Transcription
Medical LeadershipCompetency FrameworkEnhancing Engagement in Medical LeadershipThird Edition, July 2010
NHS Institute for Innovation and Improvement and Academy of Medical Royal Colleges 2010.All rights reserved.This publication may be reproduced and circulated free of charge for non-commercial purposesonly by and between UK medical professional, regulatory and educational organisations, NHSEngland, Scotland, Wales and Northern Ireland staff, related networks and officially contractedthird parties. This includes the right to reproduce, distribute and transmit this publication in anyform and by any means, including e-mail, photocopying, microfilming, and recording. No otheruse may be made of this publication or any part of it except with the prior written permission ofthe NHS Institute for Innovation and Improvement, application for which should be in writing andaddressed to the Marketing Department (and marked ‘re. permissions’). Written permission mustalways be obtained before any part of this publication is stored in a retrieval system of anynature, or electronically. Reproduction and transmission of this publication must be accurate,must not be used in any misleading context and must always be accompanied by this CopyrightNotice.Warning: Unauthorised copying, storage, reproduction, adaptation or other use of thispublication or any part of it is strictly prohibited. Doing an unauthorised act in relation to acopyright work may give rise to civil liabilities and criminal prosecution.Publisher: NHS Institute for Innovation and Improvement, Coventry House, University of WarwickCampus, Coventry, CV4 7AL.ISBN 978-1-907045-88-2
ContentsPagePreface5Medical Leadership Competency Framework6Who is it for?8Development10Design11Application121. Demonstrating Personal Qualities131.1 Developing Self Awareness141.2 Managing Yourself171.3 Continuing Personal Development201.4 Acting with Integrity222. Working with Others272.1 Developing Networks282.2 Building & Maintaining Relationships302.3 Encouraging Contribution342.4 Working within Teams373. Managing Services413.1 Planning423.2 Managing Resources453.3 Managing People483.4 Managing Performance514. Improving Services554.1 Ensuring Patient Safety564.2 Critically Evaluating594.3 Encouraging Improvement and Innovation624.4 Facilitating Transformation655. Setting Direction695.1 Identifying the Contexts for Change705.2 Applying Knowledge and Evidence735.3 Making Decisions765.4 Evaluating Impact79AcknowledgementsEnhancing Engagement in Medical Leadership823
PrefaceThe Medical Leadership Competency Framework (MLCF) was jointly developed by the Academy of Medical RoyalColleges and the NHS Institute for Innovation and Improvement in conjunction with a wide range of stakeholders.The MLCF describes the leadership competences that doctors need to become more actively involved in the planning,delivery and transformation of health services.In developing the MLCF the project team carried out a review of literature and key publications, a comparativeanalysis of other leadership competency frameworks, and an analysis of medical curricula. They also consulted withmembers of the medical and wider NHS community and received input from the project steering group, referenceand focus groups. The MLCF has been successfully tested in a range of medical education and service communitiesacross the UK. Since it was originally published in May 2008, we have received further feedback from manyindividuals and groups including patient and lay groups, equality and diversity experts, medical students and doctors,and from organisations implementing the framework. We incorporated many of the suggested improvements intothe second edition of the MLCF in 2009 and further feedback has been incorporated into this third edition.The project team continues to work closely with those involved in the delivery of medical education and NHS servicesto assist in translating the MLCF into curricula and learning experiences. Following its incorporation into Tomorrow’sDoctors, we have developed the Guidance for Undergraduate Medical Education: Integrating the Medical LeadershipCompetency Framework for medical schools as well as the Medical Leadership Curriculum which has beenincorporated into the 58 specialty curricula of the Medical Royal Colleges and Faculties.We very much hope that the MLCF will contribute to the vision articulated in the following key documents:“The doctor’s frequent role as head of the healthcare team and commander of considerable clinical resource requiresthat greater attention is paid to management and leadership skills regardless of specialism. An acknowledgement ofthe leadership role of medicine is increasingly evident. Role acknowledgement and aspiration to enhanced roles bethey in subspecialty practice, management and leadership, education or research are likely to facilitate greater clinicalengagement.” (Aspiring to Excellence, Prof John Tooke, 2008)“Greater freedom, enhanced accountability and empowering staff are necessary but not sufficient in the pursuit ofhigh quality care. Making change actually happen takes leadership. It is central to our expectations of the healthcareprofessionals of tomorrow.” (Next Stage Review: High Quality Care for All, July 2008)“It is not enough for a clinician to act as a practitioner in their own discipline. They must act as partners to theircolleagues, accepting shared accountability for the service provided to their patients. They are also expected to offerleadership and to work with others to change systems when it is necessary for the benefit of patients.” (Tomorrow’sDoctors, September 2009)The MLCF is part of the wider Enhancing Engagement in Medical Leadership project. You will find more details atwww.institute.nhs.uk/medicalleadership. If you have any comments on the MLCF or would like more details about theproject, please email us at: medicalleadership@institute.nhs.ukProfessor Dame Carol BlackChair, Steering GroupAcademy of Medical Royal CollegesProfessor Peter SpurgeonProject DirectorNHS Institute for Innovation and ImprovementProfessor Sir Neil DouglasChairmanAcademy of Medical Royal CollegesProfessor John ClarkDirector, Medical Leadership and International RelationsNHS Institute for Innovation and ImprovementEnhancing Engagement in Medical Leadership5
Medical LeadershipCompetency FrameworkLeadership and DoctorsLeadership is a key part of doctors’ professional work regardless of specialty and setting. It is already arequirement of all doctors as laid out in the General Medical Council’s (GMC) publications Good MedicalPractice, Tomorrow’s Doctors and also Management for Doctors.While the primary focus for doctors is on their professional practice, all doctors work in systems and withinorganisations. It is a vitally important fact that doctors have a direct and far-reaching impact on patientexperience and outcomes. Doctors have a legal duty broader than any other health professional and thereforehave an intrinsic leadership role within healthcare services. They have a responsibility to contribute to theeffective running of the organisation in which they work and to its future direction. The development ofleadership competence needs to be an integral part of a doctor’s training and learning. The MLCF is intendedas an aid and driver for this and to enable a doctor in the NHS to be: A Practitioner A Partner A Leader.The Medical Leadership Competency Framework (MLCF) is built on the concept of shared leadershipwhere leadership is not restricted to people who hold designated leadership roles, and where there is ashared sense of responsibility for the success of the organisation and its services. Acts of leadership cancome from anyone in the organisation, as appropriate at different times, and are focused on theachievement of the group rather than of an individual. Therefore shared leadership actively supportseffective teamwork.The MLCF describes the leadership competences that doctors need to become more activelyinvolved in the planning, delivery and transformation of health services.6Enhancing Engagement in Medical Leadership
The MLCF is a key tool which can be used to: Help with the design of training curricula anddevelopment programmes Highlight individual strengths and developmentareas through self-assessment and structuredfeedback from colleagues Help with personal development planning andcareer progression.This document is designed to be read and usedin conjunction with other medical and servicepublications. These include: General Medical Council (GMC) (www.gmcuk.org): Tomorrow’s Doctors (2009),Good Medical Practice (2006), Member’s Codeof Conduct Department of Health (DH) (www.dh.gov.uk):Knowledge and Skills Framework (2004), HighQuality Care for All: Next Stage Review FinalReport (2008) Specialty curricula of the Medical Royal Collegesand Faculties are available to view roved curricula systems.aspEnhancing Engagement in Medical Leadership Foundation on Programme Curriculum (2010) NHS Institute for Innovation and Improvement(NHS Institute) and Academy of Medical RoyalColleges (AoMRC)(www.institute.nhs.uk/medicalleadership andwww.aomrc.org.uk): Engaging Doctors inLeadership: What can we learn from internationalexperience and research evidence? (2008),Engaging Doctors: Can doctors influenceorganisational performance? (2008), Guidance forUndergraduate Medical Education: Integratingthe Medical Leadership Competency Framework(2010), Medical Leadership Curriculum (2009) Programmes and publications on quality, value,safety, innovation and leadership. Furtherinformation can be found onwww.institute.nhs.uk.Those interested in learning more about theknowledge and skills underpinning the MLCF maywish to use the LeAD learning sessions, availablefrom e-Learning for Healthcare (http://www.elfh.org.uk/lead).7
Who is it for?The Medical Leadership Competency Framework applies to all medical students, qualified doctors and dental surgeons.The way a doctor demonstrates competence and ability will vary according to the career path chosen and their level ofexperience and training. However, all competences should be capable of being achieved at all career stages, though indifferent contexts.Three main career stages have been identified and used throughout the MLCF:Stage 1: up to the end of undergraduate trainingStage 2: up to the end of postgraduate trainingStage 3: up to five years or equivalent continuing practice.UndergraduateAt undergraduate stage (medical school) all medicalstudents will be expected to achieve learning outcomes asdefined by the medical school curriculum (based on theGMC Tomorrow’s Doctors). Those outcomes concerned withThe Doctor as a Professional in particular are relevant to thecompetences within the MLCF.During their medical school training students will haveaccess to relevant learning opportunities within a variety ofsituations including: peer interaction group learning clinical placements activities and responsibilities within the university involvement with charities, social groups andorganisations.All these situations can provide a medical student with theopportunity to develop experience of leadership, to developtheir personal styles and abilities, and to understand howeffective leadership will have an impact on the system andbenefit patients as they move from learner to practitioneron graduating.8PostgraduateAt postgraduate stage the MLCF applies to all doctors intraining and practice. That is, during foundation years andto those: in specialty training (specialty curriculum approved bythe General Medical Council (GMC) [as of 1st April2010, and formerly by the Postgraduate MedicalEducation and Training Board (PMETB)], and in non-specialist training posts (postgraduate deaneryand service responsibility).As they train further and consolidate their skills andknowledge in everyday practice, doctors in training are veryoften the key medical person relating to patients and otherstaff, and the ones who are experiencing how day-to-dayhealthcare works in action.They are uniquely placed: to develop experience in management and leadershipthrough relationships with other people, departmentsand ways of working, and to understand how the patient experiences healthcare,and how the processes and systems of delivering carecan be improved.Specific activities such as clinical audit and research alsooffer the opportunity to learn management and leadershipskills. With all this comes the need to understand how theirspecialty and focus of care contributes to the widerhealthcare system.Enhancing Engagement in Medical Leadership
Continuing PracticeKeyI Depth and extent of competence will belimited. Lesser degree of emphasis on thedomain due to fewer opportunities todemonstrate competence. However, shouldhave developed the underpinning knowledgeand skills as a foundation for futurecompetence in this areaI Depth and extent of competence will begreater. Greater degree of emphasis withmore opportunities to show competence inall elements of the domainContinuing practice describes the stage of post specialistcertification, or the time during the first years of practiceafter training. The MLCF applies to all consultants andgeneral practitioners. It also applies to doctors who donot have specialist or generalist registration but who workas staff or associate specialist grade or as trust doctors innon career grade posts in hospitals.The ending of the formal training period brings with itroles and responsibilities within the team deliveringpatient care, as well as in the wider healthcare system.Doctors need an understanding of the need for each areato play its part. Experienced doctors develop their abilitiesin leadership within their departments and practices andby working with colleagues in other settings and onprojects. Their familiarity with their specific focus of careenables them to work outside their immediate setting andto look further at ways to improve the experience ofhealthcare for patients and colleagues. As establishedmembers of staff or as partners, they are able to developfurther their leadership abilities by actively contributing tothe running of the organisation and to the way care isprovided generally.Enhancing Engagement in Medical LeadershipI Depth and extent of competence will begreatest. Greatest degree of emphasis withfrequent opportunities to show competencein all elements of the domainThe diagrams illustrate the expectations ofdepth and the extent to whichcompetences can be demonstrated atdifferent career stages. That is, the darkerthe shading, the greater the depth andextent of competence.All domains and elements of the MLCF applyto all medical students, doctors in training, andConsultants and GPs. However, the applicationof and opportunity to demonstrate thecompetences in the MLCF will differ accordingto the career stage of the doctor and the typeof role they fulfil. The context in whichcompetence can be achieved will becomemore complex and demanding with careerprogression.9
DevelopmentThe Medical Leadership Competency Framework hasbeen in development since August 2006. It was firstpublished in 2008 and the project team drew on:Employers, COPMeD, MSC, BMA, NHS Institute forInnovation and Improvement and Department ofHealth. A review of the literature on medicalleadership and engagement. Advice from reference groups consisting ofindividuals from all levels within medical andservice communities. Comparative analysis of leadershipcompetency frameworks and curricula bothnationally and internationally. Influentialframeworks include: NHS Institute for Innovation andImprovement: Leadership QualitiesFramework (LQF) British Association of Medical Managers: ASyllabus for Doctors in Management andLeadership Positions in Healthcare Institute for Health Improvement:Engaging Physicians in a Shared QualityAgenda Health Care Leaders Association of BritishColumbia: Health Leadership CapabilitiesFramework for Senior Executive Leaders Management Standards Centre: NationalOccupational Standards for Managementand Leadership. Analysis of specialty medical curriculasubmitted to and approved by the GeneralMedical Council (GMC) [as of 1st April 2010, andformerly by the Postgraduate Medical Educationand Training Board (PMETB)]. Consultation with members of the medicaland wider NHS community in the UK includingthe GMC, PMETB [prior to 1st April 2010], NHSConfederation, NHS Employers, Conference ofPostgraduate Medical Education Deans(COPMeD), Medical Schools Council (MSC) andthe British Medical Association (BMA). Consultation with Patient Lay AdvisoryGroups of the Medical Royal Colleges Semi-structured interviews with MedicalSchool Deans, Postgraduate Deans and Presidentsof Medical Royal Colleges. Feedback from focus groups of medicalstudents, junior doctors, consultants and generalpractitioners. Review of key documents produced by medicalprofessional and regulatory bodies such asTomorrow’s Doctors, Good Medical Practice,Aspiring to Excellence: Final Report of theIndependent Inquiry into Modernising MedicalCareers and High Quality Care for All: NHS NextStage Review Final Report.The Project Steering Group has also tested the MLCFin a variety of medical education and servicecommunities in the UK to ensure that thecompetences are relevant to doctors at the differentstages in their training and careers.Why competence and not capability? As theGMC refers to a doctor’s competence, we have usedthis term throughout to be consistent with currentterminology.Will the MLCF stand the test of time? The MLCFhas been written in language designed to stand thetest of time. However, revisions may need to bemade from time to time to make sure it is in linewith the latest thinking and health service needs.What has changed in this third edition? Minorrefinements in this third edition have been madeafter feedback from patient groups, PMETB (prior to1st April 2010), Medical Royal Colleges, doctors andmanagers from acute and foundation trusts andgeneral practice based on the use of the MLCF. TheMLCF has also been reviewed in the light ofchanging regulatory advice for undergraduate andpostgraduate training. Advice from the Project Steering Group whichhas been led by the Academy of Medical RoyalColleges (AoMRC) and includes representationfrom the GMC, NHS Confederation, NHS10Enhancing Engagement in Medical Leadership
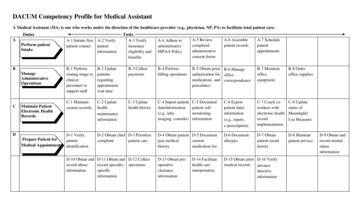
DesignDelivering services to patients, service users, carers and the public is at the heart of the Medical LeadershipCompetency Framework. Doctors work hard to improve services for people. The word ‘patient’ is used genericallyto cover patients, service users, and all those who receive healthcare. The word ‘others’ is used to describe allcolleagues from any discipline and organisation, as well as patients, service users, carers and the public.There are five domains highlighted below. To deliver appropriate, safe and effective services, it is essential that anydoctor is competent in each of the five domains. Within each domain there are four elements and each of theseelements is further divided into four competency outcomes (outlined in this document).1. Demonstrating Personal Qualities4. Improving Services 1.1 Developing self awareness 4.1 Ensuring patient safety 1.2 Managing yourself 4.2 Critically evaluating 1.3 Continuing personal development 4.3 Encouraging improvement and innovation 1.4 Acting with integrity 4.4 Facilitating transformation2. Working with Others5. Setting Direction 2.1 Developing networks 5.1 Identifying the contexts for change 2.2 Building and maintaining relationships 5.2 Applying knowledge and evidence 2.3 Encouraging contribution 5.3 Making decisions 2.4 Working within teams 5.4 Evaluating impact3. Managing Services 3.1 Planning 3.2 Managing resources 3.3 Managing people 3
the General Medical Council (GMC) [as of 1st April 2010, and formerly by the Postgraduate Medical Education and Training Board (PMETB)], and † in non-specialist training posts (postgraduate deanery and service responsibility). As they train further and consolidate their skills and kno