Transcription
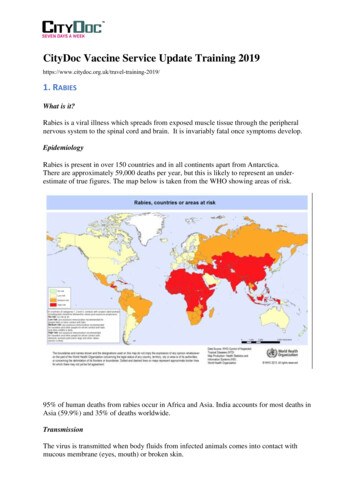
CityDoc Vaccine Service Update Training 9/1. RABIESWhat is it?Rabies is a viral illness which spreads from exposed muscle tissue through the peripheralnervous system to the spinal cord and brain. It is invariably fatal once symptoms develop.EpidemiologyRabies is present in over 150 countries and in all continents apart from Antarctica.There are approximately 59,000 deaths per year, but this is likely to represent an underestimate of true figures. The map below is taken from the WHO showing areas of risk.95% of human deaths from rabies occur in Africa and Asia. India accounts for most deaths inAsia (59.9%) and 35% of deaths worldwide.TransmissionThe virus is transmitted when body fluids from infected animals comes into contact withmucous membrane (eyes, mouth) or broken skin.
Rabies is mainly spread through saliva but can be found in other body fluids. Rabies is notpresent in blood.Rabies infections occurs in all warm-blooded animals, both domestic and wild, includingdogs, cats, monkeys, bats, raccoons, coyotes. Human to human transmission, althoughpossible, has not been documented.99% of rabies cases are due to dog bites (see map below from WHO 2016 data).However, in the Americas the majority of cases are due to bat rabies and this is an emergingthreat in Australia and Western Europe. In UK, bats carry a rabies like virus which causes aclinical illness indistinguishable from rabies. 12% of people requiring [post exposuretreatment in the UK were exposed to bat rabies.SymptomsThe incubation period from exposure to development of clinical disease varies from 3 to 12weeks. 90% of cases have onset within 1 year.The incubation period depends on the body part affected, with bites to the head, neck andhands having shorter incubation.Bites in children tend to occur to these areas due to short stature and as a consequence, up tohalf of cases and deaths occurring in children under 15 years.Early symptoms include: Fever Headache Muscle aches Fatigue Pins and needles around the woundThe disease may then follow 2 paths:
1. Furious Rabies-most common form and associated symptoms include: Fluctuating consciousness Spasms in response to drink water (hydrophobic spasms) Feeling of terror Hallucinations and mania ComaDeath usually occurs over days.2. Paralytic RabiesMuscle paralysis starting from infected body part, involving respiratory muscles, causingrespiratory failure and death, which usually occurs in 1-3 weeks.TreatmentThere is no effective treatment for rabies once symptoms develop. Therefore, post exposuretreatment is vital and effective at preventing symptom development and inevitable death.Only 15 people have been known to survive rabies and in all but 1 of the cases, they hadreceived one or more dose of the rabies vaccine pre exposure.PreventionAnimal Bite AvoidanceIt is important that all travellers to high risk areas for rabies avoid interaction with both wildand domestic animals. This includes feeding the animals. Rabid animals may not show signsof disease. Therefore, any animal contact in a rabies endemic area poses a risk of infection.Activities such as running and cycling often attract dogs leading to increased risk of bites.Pre-Exposure VaccinationBenefits Avoids need for rabies immunoglobin-difficult to obtain in many endemic countries.Reduces number of vaccines required post-exposure from 4 to 1.All available rabies vaccinations are inactivated and cannot cause the illness. Thevaccines can be used interchangeably.The rabies vaccines are licensed to be given from birth. The highest risk of exposure is inchildren who are independently mobile.EffectivenessFull primary course of rabies vaccine pre-exposure administered by the Intramuscular routeproduces rabies virus neutralising antibodies in more than 95% of immunocompetentrecipients. Additionally, in 95% of fully vaccinated individuals, the antibodies are long lived,providing long lasting protection (if the vaccine is administered through the intramuscular
route). Therefore, immunocompetent individuals primed with the full primary course willrespond promptly once they receive a booster dose of the vaccine in the event of an exposure.The only licensed route in the UK is intramuscular due to greater effectiveness.Individuals who has received part of the primary course with intradermal vaccine, cannotcomplete the course with intramuscular vaccination.Pre-exposure SchedulesThere are two recognised, approved and licensed schedules for the rabies vaccination. If thereis enough time before travel, then the standard schedule is preferred. All available rabiesvaccine can be used for both schedules.1. Standard schedule3 doses of rabies vaccine at day 0, day 7 and day 21 or day 282. Accelerated scheduleThis schedule is ONLY recommended for TRAVELLERS who have insufficient time tocomplete the standard schedule. 4 dose schedule at day 0, day 3, day 7 and 12 months.The 4th dose in this schedule is NOT a booster dose but part of the primary course to ensurethat the traveller is primed for a longer period of time. With the accelerated course antibodyresponses may wane more rapidly than someone given the standard 21 or 28 day preexposure schedule.If the individual only receives the first three out of the four doses in the accelerated schedule,they would be considered ‘fully immune’ for the purposes of post-exposure treatment.However, without the final (day 365) dose the individual may not be completely primed, andthe post-exposure treatment would need to be given promptly. If the patient misses the fourthdose (day 365) in the accelerated schedule, this should be given at the next opportunity. Abooster can then be given any time from one year after the day 365 dose.The accelerated schedule cannot be used if the traveller is having the vaccine through theintradermal route.Incomplete or Interrupted CoursesIdeally all three doses of the vaccine should be received pre-travel to obtain the most benefitfrom vaccination. Individuals who have had 1 or 2 doses of the primary course prior to travelwill receive full post exposure vaccination if 4 doses /- rabies immunoglobulin.With the new accelerated schedule, travellers should be able to achieve this.Where a course was started and not completed, there is no need to restart the course. Thepresence of immune memory means that vaccine doses given at later intervals do not affectthe immunological response. However, it is important to ensure that vaccine doses are not
given sooner than the recommended interval as this will not allow sufficient time for antibodyformation and lead to less immunologically effective vaccinations. Vaccine doses given atintervals linger than that recommended are not an issue from an immune response point ofview.Booster VaccinationsBooster dosing depends on the risk of rabies. See table below taken from Public HealthEngland Guidance (published April 2019). This should be used when advising on boosterrequirements.Booster Vaccination in travellersBooster doses in immunocompetent travellers following completion of the primary course (3doses of standard schedule or 4 doses of accelerated) will depend on future travel risk.
Therefore, all travellers should be advised to have a full travel risk assessment for any futuretrips. This includes the following: Risk of rabies in the subsequent travel destination Activities planned in destination Access to medical care and post exposure rabies treatmentThe purpose of the booster is to ensure the individual is fully primed for a longer period oftime to allow sufficient time to access post exposure treatment in remote areas.Booster doses can be offered as below: Anytime 1 year after completion of the standard scheduleAnytime 1 year after receipt of 4th dose of accelerated schedule.Booster dose may be more effective if given 5 years after completion of the primarycourses.ONLY A SINGLE BOOSTER is required in the traveller’s lifetime.Immunosuppressed IndividualsAs immunosuppressed individuals may not make a full antibody response, they face anincreased risk of clinical rabies if exposed. Therefore, despite receiving the complete primarycourse pre-exposure, they will still require full and longer course of post exposure treatment(5 doses of vaccine plus rabies immunoglobin).Post Exposure TreatmentAll travellers should be counselled on actions to take in the event of a rabies prone exposure.1. Wound careThe bitten/scratched area should be flushed in water for several minutes and thoroughlywashed with soap or detergent to remove the saliva from the wound. Alcohol 70% or iodinecan be used as the disinfectant if available. The wound should be covered with a simpledressing. The traveller should be advised to attend local medical centre for risk assessmentand consideration of need for treatment.2. Post Exposure TreatmentFor immune competent travellers, this consists of 4 doses of the rabies vaccine plusimmunoglobulin if considered high risk.This is not provided through CityDoc.All patients who have received a potential rabies probe exposure abroad or have started rabiespost exposure treatment abroad should be advised to attend their GP or A E. While postexposure treatment is not a medical emergency, treatment should be given urgently to ensurefull effectiveness.
Contacts For Post Exposure Treatment/AdviceEnglandThe Rabies Immunoglobulin Service (RIgS) is part of Public Health England team based atCollindale dealing with all post exposure rabies risk assessments. Their contact details are asbelow:RIgS contact details (for healthcare professionals only):Hours: Monday-Friday 09:00-17:00Telephone: 020 8327 6204Email: rigs@phe.gov.uk (for NON-urgent enquiries only)ScotlandAberdeen Royal Infirmary - 0345 456 6000Crosshouse Hospital, Ayrshire - 01563 521 133Queen Elizabeth Hospital, Glasgow - 0141 201 1100Monklands Hospital, Lanarkshire - 01236 748 748Ninewells Hospital, Dundee - 01382 680 111Victoria Hospital, Fife - 01582 643 355Western General Hospital, Edinburgh - 0131 537 10002. TRAVELLING WITH CHILDRENThe main concerns with paediatric travellers are: More likely to need hospitalisationLess likely to receive pre-travel adviceProne to more severe illnessesLimitations in provision of vaccinations due to age restrictions.The main reasons for hospitalisation in children are: Diarrhoeal illnessesSkin conditions such as insect bites/animal bites and sun burnFebrile illnessesRespiratory diseasesHowever, accident and injuries are the greatest cause of serious death in childrenPreparationIt is important that children are seen as soon as possible for pre-travel advice.As well as discussion on vaccine preventable diseases and malaria, counselling shouldinvolve prevention of diarrhoeal illness and its management, accident and injuries protection,animal and insect bite avoidance, as well as the importance of sun protection.
Parents should be advised on the following action while travelling:1. Importance of comprehensive travel insurance, including repatriation costs2. Taking plenty of sun protection-ideally factor 503. Oral rehydration salts and Alcohol hand gels4. Mosquito nets and insect repellent-DEET 50%.5. Analgesics from UK6. First Aid kit containing, tweezers (tick removal), dressings, anti-septic and thermometerDiarrhoeal IllnessThis is one of the most common illnesses encountered by children travelling abroad. They areparticularly vulnerable to prolonged illness and dehydration.Children are more likely to acquire traveller’s diarrhoea, because they have reduced killing ofingested bacteria owing to their higher gastric pH and more rapid gastric emptying time.Moreover, they are more immunologically naïve, and young children may be indiscriminateabout what they put in their mouthsPreventionFor infants, breastfeeding is the best way to prevent diarrhoea.Formula fed infants-the formula should be taken from the UK and made up with boiled water(not bottled water).Food and water hygiene should be maintained throughout as below: Wash hands in soap and water or alcohol gel if not feasible to do so immediately. Use only bottled or boiled/disinfected water for cleaning teeth. Ensure all food is cooked and served hot. Ensure any fruit is peeled by the caregiver. Consider taking snacks from the UK. Only give milk that has been pasteurised or boiled.TreatmentThe mainstay of treatment is ensuring rehydration through oral rehydration solutions anddrinking fluids little and oftenAntidiarrhoeal treatments like loperamide are not recommended in children under 6 years andshould generally be avoided.Prophylactic antibiotics are also not recommended for children.
Parents should be told to seek medical attention if there are signs of dehydration, or if thechild has severe diarrhoea or there is blood/mucous stained diarrhoea, high fever or severeabdominal pain.Sun ProtectionBabies and children are particularly vulnerable to sunburn and over exposure to the sun canincrease their risk of skin cancer later in life. Sunburn may also cause considerable pain anddiscomfort in the short term.The safest way to protect children from sunburn is to use a combination of shade, clothingand sunscreen. Use a sunscreen of at least SPF 15 which also has high UVA protection. Ensure sunscreens are applied generously to ALL sun exposed areas. Sunscreenshould be applied 20 - 30 minutes before sun exposure. Remember that showering, swimming and sweating may remove sunscreen; ensurefrequent application and consider water resistant sunscreens. Cover children up using clothing such as wide brimmed hat and long sleeved tops,closed weaved fabrics may offer better sun protection. Protect eyes from sun exposure, use sunglasses with a CE mark, UV400 label or thatoffer 100% UV protection. Seek shelter; avoid sun exposure between 11am and 3pm when sun is typicallystronger.MalariaMalaria is among the most serious and life-threatening infection that can be acquired
CityDoc Vaccine Service Update Training 2019 1. RABIES What is it? Rabies is a viral illness which spreads from exposed muscle tissue through the peripheral nervous system to the spinal cord and brain. It is invariably fatal once symptoms develop. Epidemiology Rabies is present in over 150 countries and in all continents apart from Antarctica. There are approximately 59,000 deaths per year .