Transcription
Use of the Functional Movement Screen TM Corrective Exercises to Address StrengthDeficits in a 55 Year Old Female Status Post L5-S1 DiscectomyA Capstone Project for PTY 768Presented to the Faculty of the Department of Physical TherapySage Graduate SchoolIn Partial Fulfillmentof the Requirements of the Degree ofDoctor of Physical TherapyHannah SolomonMay, 2010Approved:Gabriele Moriello, PT, PhD, MS, GCSResearch AdvisorMarjane Selleck, PT, DPT, MS, PCSProgram Director, Doctor of Physical Therapy Program
Use of the Functional Movement Screen TM Corrective Exercises to Address StrengthDeficits in a 55 Year Old Female Status Post L5-S1 DiscectomyA Capstone Project for PTY 768Presented to the Faculty of the Department of Physical TherapySage Graduate SchoolIn Partial Fulfillmentof the Requirements of the Degree ofDoctor of Physical TherapyHannah SolomonMay, 2010Approved:Gabriele Moriello, PT, PhD, MS, GCSResearch AdvisorMarjane Selleck, PT, DPT, MS, PCSProgram Director, Doctor of Physical Therapy Program
SAGE GRADUATE SCHOOLI hereby give permission to Sage Graduate School to use my work,Use of the Functional Movement Screen TM Corrective Exercises to Address StrengthDeficits in a 55 Year Old Female Status Post L5-S1 DiscectomyFor the following purposes:-Place in the Sage Colleges Library collection and reproduce for Interlibrary Loan.-Keep in the Program office or library for use by students, faculty,or staff.-Reproduce for distribution to other students, faculty, or staff.-Show to other students, faculty or outside individuals, such as accreditorsor licensing agencies, as an example of student work.-Use as a resource for professional or academic work by faculty or staff.Hannah SolomonMay, 20010
I represent to The Sage Colleges that this project and abstract are the original work of theauthor, and do not infringe on the copyright or other rights of others.Use of the Functional Movement Screen TM Corrective Exercises to Address StrengthDeficits in a 55 Year Old Female Status Post L5-S1 DiscectomyHannah SolomonMay, 2010
Use of the Functional Movement Screen TM Corrective Exercises toAddress Strength Deficits in a 55 Year Old Female Status Post L5-S1DiscectomyHannah Solomon, SPT
AbstractBackground and Purpose: This case report describes the use of the Functional MovementScreen (FMS) corrective exercises in addition to a traditional strengthening andrehabilitation program in the treatment of a 55 year old female status post L5-S1 discectomy.The aim of this case report was to determine if the FMS corrective exercises in addition to atraditional rehabilitative program are useful in increasing trunk strength and stability,flexibility, ROM, and ADL’s in a person post L5-S1 lumbar discectomy. Case Description:The individual in this case report is a 55 year old female department of transportation laborer.She received outpatient physical therapy 3 times per week for a duration of 11 weeks. Adynamic strengthening program was provided using several of the FMS corrective exercisesin conjunction with other exercises to provide a comprehensive rehabilitative program thatfocused on improving strength and return to work. Outcomes: At the completion of treatmentimprovements were noted in strength, flexibility, activities of daily living, and special andfunctional testing. Her lower body strength improved from 0.5 to 1.5 manual muscle testinggrades and trunk range of motion improved from 20% to 55%. She also had significantimprovements in ADL’s such as tolerance to sitting, walking, and bending at the trunk yetwas not able to return to work. She was discharged to a local fitness club. Discussion: Thefindings suggest that FMS corrective exercises when used in adjunct to a traditionaltreatment program may be useful in the rehabilitation of individuals status post L5-S1discectomy. However further experimental research is needed utilizing the correctiveexercises to determine the efficacy and usefulness of the FMS corrective exercises in thephysical therapy setting.
IntroductionLumbar disc herniations are the most common cause of lumbar radiculopathy. InNorth America, lumbar disc herniations affect 1% to 2% of the population,1 with ninety-fivepercent occurring in one of the lower intervertebral discs.2 A disc herniation at the level ofL5 and S1 affects the corresponding nerve roots resulting in sciatica, bowel and bladderdysfunction, postural control, and lower extremity impairments.3,4Discectomies are currently the most frequently utilized surgical intervention toaddress spinal nerve and nerve root compression resulting from intervertebral disc herniation.Surgical intervention has been reported in 2% to 10% of people with lumbar disc herniation,with approximately 200,000 discectomies performed annually in North America.1 A study byLurie et al3 explored the differences in outcomes over a 2 year period between upper andlower lumbar spine discectomies finding that individuals with upper spine discectomies (L2L3 and L3-L4) had better outcomes after surgical procedure as compared to lower spinediscectomies (L4- L5 and L5-S1). Outcomes in individuals with lower spine discectomieswere worse in all aspects of treatment after surgery with regards to pain, quality of life, anddisability after operative treatment.Following surgery, residual sciatic pain is reported by 10% to 30% of individuals,5whereas residual back pain is reported by 30% to 40%.6,7 Only 80% of those havingundergone discectomy return to work within 12 months after surgery.8,9 Approximately halfof those who undergo disc herniation experience a preoperative as well as postoperativereduction of muscle strength and endurance corresponding to the affected nerve rootdistribution which is one of the reasons that the return to work rate is so low after undergoingdiscectomy surgery.2,10,11 The aforementioned low return to work rate after surgical3
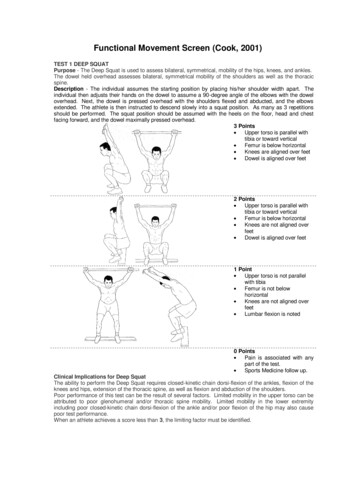
discectomy implicates the necessity for an intense and comprehensive rehabilitative programfor return to work and functional independence.The Functional Movement ScreenTM (FMS) is an assessment tool developed by GrayCook and Lee Burton as a screening tool for fitness professionals such as physical therapistsand athletic trainers to gather objective data on human movement patterns during theperformance of functional activities for injury prevention. It is also widely used in manycolleges and professional sports teams for injury prevention in athletes. Each of the testingcriteria in the FMS was created to exacerbate the individual’s compensatory movementpatterns, allowing for easy identification by the examiner. By identifying movement flaws itis expected that fitness professionals can assist individuals by preventing eventual breakdownand trauma during activity.12 One study by Hoover et al13 found that the FMS’ specificity forinjury prediction was 97.2% in a sample of 49 recreational runners training for a halfmarathon.The FMS consists of 7 fundamental movement tests to identify abnormal movementpatterns and impaired mobility and stability. The 7 testing categories consist of a deep squat,hurdle step, in-line lunge, shoulder mobility, active straight leg-raise, trunk stability push-up,and rotary stability. Scoring is performed on a 0 to 3 point system. A score of zero is given ifthe individual has pain at any point during the movement; a 1 is given if the individual isunable to be complete the activity even with compensations; a 2 is given if the individual isable to perform the movement but uses poor mechanics or compensatory methods; and a 3 isgiven if the individual can perform the movement without any compensations.12 Three of thetests: shoulder mobility, trunk stability push-up, and rotary stability have clearing testsassociated with them that are pass/fail to determine if the actual FMS tests in these sections is4
safe to perform. For example, the clearing test for the trunk stability push up test is a pronepress up. If the press up elicits pain in the individual, a score of zero is given for that sectionof the screen the trunk stability push up test is not attempted.Corrective exercises were also developed as a supplement to the FMS. The correctiveexercises are based on dysfunction in the dynamic motor learning, mobility and movement,stability and static exercise categories. The exercises then coordinate to specific movementdysfunction that the individual displays during the testing scenarios. The corrective exercisesdeveloped to accompany the FMS are based on incorporating proprioceptive neuromuscularfacilitation (PNF) and motor learning.14,15 At this time there is no research available tosupport these corrective exercises however PNF and motor learning are both well establishedand accepted principles for rehabilitation.PNF exercises were developed to enhance the body’s neuromuscular responsethrough stimulating proprioceptors in the joint. PNF movement patterns are performed on adiagonal and often have a spiral component. The usage of PNF patterns has been suggestedto allow muscle strengthening in functional movements patterns such as those found in sportsand daily activities.16 Kofotolis et al16 utilized both static and dynamic PNF exerciseprograms in women with chronic low back pain. Finding that both methods of PNF trainingwere highly effective in decreasing back pain, improving trunk musculature strength andendurance and decreasing disability as measured by the Oswestry disability index. PNFexercises are also widely used in rehabilitative programs in both the upper and lowerextremities in addition to the trunk and have been demonstrated to be an effective method ofstrengthening and gaining flexibility.17,185
Motor learning is defined as "a set of processes associated with practice or experienceleading to relatively permanent changes in the capability for producing skilled action.”19, Pg 22It is the necessary process that allows individuals to learn new skills and improve thesmoothness and accuracy of movements.19 Physical therapists routinely utilize the theory ofmotor learning for rehabilitative treatment. Through the utilization of practice and intensity,the hallmarks of successful motor learning, physical therapists enable patients to producemotor patterns that are beyond their current capabilities.20 The use of practice and intensityduring training periods has been demonstrated to improve motor learning in individualslearning or relearning a task. Training that emphasizes these principles has beendemonstrated to improve the quality of motor learning and reproducibility of the skill infuture practice sessions and improve outcomes in both children and adults.21At this time there is no research available to determine the appropriateness of theFMS corrective exercises in the rehabilitative setting. Therefore, the purpose of this casereport was to determine if the FMS corrective exercises are useful in increasing trunkstrength and stability, flexibility, ADL’s and functional activities in a person post L5-S1lumbar discectomy.Case DescriptionThe individual in this case study was a 55 year old female department oftransportation laborer. Her job entails driving machinery such as a snow plow, heavy lifting,sitting and twisting at the trunk. She initially injured her low back while shoveling dirt froma washout at work on May 1, 2004. After this injury her symptoms resolved, in that she wasable to return to work and athletic/recreational activities. The medical management to treather back pain at this time is unknown. She had a second injury on March 26, 2009 when6
seated bending over to tie her boot at work. Shortly after her injury she was seen by herchiropractor who recommended she see a local orthopedic surgeon. She had an MRI whichwas positive for a herniated nucleus pulposis at the L5-S1 intervertebral disc. She was thenadmitted to the hospital for pain reduction several days prior to surgery, where she wastreated with morphine. The L5-S1 lumbar discectomy was performed on April 20, 2009. Sherated her pain as a 10/10 on the verbal analogue scale up until after the surgery wasperformed. The participant reported constant pain located down the posterior aspect of herright lower extremity extending to her foot. After the L5-S1 discectomy she was treated inthe hospital by a physical therapist until she was discharged at which time she returned homewith a home exercise program.She presented to outpatient physical therapy for an evaluation and strengtheningprogram after referral from her orthopedic surgeon. At the initial interview she rated her lowback pain as a 0-1/10 according to the verbal analogue scale. Her low back was “sore” innature, with constant numbness in her posterior thigh, leg, lateral foot and heel. At the initialevaluation she reported no bowel or bladder dysfunction. She was independent in activities ofdaily living (ADL) including self care and driving, however she was unable to perform othertasks such as cleaning her home, walking, hiking, hunting, camping and competitive archery.She had limitations in sitting, bending, trunk rotation, and lifting as depicted in table 1. Hergoals for physical therapy treatment were to return to work, and activities of daily livingunrestricted and without symptoms.Upon physical examination, she had limited trunk range of motion (ROM) in alldirections most notably rotation to the right. See Table 2 for specific measurements. Manualmuscle testing was performed according to the method determined by Hislop.22 She exhibited7
muscle strength deficits bilaterally with increased deficits noted in her right lower extremity.See Table 3 for specific measurements.She presented with impaired light touch sensation at her L4-S1 dermatomes and herAchilles deep tendon reflex was impaired. See Table 4 for specific measurements. Specialtesting demonstrated a positive straight leg raise and short sitting slump test on the right. Theaforementioned special tests were used to asses
Use of the Functional Movement Screen TM Corrective Exercises to Address Strength Deficits in a 55 Year Old Female Status Post L5-S1 Discectomy For the following purposes: - Place in the Sage Colleges Library collection and reproduce for Interlibrary Loan. - Keep in the Program office or library for use by students, faculty, or staff. - Reproduce for distribution to other students, faculty, or .