Transcription
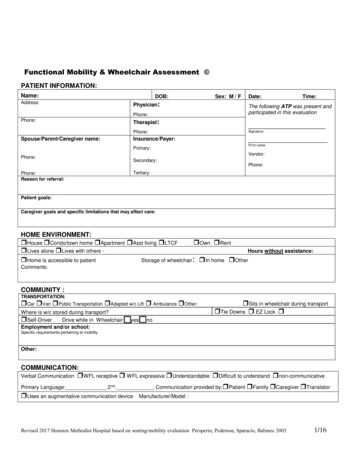
Functional Mobility & Wheelchair Assessment PATIENT ne:Therapist:Spouse/Parent/Caregiver name:Sex: M / FDate://Time:The following ATP was present andparticipated in this rint ason for referral:Patient goals:Caregiver goals and specific limitations that may affect care:HOME ENVIRONMENT: House Condo/town home Apartment Asst living LTCF Own Rent Lives alone Lives with others Hours without assistance: Home is accessible to patientStorage of wheelchair: In home OtherComments:COMMUNITY :TRANSPORTATION: Car Van Public Transportation Adapted w/c Lift Ambulance Other:Where is w/c stored during transport? Self-Driver Drive while in WheelchairEmployment and/or school: Sits in wheelchair during transport Tie Downs EZ Lock yes noSpecific requirements pertaining to mobilityOther:COMMUNICATION:Verbal Communication WFL receptive WFL expressive Understandable Difficult to understand non-communicativePrimary Language: 2 nd: Communication provided by: Patient Family Caregiver Translator Uses an augmentative communication deviceManufacturer/Model :Revised 2017 Houston Methodist Hospital based on seating/mobility evaluation Presperin, Pederson, Sparacio, Babinec 20031/16
Name:MR#:MEDICAL HISTORY:Diagnosis:DiagnosisDiagnosisPrimary Diagnosis:Onset:Diagnosis:Code:DiagnosisCode: Progressive diseaseRelevant future agnosis:Code:Explain recent changes or trends in weight:History:Cardio Status:Functional Limitations: Intact ImpairedRespiratory Status:Functional Limitations: Intact Impaired SOB COPD O2 Dependent LPM Ventilator DependentResp equip:Objective Measure(s):Orthotics: Amputee: Prosthesis:MOBILITY/BALANCE:Sitting BalanceStanding Balance WFL Uses UE for balance in sitting WFL Uses UE/device for stabilityComments:Comments:Transfers Independent Min assistAmbulation Independent Ambulates independently withdevice: Mod assist Able to ambulate feet Max assist Non-functional ambulatorsafely/functionally/independently Min assist Min assistHistory/High risk of falls Mod assist Max assist Unable Mod assist Max assist Unable Dependent Unable to ambulateTransfer method: 1 person 2 person sliding board squat pivot stand pivot mechanical patient lift other:Fall History: # of falls in the past 6 months? # of “near” falls in the past 6 months?CURRENT SEATING / MOBILITY:Current Mobility Device: None Cane/Walker Manual Dependent Dependent w/ Tilt Scooter Power (type of control):Manufacturer:Model:Serial #:Size:Color:Age:Purchased by whom:Current condition of mobility base:Current seating system:Age of seating system:Describe posture in present seating system:Is the current mobility meeting medical necessity?: Yes NoDescribe:Revised 2017 Houston Methodist Hospital based on seating/mobility evaluation Presperin, Pederson, Sparacio, Babinec 20032/16
Name:MR#:Ability to complete Mobility-Related Activities of Daily Living (MRADL’s) with Current Mobility Device:Move room to roomMeal prepFeedingBathingGroomingUE dressingLE dressingToileting Independent Independent Independent Independent Independent Independent Independent Independent Min Mod Max assist Min Mod Max assist Min Mod Max assist Min Mod Max assist Min Mod Max assist Min Mod Max assist Min Mod Max assist Min Mod Max assist Unable Unable Unable Unable Unable Unable Unable UnableComments:Bowel Mgt: Continent Incontinent Accidents Diapers Colostomy Bowel ProgramBladder Mgt: Continent Incontinent Accidents Diapers Urinal Intermittent Cath Indwelling Cath Supra-pubic CathEQUIPMENT TRIALS:Cane/CrutchesWalker / Rollator NAManual WheelchairK0001-K0007:Does not meet mobility needs due to:Mark all boxes that indicate inability to use the specific equipment listedMeets needsfor safeindependentfunctionalambulation /mobilityRisk ofFallingorHistoryof FallsEnviromentallimitations SafetyconcernswithphysicalabilityDecreased /limitationsendurance& strengthDecreased /limitationsmotor skills&coordinationPainPace /SpeedCardiacand/orrespiratoryconditionContra –indicatedby diagnosis Cognition NAManual W/C (K0005)with power assist NAScooter NAPower Wheelchair:standard joystick NAPower Wheelchair:alternative controls NASummary:The least costly alternative for independent functional mobility was found to be: Crutch/Cane Walker Manual w/c Manual w/c with power assist Scooter Power w/c std joystick Power w/c alternative control Requires dependent care mobility deviceFunctional Processing Skills for Wheeled MobilityProcessing skills are adequate for safe mobility equipment operation Yes NoPatient is willing and motivated to use recommended mobility equipment Yes No Patient is unable to safely operate mobility equipment independently and requires dependent care equipmentComments:Revised 2017 Houston Methodist Hospital based on seating/mobility evaluation Presperin, Pederson, Sparacio, Babinec 20033/16
Name:MR#:Patient TION and SKIN ISSUES:Sensation Intact Impaired Absent Hyposensate Hypersensate DefensivenessLocation(s) of impairment:Pressure Relief Method(s): Lean side to side to offload Stand up (without risk of falling)(without risk of falling) W/C push up (4 times/hour for 15 seconds) Other: (Describe)Effective pressure relief method(s) above can be performed consistently throughout the day: Yes NoIf not, Why?Pressure Map Results: The above method(s) provided effective pressure relief - Yes NoSkin Issues/Skin IntegrityHistory of Skin Issues Yes NoHx of skin flap surgeriesCurrent skin Issues Yes No Intact Red area Open area Scar tissue At risk from prolonged sittingWherePain: Yes No Yes NoWhereWhereWhenWhenStageLocation(s): Intensity scale: (0-10)How does pain interfere with mobility and/or MRADLs? -Revised 2017 Houston Methodist Hospital based on seating/mobility evaluation Presperin, Pederson, Sparacio, Babinec 20034/16
Braden Scale For Predicting Pressure Sore Risk Risk FactorScore/DescriptionSENSORY 1. COMPLETELY LIMITED 2. VERY LIMITED – 3. SLIGHTLY LIMITED –PERCEPTIONAbility to respondmeaningfully topressure-relateddiscomfortMOISTUREDegree to whichskin is exposed tomoistureACTIVITYAbility to changeand control bodypositionNUTRITIONUsual food intakepattern 1NPO:Nothing by mouth.2IV: Intravenously.3TPN: Totalparenteralnutrition.FRICTIONAND SHEAR0OR limited ability to feel painover most of body surfaceResponds to verbalcommands but cannot alwayscommunicate discomfort orneed to be turned, OR hassome sensory impairmentwhich limits ability to feel painor discomfort in 1 or 2extremities.IMPAIRMENT –Responds to verbalcommands. Has nosensory deficit whichwould limit ability tofeel or voice pain ordiscomfort. 1. CONSTANTLY 2. OFTEN MOIST – Skin 3. OCCASIONALLY 4. RARELYMOIST– Skin is kept moistis often but not always moist.Linen must be changed at leastonce a shift.MOIST – Skin isMOIST – Skin isoccasionally moist, requiringan extra linen changeapproximately once a day.usually dry; linen onlyrequires changing atroutine intervals. 1. BEDFAST – Confined to 2. CHAIRFAST – Ability 3. WALKS 4. WALKSbedto walk severely limited ornonexistent. Cannot bear ownweight and/or must be assistedinto chair or wheelchairOCCASIONALLY – WalksFREQUENTLY–occasionally during day, butfor very short distances, withor without assistance. Spendsmajority of each shift in bed orchair.Walks outside theroom at least twice aday and inside room atleast once every 2hours during wakinghours. 1. COMPLETELY 2. VERY LIMITED – 3. SLIGHTLY 4. NOIMMOBILE – Does not makeLIMITED – Makes frequentLIMITATIONS –even slight changes in body orextremity position withoutassistance.Makes occasional slightchanges in body or extremityposition but unable to makefrequent or significant changesindependentlythough slight changes in bodyor extremity positionindependentlyMakes major andfrequent changes inposition withoutassistance. 1. VERY POOR – Never 2. PROBABLY 3. ADEQUATE – Eats 4. EXCELLENTeats a complete meal. Rarelyeats more than 1/3 of any foodoffered. Eats 2 servings or lessof protein (meat or dairyproducts) per day. Takes fluidspoorly. Does not take a liquiddietary supplement,INADEQUATE – Rarely eatsover half of most meals. Eatsa total of 4 servings of protein(meat, dairy products) eachday. Occasionally refuses ameal, but will usually take asupplement if offered,– Eats most of everyOR is NPO1 and/or maintainedon clear liquids or IV2 for morethan 5 daysOR receives less than optimumamount of liquid diet or tubefeeding.OR is on a tube feeding orTPN3 regimen, whichprobably meets most ofnutritional needs. 1. PROBLEM- Requires 2. POTENTIAL 3. NO APPARENTmoderate to maximumassistance in moving. Completelifting without sliding againstsheets is impossible. Frequentlyslides down in bed or chair,requiring frequent repositioningwith maximum assistance.Spasticity, contractures, oragitation leads to almostconstant friction.PROBLEM– Moves feebly orPROBLEM – Moves in bedrequires minimum assistance.During a move, skin probablyslides to some extent againstsheets, chair, restraints, orother devices. Maintainsrelatively good position in chairor bed most of the time butoccasionally slides down.and in chair independentlyand has sufficient musclestrength to lift up completelyduring move. Maintains goodposition in bed or chair at alltimes.almost constantly by perspiration,urine, etc. Dampness is detectedevery time patient is moved orturned.a complete meal and generallyeats only about ½ of any foodoffered. Protein intake includesonly 3 servings of meat or dairyproducts per day. Occasionallywill take a dietary supplementSource: Barbara Braden and Nancy Bergstrom. Copyright, 1988. Reprinted with permission. All rights reservedBraden Scale Score: 4. NOResponds only to painfulstimuli. Cannot communicatediscomfort except by moaningor restlessness, OR has asensory impairment which limitsthe ability to feel pain ordiscomfort over ½ of body.Unresponsive (does not moan,flinch, or grasp) to painful stimuli,due to diminished level ofconsciousness or sedation,Degree of physicalactivityMOBILITYScore0000meal. Never refuses ameal. Usually eats atotal of 4 or moreservings of meat anddairy products.Occasionally eatsbetween meals. Doesnot requiresupplementation.0Total Very High Risk 6-9 High Risk 10-12 Moderate Risk 13-14 Mild Risk 15-18 No Risk 19-23Barbara Braden & Nancy Bergstrom, Copyrighted 1988. Reprinted with permission. All rights reserved.5/160
MAT EVALUATION:Neuro-Muscular Status: (Tone, Reflexive, Responses, etc.) Intact Spasticity: Hypotonicity Fluctuating Muscle Spasms Poor Righting Reactions/Poor Equilibrium Reactions Primal Reflex(s):Comments:POSTURE:COMMENTS:Anterior / PosteriorPELVIS Neutral PosteriorAnterior Fixed – No movement Tendency away from neutral Flexible Self-correction External correctionTRUNK WFLWFL ThoracicKyphosis LumbarLordosis Fixed – No movement Tendency away from neutral Flexible Self-correction External correction Functional Flexed Extended Rotated R Lat flexed R Rotated L Lat flexed L Cervical Hyperextension R obliquity L obliquity(L elev)(R elev) Fixed – No movement Tendency away from neutral Flexible Self-correction External correctionAnterior / Posterior HEAD&NECKObliquity (viewed from front) WFLConvexConvexLeftRight C-curve S-curve Multiple Fixed – No movement Tendency away from neutral Flexible Self-correction External correction Good head control Adequate head control Limited head control Absent head control Normal Flaccid Low toneWFLRightLeft SpasticityAnterior Anterior Dystonia Pelvic thrust Fixed – No movement Tendency away from neutral Other: Flexible Self-correction External correctionRotation-shoulders and Tonal InfluenceTrunk:upper trunkLeft Right Rotation-PelvisTonal InfluencePelvis: Neutral Left-anterior Right-anterior Fixed – No movement Tendency away from neutral Flexible Self-correction External correction Normal Flaccid Low tone Spasticity Dystonia Other:Describe Tone/Movement of head and neck:Revised 2017 Houston Methodist Hospital based on seating/mobility evaluation Presperin, Pederson, Sparacio, Babinec 20036/16
Name:MR#:PositionWindsweptHip R.O.M / StrengthWFLHIPS Neutral ABductADduct Subluxed Dislocated Fixed – No movement Tendency away from neutral Flexible Self-correction External correctionKnee R.O.M.RightLeftKNEES&FEET WFL Limitations Neutral Right WFL WFL Limitations R L R L R L R L R LPlantar FlexedWrist&HandFlex Grade R / 5 L / 5Dorsi Grade R / 5 L / 5Ext Grade R / 5Plantar Grade R /5 L / 5L / 5SHOULDERSTendency Towards:Right Functional Elevation Depression Protraction Retraction Int-rotation Ext-rotation SubluxedHip FlexR /5 L /5Hip ExtR /5 L /5Hip ABdR /5 L /5Hip ADdR /5 L /5 1 Barely detectable impression when finger ispresssed into skin. 2 Slight indentation.15 seconds to rebound 3 Deeper indentation.30 seconds to rebound. 4 30 seconds to rebound.R.O.M and Strength for UE:WFLLeftRightLimits Shlder Flex Shlder ABd Shlder ADd Elbow Flex Elbow ExtTone/Movement ofLeftLimitsR/L StrengthR /5 L /5R /5 L /5R /5 L /5R /5 L /5R /5 L /5WNLLimitationsContracturesFistingTremorsWeak graspPoor dexterityHand movementnon-functionalParalysis Normal Flaccid Low tone Spasticity Dystonia Other: Edema UE 1 2 3 4 Describe:Comments:Handedness: Right Left NAComments:R/L Strength Normal Low tone Spasticity Flaccid Dystonia Rocks/Extends at hip Thrust into knee extension Pushes legs
pattern 1NPO: Nothing by mouth. 2IV: Intravenously. 3TPN: Total parenteral nutrition. OR 1. VERY POOR – Never eats more than 1/3 of any food offered. Eats 2 servings or less of protein (meat or dairy products) per day. Takes fluids poorly. Does not take a liquid dietary supplement, is NPO1 and/or maintained on clear liquids or IV2 for more