applicable)14Type of AdmissionRequiredEnter patient’s name in 8bMilitaryStandard Time(00-23)Singledigitcode: 1-9Enter hour of patient's admission.Enter the numeric code indicating thenecessity for admission to the hospital. 1 Emergency 2 – ElectiveMIF@health.ny.gov 1-855-NYMIF33 (1-855-696-4333)7
,-llgK ATEIMedicalIndemnity FundMIF Claim Submission GuidanceApril 2019Appendix B MIF Claims Requirements for UB Institutional Forms Continued: claimsreceived with missing required elements will be rejectedField #Field NameInstruction15Source of AdmissionRequired16Discharge HourRequired(if applicable)1718-28Patient StatusCondition Codes IfApplicable Type ofAdmissionAccident StateRequiredRequired(if applicable)29Optional3031-34Not UsedDO NOT USEOccurrence Codes and Required(if applicable)Dates35-36Occurrence Span Codesand DatesNot UsedResponsiblePartyName and AddressRequired(if applicable)DO NOT USERequired(if applicable)Value Codes andAmountsRevenue CodeRequired(if tSingle code: 1-9;A-ZMilitaryStandard Time(00-23)DescriptionIf the patient was transferred from anotherfacility, enter the numeric code indicating thesource of transfer.1 - Non-Healthcare Facility Point of Origin 2– Clinic 4 - Transfer from a Hospital(Different Facility) 5 - Transfer from a SkilledNursing Facility (SNF) or Intermediate CareFacility (ICF) 6 - Transfer from AnotherHealthcare Facility 7 - Emergency Room 8 Court/Law Enforcement 9 - Information NotAvailable B - Transfer from AnotherHealthcare Facility C - Readmission to thesame Home Health Agency D - Transfer fromone distinct unit of the hospital to anotherdistinct unit of the same hospital resulting in aseparate claim to the payer E - Transfer fromAmbulatory Surgery Center F - Transfer fromHospice and is under a hospice plan of care orenrolled in a hospice programEnter the discharge hour. For Inpatient only.Enter Patient Discharge Status2 alphaabbreviationIf visit or stay is related to an accident, enterin which state accident occurred.MMDDYYYYEnter the codes and associated dates thatdefine the significant even related to the claim.Occurrence Codes covered by SFHP: 01 Auto Accident 02 - No Fault InsuranceInvolvement - Including Auto Accident/Other03 - Accident/Tort Liability 04 - EmploymentRelated 05 - Other Accident 06 - CrimeVictimEnter Occurrence Span Codes and DatesMMDDYYYYEnter the name and address of the partyresponsible for payment if different fromname in box 50Enter Value Codes and Amounts4 digit codeEnter the four-digit revenue code for theservices provided, e.g. room and board,obstetrics, etc.MIF@health.ny.gov 1-855-NYMIF33 (1-855-696-4333)8
,-llgK ATEIMedicalIndemnity FundMIF Claim Submission GuidanceApril 2019Appendix B MIF Claims Requirements for UB Institutional Forms Continued: claimsreceived with missing required elements will be rejectedField #Field NameInstruction43Revenue DescriptionRequired(if applicable)44CPT/HCPCS onlyRequired(if applicable)45Service DatesRequired46Units of ServiceRequired4748n/an/a4950a-c51a-cTotal ChargesNon-covered ChargesCreation DateTotalsNot UsedPayer NameNational Health PlanIdentifierRelease of InformationCertification IndicatorAssignment of BenefitsCertification IndicatorPrior PaymentsRequiredOptionalRequiredRequiredDO NOT c59a-c60a-c61a-c62a-c63a-cEstimated AmountNational Provider ID(NPI)Other Provider IDInsured’s NameDescriptionFormattingRequirementMMDDYYYYEnter the description of the particular revenuecode in box 42 or HCPCS code in box44. Include NDC/UPN Codes here, whenapplicable.Enter the applicable HCPCS codes andmodifiers. For outpatient billing do not bill acombination of HCPCS and Revenue codes onthe same claim form. When billing forprofessional services, use CMS 1500 form.Enter the service date in MMDDYY formatfor outpatient billing.Enter the actual number of times a singleprocedure or item was performed or providedfor the date of service.Enter Total Charges (By Rev. Code)Enter Non-Covered ChargesEnter Health Plan IDRequiredCheck Yes or NoRequiredCheck Yes or NoRequired ifApplicableOptionalRequiredEnter any prior payments received from OtherCoverage in full dollar amount.Enter Estimated Amount DueEnter NPI numberOptionalRequiredPatient’s Relationshipto InsuredInsured’s Unique IDRequiredInsurance Group NameInsurance GroupNumberTreatmentAuthorization CodeOptionalOptionalRequiredOptional10 digit number10 digit number12 alphanumericEnter Other Provider IDsEnter the mother’s name if billing for an infantusing the mother’s ID. If any othercircumstance, leave blank.Enter “03” (child) if billing for an infant usingthe mother’s Identification NumberEnter the patient’s 12-digit MIF ID number asit appears in the member’s ID card.Enter Insured Group NameEnter Insured Group NumberEnter any authorizations numbers in thissection. It is not necessary to attach a copy ofthe authorization to the claim. Memberinformation from the authorization mustmatch the claim.MIF@health.ny.gov 1-855-NYMIF33 (1-855-696-4333)9
,-llgK ATEIMedicalIndemnity FundMIF Claim Submission GuidanceApril 2019Appendix B MIF Claims Requirements for UB Institutional Forms Continued: claimsreceived with missing required elements will be rejectedField #646566Field NameInstructionforDocumentControl Requiredcorrection orNumber (DCN)voiding of a claimonlyEmployer NameOptionalDiagnosisand Required10 digit n the Type of Bill in box 4 ends in a 7 oran 8 enter the Claim ID number of the claimyou are requesting to correct or void. This canbe found on your Remittance AdviceEnter Employer NameEnter:0—ICD-10-CM DiagnosisRequiredEnter all letters and/or numbers of the ICD-9or 10 CM code for the primary diagnosisincluding the fourth and fifth digit if presentEnter all letters and/or numbers of thesecondary ICD-9 or 10 CM code includingfourth and fifth digits if present.67PrincipleCode67A-QOther Diagnosis Code Required(including POA Codes) (if applicable)6869Not UsedAdmitting Diagnosis70A-CPatient’s Reason forVisitProspective PaymentSystem (PPS) CodeExternal Cause ofInjury (ECI) CodeNot UsedPrincipleProcedureCodes and DateOther Procedure Codesand DatesNot UsedAttendingProviderName and Identifiers(including NPI)OperatingProviderName and Identifiers(including NPI)Other Provider Nameand Identifiers(including NPI)RemarksCode to Code mattingRequirementDiagnosisDO NOT USERequired(if applicable)Required(if applicable)Optional10 digit alphanumeric10 digit alphanumeric10 digit alphanumeric10 digit alphanumericEnter Admitting Diagnosis CodeEnter Patient's Reason for Visit CodeEnter PPS Code10 digit alphanumericEnter External Cause of Injury CodeMMDDYYYYEnter Principal Procedure Code/DateMMDDYYYYEnter Other Procedure Code/Date10 digit numberEnter Attending Name/ ID-Qualifier 1GRequired(if applicable)10 digit numberEnter Operating IDRequired(if applicable)10 digit numberEnter Other IDOptionalDO NOT USERequired(if applicable)Required(if applicable)DO NOT USERequired(if applicable)OptionalOptionalEnter RemarksEnter Code-Code Field/QualifiersMIF@health.ny.gov 1-855-NYMIF33 (1-855-696-4333)10
All completed claims are required to be received by the MIF within 90 days from the date services are rendered or purchased. Provider Claims . o You are required to submit an IRS Form W9 and a list of providers who will be billing with the TIN/SSN listed on the W9 before payment can be made. o You can submit