Transcription
Enrollment Guide for Electronic Services 2014 Kareo, Inc. Rev. 3/111
Table of Contents1. Introduction .11.1 An Overview of the Kareo Enrollment Process . 12. Services Offered. 22.1 Electronic Claim Services . 22.2 Electronic Remittance Advice (ERA) Services . 22.3 Electronic Eligibility Services . 23. How to Enroll in Electronic Services . 33.1 Understanding the Enrollment Process . 33.2 Enrolling Providers with Kareo and Clearinghouse . 33.3 Enrolling Providers with Payers. 33.4 Transitioning to Kareo from Another Billing System . 53.5 Common Enrollment Errors . 53.6 Tracking Your Enrollments . 63.7 Trouble Shooting Enrollments with Payers . 64. How to Use Services . 84.1 Setting up Provider and Group Numbers . 84.2 Activating Electronic Services within Kareo . 84.3 Sending Electronic Claims. 104.4 Submitting Eligibility Requests . 104.5 Reviewing Clearinghouse Reports . 104.6 Using Electronic Remittance Advice Reports .115. Contact Information . 125.1 Who should I contact to check on enrollment status? . 125.2 Kareo Contact Information. 125.3 Clearinghouse Contact Information . 126. Sample Web Enrollment Request Form . 137. Sample Payer Agreement . 158. Enrollment Worksheet . 169. Glossary of Terms. 17 2014 Kareo, Inc. Rev. 3/11i
1.IntroductionKareo’s electronic clearinghouse services provide connections to over 3,000 government payers and commercialinsurance companies with support for primary and secondary electronic claim processing, electronic remittance,and patient eligibility verification services. This guide provides complete instructions for enrolling in theseservices.1.1An Overview of the Kareo Enrollment ProcessYou will follow the steps below to enroll your providers in electronic services: You will start the process by submitting a web enrollment request to Kareo by completing an onlineform located at nt/. Kareo will register your new providers with the clearinghouse and notify you within 24-48 hours whencomplete. This step allows you to begin sending claims immediately to any payer that does not requirea separate enrollment agreement. To enroll for any payers that do require a separate enrollment agreement, you will be responsible fordownloading agreements directly from Kareo’s Help and Support website located house/payers. You will be responsible for gettingyour providers’ signatures, completing the agreements correctly, and identifying yourself as the contactto be notified by the payers regarding your enrollment status. You will send the signed enrollment agreements directly to the payers, and NOT to the clearinghouse. After 15-45 days, depending on the payer, you will be notified by the payer once your enrollmentagreements have been received and have been approved (or denied). You will be able to configure your enrollment settings within Kareo to begin sending electronic claimsimmediately to approved payers once you have been notified by the payer or you have verified theapproval by calling the payer.To ensure a timely implementation of Kareo, please read this guide carefully for complete information about theenrollment process. You may also refer to the Clearinghouse Enrollment training video located on Kareo’s Helpand Support at https://help.kareo.com/training/recorded webinars/enrollment 2014 Kareo, Inc. Rev. 3/111
2.2.1Services OfferedElectronic Claim ServicesKareo’s electronic claim services enable you to submit health care claims directly from the Kareo application,through our third-party clearinghouse partners, to over 3,000 government and commercial insurance payers.Kareo’s electronic claim services also include the delivery of electronic claim submission response reports frominsurance companies, government payers, and our clearinghouse partners.Kareo provides multiple levels of reporting as your claims make their way through the claim submission andadjudication process. Once you submit your claims, we automatically review all of your claims and returninternal validation reports to highlight claims with missing information, such as missing provider or groupnumbers, missing patient information, or missing policy numbers. Once your claims pass our internal validation,we send your claims to the appropriate clearinghouse partner who also reviews your claims and return dailyreports that highlight claims that have been rejected for various payer-specific reasons. Once your claims aredelivered to payers, the payer may respond with acceptance reports or reports highlighting claims that havebeen rejected for various reasons prior to the adjudication process.2.2Electronic Remittance Advice (ERA) ServicesKareo’s electronic remittance services include the delivery of electronic remittance advice (ERA) reports; and inmany cases, electronic funds transfer (EFT) reports from payers. Using electronic remittance services can saveyou significant time in posting payments and reconciling responses from payers as compared to manualpayment posting using the older, paper explanation of benefits (EOB) reports.Once you have enrolled and your enrollment has been approved by the payers that provide ERA services, youshould begin receiving ERA reports within 24-48 hours of claim adjudication. You also receive electronic fundstransfer (EFT) reports within 24 hours of funds transfer.All of your reports are automatically routed to the right medical practice within your account. You can view andprint all remittance reports in a standardized format. You can save them to your computers in ANSI 835 format;or you can export your ERA reports for use with other programs, such as Medicare's Remit Easy Print software.You can also use these reports to automatically post payments to patient accounts.2.3Electronic Eligibility ServicesKareo’s electronic patient eligibility services enable you to submit eligibility verification requests directly fromthe Kareo application to certain payers that provide these services. Using Kareo's real-time patient eligibilityengine empowers you to make sure patients have valid insurance coverage before scheduling the patient's visit,which helps reduce downstream claim denials and uncollectible accounts receivable. When you submit aneligibility verification request to a payer, you will be returned an eligibility report that can be viewed or printed.You can also store or attach the eligibility report to the patient’s insurance policy record for future reference.You can perform real-time patient eligibility checks for many of the larger government and commercialinsurance payers through Kareo’s clearinghouse interface to Capario and Gateway. Kareo will be introducingsupport for additional payers as this service becomes available through them.Note that this service is only available for practices that have subscribed to the Complete or Max Edition ofKareo. 2014 Kareo, Inc. Rev. 3/112
3.How to Enroll in Electronic Services3.1Understanding the Enrollment ProcessThere are two critical steps to enrolling your providers in electronic claims, electronic remittance, and patienteligibility services:3.2 Enrolling Providers with Kareo and the Clearinghouse – This step involves registering your providers’information with Kareo and the clearinghouse so that our systems are configured to send your claimsand eligibility requests correctly to the payers. Enrolling Providers with Payers – This step involves registering your providers’ information with thepayers so that their systems know to expect to receive electronic claim and eligibility requests from yourproviders through Kareo, and so they know to deliver your electronic remittance reports to Kareo.Enrolling Providers with Kareo and ClearinghouseThe first step of the process is to complete Kareo’s Web Enrollment Request form. This step registers yourproviders’ information with Kareo and the clearinghouse so that our systems are configured to send your claimsand eligibility requests correctly to the payers.You can access the Kareo Web Enrollment Request Form from the following web enrollment.Once you complete the Kareo Web Enrollment Request Form, Kareo will process your information by registeringyour providers with the clearinghouses and sending you an email within two business days of receiving yourrequest. Since most commercial payers (e.g. Aetna, Cigna, United Healthcare, etc.) do not require separate payeragreements, you will be able to begin submitting electronic claims to these payers as soon as Kareo notifies youthat your enrollment request has been processed. (Note that there will be certain payers that might requiresome additional setup time before you can begin sending claims to those payers. Kareo will notify you whenthat is the case.)To begin submitting claims to your commercial payers, you must activate the practice for electronic claims,configure certain settings in the insurance company record associated with those payers, and then beginsubmitting claims. For information on using Kareo’s electronic services, please see section 4, “How to UseServices.” For a sample of Kareo’s Web Enrollment Request Form, including a list of information to gather priorto completing this form, please see section 6.3.3Enrolling Providers with PayersThe second step of the enrollment process is to find and get payer-specific enrollment agreements, complete theagreements, have your physicians sign the agreements, and then send the agreements to the payer. Once thepayer receives and processes your enrollment request, the payer will notify you with an approval indicating youcan begin sending claims to that payer.Only certain payers require a separate agreement prior to submitting claims to them. While it varies by state,the payers that typically require payer agreements include Medicare, Medicaid, Tricare/CHAMPUS, BlueCross/Blue Shield, and a few others. 2014 Kareo, Inc. Rev. 3/113
To enroll with these payers, you will need to download the payer agreements directly from Kareo’s Help &Support website at use/payers. As you search the payerlist, note that that the “Services” column lists the various electronic services offered by each payer, and the“Agreements” column provides a link to the agreements that can be downloaded. Please refer to theinstructions just above the payer list prior to searching the list and downloading your agreements.When downloading payer agreements, you should decide beforehand which clearinghouse you will be using toprocess your claims. Kareo offers clearinghouse connections with Gateway and Capario.Note regarding Eligibility services. You typically do not need to complete a separate payer agreement foreligibility verification. Once you are enrolled with a payer for electronic claim services through theclearinghouse, eligibility services are automatically provided (if the payer also offers eligibility services). The onlyexceptions to this are for the following payers: Medicare for all states, Georgia BC/BS, Florida Medicaid, FloridaBlue Shield, and California Blue Cross (these payers do require authorization for eligibility services). For thesepayers Kareo will request eligibility services with the clearinghouse for you.You will be responsible for completing the agreements, identifying yourself as the contact to be notified by thepayers regarding your enrollment status, and getting your providers’ signatures. Each payer agreement providesinstructions for completing the agreement. Generally, most payers require an original signed copy, but somepayers will accept agreements by fax. If so, the fax number will be provided on the agreement. Also some payershave other special requirements, such as provider signatures in blue ink and typed practice information. Pleasepay close attention to any special instructions provided within the payer agreement. If you should have anyquestions about completing a payer agreement, contact the payer directly for clarification.In addition to internal signatures, note that some payers (e.g., CA Medi-Cal - MC051, Maryland Medicaid –MC091, and Mississippi BC/BS – BS047) also require signature by the clearinghouse. If the payer agreement asksfor signature of submitter agent, billing service/biller signature or clearinghouse signature, this typically meansthat the agreement must be signed by the clearinghouse before being sent to the payer. In this case, thecompleted agreement must be sent to the clearinghouse to be signed. The clearinghouse contact information islisted in Section 4.3.Once you have completed the payer agreements and have obtained the appropriate signatures, you will need tosend them directly to the payer, or to the clearinghouse if so indicated. If sent to the clearinghouse for signature,the clearinghouse will sign the agreements and forward them to the payer. Again, please read the entireagreement and follow the instructions carefully. Note: Be sure to send payer agreements to the clearinghouseONLY when a clearinghouse signature is required. All other agreements are to be mailed directly to the payer.In most cases, you will be notified by the payer once the agreement has been received and approved. However,in some situations, a payer may not notify you but instead just approve and file your agreement. If you do nothear back from a payer within 10 to 15 days, you may wish to follow up with that payer to check on yourenrollment status. Once approved by a payer, you will then configure your enrollment settings within Kareo tobegin sending electronic claims to the approved payer. It is imperative that you do not set an insurance companyrecord within Kareo to live mode for these payers until you have received an approval notification by the payeror once you have verified enrollment by calling the payer directly.Section 7 provides a sample of a typical payer agreement. Note that payer agreements vary greatly, dependingon the requirements of the individual payer; but at least this sample will give you a fair idea of the morecommon agreements and how to complete them. 2014 Kareo, Inc. Rev. 3/114
3.4Transitioning to Kareo from Another Billing SystemIf a provider is new to electronic claims with any insurance payer that requires an enrollment agreement, youwill need to follow the steps as described in Section 3.3 above.However, if a provider is already submitting electronic claims to a specific payer using another billing system,some payers may NOT require the agreement typically you will only need to submit a change request form orletter to the payer requesting a change in submitter number. A letter template has been prepared for you forthis purpose, and can be downloaded from Kareo’s Help and Support Website athttps://help.kareo.com/documents/doc/Payer RequestToChangeSubmitterNumber Template. It isrecommended that you contact the EDI department of the insurance payer to verify their requirement as thisletter may not be accepted by all payers. You may also contact Kareo at enrollments@kareo.com if you havequestions.Clearinghouse submitter numbers (also referred to as a Trading Partner ID or Clearinghouse ID on certain payeragreements) are different per payer and clearinghouse. The former clearinghouse submitter number can befound on the provider’s original payer agreement or by contacting the former clearinghouse directly. The newsubmitter number can be obtained contacting Kareo at enrollments@kareo.comAdditional Requirements:3.5 If you are an existing GatewayEDI customer and you would like to transition a provider to Kareo who isalready enrolled with GatewayEDI through another billing system, you will submit a letter to Gatewayrequesting for the provider to be moved to Kareo site 11QZ. This letter should include the provider’sexisting Gateway site #. The letter should also include if the old site should be termed or left active andthe letter has to be on letterhead and signed by the provider. The letter can be faxed to
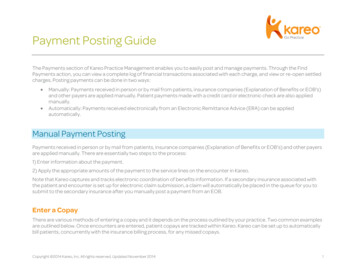
Kareo’s electronic claim services enable you to submit health care claims directly from the Kareo application, through our third-party clearinghouse partners, to over 3,000 government and commercial insurance payers. Kareo’s electronic claim services also include the deli