Transcription
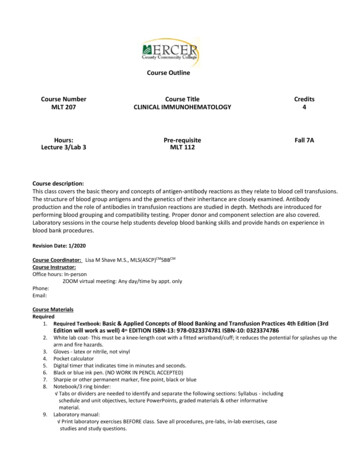
Back To Chiropractic CE SeminarsChiropractic Technique 4 HoursWelcome to Back To Chiropractic Online CE exams:This course counts toward your California Board of Chiropractic Examiners CE.(also accepted in other states, check our website or with your Chiropractic State Board)The California Board requires that you complete all of your CE hours BEFOREthe end of your Birthday month. We recommend that you send your chiropracticlicense renewal form and fee in early to avoid any issues.COPYRIGHT WARNINGThe copyright law of the United States (Title 17, United States Code) governs the making of photocopies or otherreproductions of copyrighted material. Under certain conditions specified in the law, libraries and archives are authorizedto furnish a photocopy or other reproduction. One of these specified conditions is that the photocopy or reproduction is notto be "used for any purpose other than private study, scholarship, or research." If a user makes a request for, or later uses,a photocopy or reproduction for purposes in excess of "fair use," that user may be liable for copyright infringement. Thissite reserves the right to refuse to accept a copying order if, in its judgment, fulfillment of the order would involve violationof the copyright law.
Exam Process: Read all instructions before starting!1. You must register/pay first. If you haven't, please return to: backtochiropractic.net2. Open a new window or a new internet tab & drag it so it's side-by-side next to this page.3. On the new window or new tab you just opened, go to: backtochiropractic.net website.4. Go directly to the Online section. DON'T register again.5. Click on the Exam for the course you want to take. No passwords needed.6. Follow the Exam instructions.7. Upon passing exam (70%), you’ll be able to immediately download your certificate,and it’ll also be emailed to you. If you don’t pass, you must repeat the exam.Please retain the certificate for 5 years. DON’T send it to the state board.If you get audited and lose your records, I’ll have a copy.I’m always a phone call away. 707.972.0047 or email: marcusstrutzdc@gmail.comMarcus Strutz, DCBack To Chiropractic CE Seminars33000 North Highway 1Ft Bragg CA 95437
Chiropractic TechniqueOnline CoursePresented by:Dr. Lauren Ragazzo, D.C.For Back to Chiropractic
Dr. Lauren Ragazzo, D.C.Why I became a chiropractor instead of a pediatrician: Ihad Migraine Headaches for seven years- unresolved withmultiple neurologists and medications; a doctor ofchiropractic resolved this for me in three months. I worked as the Patient Care Coordinator for theUniversity of Utah Hospital. I then obtained my Associate of science degree fromSalt Lake Community College, as a part of their premed track I then attended Life University, where I completed myBachelor's of Science Degree in Biology. I was quickly accepted into the nationally ranked LifeUniversity College of Chiropractic in Atlanta, where Ithen received my Doctor of Chiropractic Degree fouryears later. I did my internship with Dr. Jessica Gold in EncinitasCalifornia, where I began to work with UFC and MMAfighters, in addition to family practice for wellnesscare. I began the chiropractic department for several FQHCfacilities which include: Neighborhood Healthcare, theSan Marcos chiro branch for North County HealthServices, and Family Health Centers of San Diego.
My focus in private practice: Postural correction via: gravity based traction Wellness care Treating the injuries of professional athletes
How might my experience differ, by working in a FQHC? I’m working with the underservedcommunities, therefore:I typically see patients who have not hadconsistent health care. I am often their first doctor of chiropractic I typically see extreme cases every day inpractice which include:severe disc herniation, failed surgeries, ahistory of severe physical trauma, multipleco-morbidities, dependent on painmedication and injections, patients whoshould be sent to the E.R. for their currentcondition
This course will utilize the followingformat: We’re going to look at specific case studies:––––Patient historyExaminationImagingDiagnosis All of this information will be integrated:– So that the information we’re learning has real worldapplication– We can connect the technique with the history,imaging an exam findings .– (As opposed to individual subjects)
Case #1 A 49 year old male returns to your office for afollow up appointment, after receiving onechiropractic adjustment During the initial appointment his chiefcomplaint was: lower back pain– Which was a 7/10 pain scale– Site L3-S1
I was fortunate enough to have imaging on filefor this patient: 1)thoracic x-ray: s-shaped scoliosis (thoracicdextro, lumbar levo)2) lumbar x-ray: L4 anterolisthesis3) lumbar mri: six lumbar vertebrae: L1: discbulge, L2: disc bulge contacting the thecal sac,L3 disc bulge at thecal sac, L5 anterolisthesis,L6-S1 disc bulge
What was the diagnosis for this patient so far basedon the imaging? DX: lumbar disc displacement,lumbar djdanterolisthesis of the lumbar vertebraesix lumbar vertebraedextroscoliosis of thoracic spinelevoscoliosis of the lumbar spine
*Break down the imaging into thespinal levels we are avoiding first.*Then notate levels that may betreated with gentle chiropractic care(activator typically) Which spinal levels should we avoid?
The vertebrae are subluxated anterior– Adjusting them P-A would make them worse It may be hard to isolate the other vertebrae inside posture, with a scoliosis curvature This patient has multiple levels of herniated discs! Side posture/ diversified may irritate a disc bulge ormake it worse if we’re using a shearing motion to adjust
What else stood out about hisimaging reports?
*He has six lumbar vertebrae!– What a weirdo– You should always palpate and count your spinallevels before adjusting (be specific!)*What else might be important?-He has two disc bulges which are touching thethecal sac!-Which levels were those?
L2-L3 @ the thecal sac What does that mean again?– The disc is touching the outer covering of the spinal cord– That’s bad.– We should probably be careful here
What would this condition look like onan MRI?(not the MRI of this case study)
How would we adjust this patient? (note: I can only see these patients 2x permonth as per medi-cal) Adjustment: thoracic spine: gentlediversified/drop Lumbar spine: low force activator device withthe avoidance of L4-L5 (anterolisthesis) Supine SOT blocks at L6
What was the outcome? Outcome: lbp decreased from 7/10 tointermittent 4/10 within one adjustment
Case #2 53 year old male, with chronic lower back painthirty years in duration Has a history of multiple gunshot wounds(Injury occurred approximately Thirty yearsago)
His Lumbar radiology report: FINDINGS: BONES: Normal. No significant spondylosis, scoliosis, fracture, orvisible bony lesion. DISC SPACES: There is moderate degenerative disc disease at theL4-5 level. Mild degenerative disc disease at the L1-2, L2-3, L3-4and L5-S1 levels. PARASPINOUS: There are two bullets within the central posteriortissues and the right paramedian posterior tissues. OTHER: There appears to be a small bullet fragment within the leftside of the sacral canal. CONCLUSION: Small bullet fragment within left side of the sacral canal. Bulletfragments within the posterior soft tissues. Moderate degenerativechanges
Initial adjustment approach The patient was laying PRONE With SOT blocks under the superior pelvisbilaterally (to increase disc spaces) The Activator device was utilized to adjust alllumbar subluxations The sacrum was avoided
How did the patient respond? He didn’t. No change for three visits (did I mention that Ionly get six visits with a referral?) So I looked at his x-rays myself to see if I coulddo more
What did I notice? The bullet fragments were very far from thespine itself and they were adjacent to T10 andT12 (I documented this on every visit so I wasaware) The Sacral bullet fragment was not in thesacral canal. It was lodged in the left sacralbase and was not in an area where nerveswould be compromised
In case you were wondering I’ve treated a lot of patients who have beenshot The first patient was a surprise Five patients later, my eyes don’t get as bigduring the patient history
So how did I change this patients care? The drop table was utilized for three visits. The thoracic and lumbar spine were adjustedas well as the sacrum With the activator utilized for: T10 and T12when necessary
How did the patient respond? He was feeling much better! Pain reduced from 7/10 to 0/10, after 30 years ofchronic pain
However, he had a two month lapse incare after this Following a 2 month lapse in care, pain hadreturned to 7/10 He needed to remain on a wellness areprogram Patient education regarding maintenance isvery important He is currently feeling well again, and I seehim every two weeks!
Anatomical review of: the lumbarspine, pelvis and sacrum
Assessment Protocol: Radiographicand Manual Examination Procedures BP or Base Posterior sacrum:– The definitive assessment for a posterior sacral baseor posterior sacral apex is based on a laterallumbopelvic or sacral spot-shot radiograph. On X-ray,a posterior sacral base is indicated by the following onthe lateral view: 1) A decrease in the sacral base angleto less than 36 degrees; 2) Hypolordosis of the lumbarspine; 3) Posteriority of the sacral base George‘s linerelative to L5; 4) A posterior open wedge at the L5-S1disc space.1-2Text provided by Dynamic Chiropractic
Physical examination assessment of BPSacrum: Motion palpation may reveal extensionfixation at L5-S1.2 Patients with a baseposterior sacrum usually can stand erect withno significant forward antalgia, but they maydemonstrate a positive Minor's sign whenrising from a seated position.Text provided by Dynamic Chiropractic
Review of Sacral adjusting: Can be adjusted several ways:– prone with a drop table– Posture– Activator technique
Prone drop adjustmentImage courtesy of Dynamic Chiropractic
Manual Adjustment of BP Sacrum– Contact: second sacral segment– LOD: inferior-to-superior (I-S) and posterior-toanterior (P-A)
Nutation and Counternutation:Nutation - occurs as the sacrum moves anteriorly andinferiorly while the coccyx moves posteriorly relativeto the Ilium.[3]Counternutation - occurs as the sacrum movesposteriorly and superiorly while the coccyx movesanteriorly relative to the Ilium.[3] This motion isopposed by the posterior sacroiliac ligament that issupported by the multifidus.https://www.physio-pedia.com/Sacroiliac joint
Case #3 58 year old male presents with chronic lowerback pain (at the sacral area) approximatelyone year in duration, and right “trochanter”pain that is sharp approximately three monthsin duration. The patient has an abnormal gaitwhere he is favoring the right leg. He also hasan anterior antalgic lean at the waist.
RELEVANT HISTORY: approximately one year ago: thepatient had fallen out of a hospitalbed onto the floor. He landed flat onhis back.
What do we think is wrong withthis patient?(AKA: DIAGNOSIS)
IMAGING RESULTS: lumbar x-ray: djd, loss of lumbar lordosis,levoscoliosis lumbar mri: mild disc bulge at L3,retrolisthesis of L4
At this point what is our workingdiagnosis?
PHYSICAL EXAM FINDINGS: Valsavas: positive for the lumbar spine area Lumbar ROM: restricted with flexion (could reach to thetibias and pain began), lumbar rotation 5 degrees only ineither direction elicited pain palpation: edema and joint fixation at the right sacral base,joint fixation L2-5; kemps test: positive with right rotation, PAIN ON THE RIGHT SLR: negative Belts test: positive for decreased pain with pelvic/SACRALstabilization LE Sensation and muscle testing: all muscle testing wnl;hyperesthesia on the RLE all dermatomes
What does the patient have so far? lumbar disc displacement (positive Valsavas andbulge noted on MRI at L3) lumbar radiculopathy (hyperesthesia in the RLE) lumbar djd (as noted on x-ray and MRI andpositive Kemps) lumbopelvic sprain strain (positive belts test forsacral involvement) right hip pain (the patient complains of pain andhe is favoring this leg with his gait)
The Adjustment: prone drop table 1) right base posterior sacrum 2) L2, L3, L5- body right/spinous left dropadjustment 3) (right apparent short leg of 3”) PI Ilium onthe right, AS Ilium on the left.
The result following this adjustment: LBP decreased from 7/10 to 1/10 right greater trochanter pain resolved (90% ofmy patients with hip pain improve with theadjustment of the sacrum and pelvis. I rarelyadjust the hip) (Side note: please stop pulling on patient’slegs! ) gait WNL anterior antalgia resolved.
Joint fixations that are often missed: T1 Rib Lunate/capitate for carpal tunnel (A-Padjustment) Sacral adjustment Pelvis adjustments (most often PI; howeverassess for PI, AS, IN and EX) Lateral tracking of the patella Posterior fibula head
T1 Rib Subluxation: symptoms, palpation andadjustment of
T1 Rib Subluxation symptoms: Neck PainShoulder PainDiscoloration of the extremityDecreased temperature of the extremityArm and Hand Numbness (abnormaldermatomes also/hypoesthesia) Limited cervical rotation
Lunate/capitate for carpal tunnel (A-P adjustment) Symptoms? (numbness tingling and weakness in themedian nerve distribution) orthopedic tests for carpal tunnel: (tinels wrist,phalens and reverse phalens) palpation and adjustment of the Carpal bones
Sacral subluxationThe first thing I check!!!BP sacrum; Right base posterior/ left sacral apex; Left Baseposterior/right sacral apex; BA sacrum
Pelvic misalignments: Pelvis adjustments (most often PI) however assess for PI, AS, IN and EX)
Review of Knee Joi
Chiropractic Technique Online Course Presented by: Dr. Lauren Ragazzo, D.C. For Back to Chiropractic . Dr. Lauren Ragazzo, D.C. Why I became a chiropractor instead of a pediatrician: I had Migraine Headaches for seven years- unresolved with multiple neurologists and medications; a doctor of chiropractic resolved this for me in three months. I worked as the Patient Care Coordinator for the .File Size: 1MBPage Count: 106





![Tier 1 Chiropractic Directory [as of April 2018]](/img/8/chiropractic-tier1.jpg)