Transcription
Doing Business withHumanaInformation for healthcareproviders and administrators
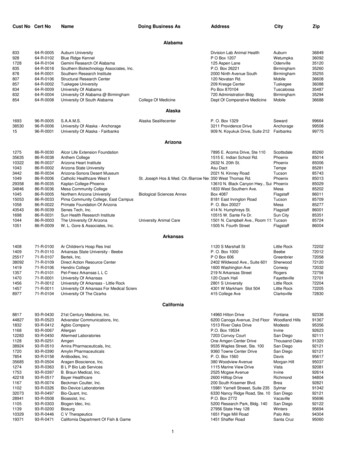
Presentation Overview1.Credentialing/Recredentialing2.Claims Inquiry Resolution Process and Code Edit Inquiries3.Provider Payment Integrity (Financial Recovery)4.Most Common Denial Reasons5.Preauthorization and Notification Guidelines6.Physician Finder Plus7.Online Tools – Making it Easy8.eBusiness/Availity9.Key Points of Contact2
Credentialing Overview3
Initial Credentialing The market contractors submit a task (via our workflow system) to add a provider or facility toHumana’s network. The contractor will indicate on that task, if credentialing is needed. As well asattach a completed credentialing application or the providers CAQH #. If Credentialing is needed, a credentialing task will be created and sent to the credentialing team. The credentialing team has a 7 day Service Level Agreement (SLA) for physicians and 2 day SLA forfacilities. The Credentialing team will review the credentialing application to ensure all requiredelements are present. If the required elements are present, the credentialing team will complete the provider/facility credentialing. A letter is sent to theprovider/facility advising their credentialing was approved. If the required elements are not present, the credentialing team will deny the provider/facility credentialing. An automaticnotification from our workflow system is sent to the market contractor that submitted the task, to advise them that credentialingwas denied and what information they need to obtain for credentialing to complete the provider/facilities credentialing.Some situations require a provider to be taken to our committee board for review and determination asto whether the providers credentialing can be approved. Reasons for taking a provider to committeeare, but not limited to: Licenses with current material limitations, Adverse reactions indicated on theproviders NPDB report, Restricted DEA/CDS, etc.4
Recredentialing Providers and Facilities are required to be recredentialed every 3 years (unless their state mandatesrecredentialing more frequently). Humana will initiate the provider/facilities recredentialing 7 months prior to their recred due date. Thisallows plenty of time for the credentialing team to make multiple outreach attempts (phone calls, faxesand mailings) to collect the needed information to complete recredentialing. Note: Providers using CAQH – As long as they’ve re-attested within the last 120 days, and there isn’t any expiredinformation, we can complete their recredentialing without any outreach attempts to the provider needed. Providers not using CAQH and facilities, are required to complete a new credentialing application for theirrecredentialing to be processed. Providers and facilities still missing information 60 days prior to their recred due date are sent to themarket contractors. The contractors then attempt to collect the needed information. Providers and facilities still missing information 30 days prior to their recred due date are sent a certifiedletter, advising them that if the completed credentialing application/missing information is not providedin the next 30 days, they will be decredentialed.5
Recredentialing, continued Providers and facilities still missing the required information to complete their recredentialing, attheir recred due date, are then decredentialed and removed from Humana’s network. Providers and facilities successfully recredentialed receive a letter from Humana, notifying themthat they’ve successfully been recredentialed. Providers and facilities that are decredentialed aresent a letter from Humana and the market contractors are notified of all decredentialed andtherefore termed providers and facilities as well. The same reasons a provider may need to go to the committee board during the initialcredentialing process, may result in a provider being taken to the committee board atrecredentialing as well. For example: A provider could have limitations placed on their licensesafter they were initially credentialed. This would require the committee board to review theprovider information and make the determination as to the providers recredentialing beingapproved or denied.6
Claims7
Claim Submission Time Frames Claim submission time frames–Medicare Advantage: One (1) calendar year from date of service–Commercial: Generally must be submitted within: 180 days from the date of service for physicians 90 days from the date of service for facilities and ancillary providersPlease reference your contract as these timeframes may differ8
Claim Payment Inquiry Resolution GuideStep 11. Call Humana’s Provider Contact Center (PCC) at 1-800-448-6262. OurProvider Contact Center Agents are trained to answer many of your claimsquestions and can initiate contact with other Humana departments whenfurther review or research is needed. a. Note the reference number issued to you by the Provider Contact CenterAgent, as it may be needed in the future. b. You have the option to speak to a Provider Contact Center supervisor if youfeel your concern is not being properly addressed. Based on availability, youwill either be connected to a supervisor, or a supervisor will contact youwithin 48 hours of your request. c. If the Provider Contact Center associate needs to have your disputereviewed by another department, you will receive a letter from the Humanadepartment that completes the additional review/research. You will benotified of the review via a corrected EOR or a letter explain why the claimwas upheld within 30 to 45 days. Please allow us time to properly researchand resolve your inquiry before contacting us again.9
Claim Payment Inquiry Resolution GuideStep 22. Once you have received our response to your initial Provider Contact Centerinquiry and you disagree with the determination, you may escalate yourconcern by submitting a secure email tohumanaproviderservices@humana.com. Be sure to include : a. The reference number(s) associated with previous attempt(s) to resolvethe inquiry (referenced in 1a above) b. Health care provider name and tax ID number c. Member name and identification number, including the relationship of themember to the patient d. Date of service, claim number and name of the provider of the services e. Charge amount, actual payment amount, expected payment amount and adescription of the basis for the contestation f. Contact information for our response10
Claim Payment Inquiry Resolution GuideStep 33. Look for an “Acknowledgment of Submission” email with atracking number within five business days of your submission.Please allow 30 to 45 days from the date of the acknowledgmentnotice for our response. The specialist assigned your inquiry will provide an update every14 days regarding the status of your submission until thesubmission is complete.11
Claim Code Edits Code editing is the process of evaluating information submittedon a claim. The information considered includes, but is notlimited to:–Procedure codes, diagnosis codes, revenue codes, billing units, andmodifiers–Attributes of the member, such as age or gender12
Claim Code Edits, continued Humana applies code editing to: Validate the accuracy and integrity of codes submitted forpayment consideration Ensure consistent and appropriate processing of member claims,based on the services billed Facilitate accurate reimbursement for providers Administer Humana’s policies and industry standard codingguidelines Maintain compliance with coding, clinical and regulatoryguidelines13
Appeals and Reconsideration Participating providers can requesta “reconsideration” which ishandled through ourCorrespondence Department Provider Reconsiderations shouldbe sent to:HumanaProvider ReconsiderationsPO Box 14601Lexington, KY 40512-4601 Appeals on behalf of the membermust be submitted to Humanawithin 60 days from the date of thedenial. Appeals should be sent to:HumanaProvider AppealsP.O. Box 14165Lexington, KY 40512-416514
Provider Payment Integrity(Financial Recovery)15
Provider Payment Integrity – Types of Audits Global Audits - Focuses on overpayment issues that are notprovider specific (COB, Duplicates, Retro Contract Terms) Contractual Audits – Focus is to ensure claims are paid inaccordance with provider contract – queries target provisionswithin provider contracts (i.e., Stop Loss, Carve-Outs, etc.) Clinical Audits - Use internal team & vendors with clinicalexpertise (physicians, nurses, coders, pharmacists, etc) to reviewmedical records and identify potential overpayments due toincorrect coding and billing, services did not meet medicalnecessity criteria, etc.16
Clinical Types of Audits Examples of audits performed (this list is not all inclusive):Intensity of Service Audit: Inpatient stays are reviewed to determine if the service/procedure could havebeen performed in a less-intensive setting. CMS criteria and Milliman criteria are used for the review.Diagnosis Related Group (DRG) Coding: DRG audits are performed to determine that the correct procedurecodes and diagnosis codes have been billed based on the physician’s documentation in the medical record.Hospital Bill Audits: Registered nurses review medical records to validate that items billed on the itemized billwere provided to the patient and a physician order is present.Humana Registered Nurse (RN) & Medical Doctor (M.D.) Audits: Cases are reviewed to determine if productsand technologies are used that are not Food and Drug Administration (FDA) approved, are used in a mannerdifferent than there intent, or are not used in accordance with Humana’s medical coverage policies.APC Coding (Post-payment Coding): Outpatient cases that are paid according to Ambulatory PaymentClassifications (APC) are reviewed to ensure HCPCS codes and CPT codes billed are correct and supported bymedical records.High Cost Drug Audits: The medical record is reviewed to determine if a drug was ordered by the health careprovider, administered to the member, and units billed are supported in the documentation.Pre-Pay reviews: The itemized bill and/or medical records are requested to perform any of the audits listedabove but this list may not be all inclusive.17
18
Provider Payment Integrity (PPI) Resolution ProcessFor provider payment integrity inquiries (not related to a medical record review dispute), pleaseleave a secure voice mail message for the Humana PPI Customer Care Team by calling 1-800-4387885 or sending a message to the secure e-mail address: ContactPPI@humana.com. Pleaseinclude the following information: Patient name Member identification number Date of service Claim number Recovery identification number Reason for your call Contact name, e-mail, mailing address, phone number, and best time to call Your preferred method of response A Humana PPI Customer Care representative will carefully research your question and provideyou with a response within three business days. Be sure to note the reference number providedby the representative and refer to it if you need to contact us again regarding the same topic. 19
PPI Resolution Escalation Process If you feel the response to your inquiry was unsatisfactory or did not resolve yourconcern, you may escalate your PPI concern by sending a secure email toHelpPPI@humana.com.Please note:–The subject line of your email should have the reference number(s) associated with theprevious attempt(s) to resolve the inquiry.–The email body should include the required information listed above, plus the: Health care provider name Tax Identification number Charge amount, actual payment amount, and expected payment amount Description of the basis for the disputeYou will receive an “Acknowledgement of Submission” email within three business days.Please allow seven business days for review and response to your inquiry.20
Preauthorization andNotification Guidelines21
Preauthorization, Case Management, and PharmacyDepartmentPhone NumberAdditional InformationClinical Intake TeamReferrals, authorizations, andnotifications1-800-523-0023Online referrals andauthorizationsAvaility Web Portal:www.availity.comCase ManagementCommercial: 1-800-327-9496Medicare and Medicaid: 1800-322-2758Humana Clinical PharmacyReviewAuthorizations, step therapy,quantity limits and medicationexceptionsPhone: 1-800-555-2546Fax: 1-877-486-262122
Utilization Management Vendors US ImagingNetwork/HealthHelp/RadSite– Orthonet––– High dollar imaging authorizationsOutpatient therapies (PT, OT, ST)Pain ManagementSpinal SurgeryNew Century Health––ChemotherapyIt is the physicians’ responsibilityto obtain the authorization23
Physician Finder Plus24
Using Physician Finder Plus Get to Physician Finder from www.humana.com 2 search functions available: “Just Looking” or Member ID Searching by Member ID yields better results You can search by the physician’s name or specialty Results are displayed within a 15 mile radius; however you canchange your radius option25
Online Tools onhumana.com(Unsecure)26
On-line Tools (Unsecure) Claims processing edits Claim coding guidelines Provider Payment Integrity policies (financial recovery) Medical and pharmacy coverage policies Preauthorization and Notification List Provider manual Medicare provider materials27
Making It Easier On-demand training modules–Working with Humana–Making It Easier for Healthcare Providers Anatomical Modifiers Modifier 24,25, 59, and X (EPSU) Medicare Preventive Services Procedure-to-Procedure Code Editing Printable Tip Sheets Available Plus many, many, more28
Key points of contact29
Please visit our table for tip sheets andmore information on the following: Provider Quick Reference Guide Making It Easier Flyer Claim and Provider Payment Integrity Resolution Guide Information on Humana’s vendors30
Questions31
The credentialing team has a 7 day Service Level Agreement (SLA) for physicians and 2 day SLA for facilities. The Credentialing team will review the credentialing application to ensure all required elements are present. If the required elements are present, the credentialing team will compl