Transcription
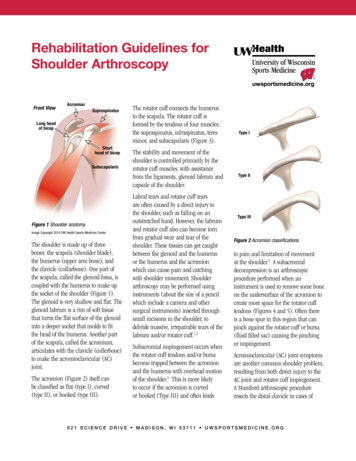
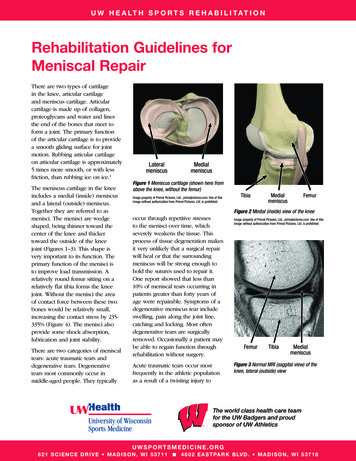
U W H E A LT H S P O R T S R E H A B I L I T A T I O NRehabilitation Guidelines forMeniscal RepairThere are two types of cartilagein the knee, articular cartilageand meniscus cartilage. Articularcartilage is made up of collagen,proteoglycans and water and linesthe end of the bones that meet toform a joint. The primary functionof the articular cartilage is to providea smooth gliding surface for jointmotion. Rubbing articular cartilageon articular cartilage is approximately5 times more smooth, or with lessfriction, than rubbing ice on ice.1The meniscus cartilage in the kneeincludes a medial (inside) meniscusand a lateral (outside) meniscus.Together they are referred to asmenisci. The menisci are wedgeshaped, being thinner toward thecenter of the knee and thickertoward the outside of the kneejoint (Figures 1–3). This shape isvery important to its function. Theprimary function of the menisci isto improve load transmission. Arelatively round femur sitting on arelatively flat tibia forms the kneejoint. Without the menisci the areaof contact force between these twobones would be relatively small,increasing the contact stress by 235335% (Figure 4). The menisci alsoprovide some shock absorption,lubrication and joint stability.There are two categories of meniscaltears: acute traumatic tears anddegenerative tears. Degenerativetears most commonly occur inmiddle-aged people. They typicallyLateralmeniscusMedialmeniscusFigure 1 Meniscus cartilage (shown here fromabove the knee, without the femur)Image property of Primal Pictures, Ltd., primalpictures.com. Use of thisimage without authorization from Primal Pictures, Ltd. is prohibited.TibiaMedialmeniscusFemurFigure 2 Medial (inside) view of the kneeoccur through repetitive stressesto the menisci over time, whichseverely weakens the tissue. Thisprocess of tissue degeneration makesit very unlikely that a surgical repairwill heal or that the surroundingmeniscus will be strong enough tohold the sutures used to repair it.One report showed that less than10% of meniscal tears occurring inpatients greater than forty years ofage were repairable. Symptoms of adegenerative meniscus tear includeswelling, pain along the joint line,catching and locking. Most oftendegenerative tears are surgicallyremoved. Occasionally a patient maybe able to regain function throughrehabilitation without surgery.Acute traumatic tears occur mostfrequently in the athletic populationas a result of a twisting injury toImage property of Primal Pictures, Ltd., primalpictures.com. Use of thisimage without authorization from Primal Pictures, Ltd. is prohibited.FemurTibiaMedialmeniscusFigure 3 Normal MRI (saggital view) of theknee, lateral (outside) viewThe world class health care teamfor the UW Badgers and proudsponsor of UW AthleticsUWSPORTSMEDICINE.ORG621 SCIENCE DRIVE MADISON, WI 53711 4 6 0 2 E A S T PA R K B LV D . M A D I S O N , W I 5 3 7 1 8
Rehabilitation Guidelines For Mensical RepairwithoutmeniscuswithmeniscusFigure 5 MRI (saggital view) of a lateralmeniscus tear (yellow arrows)Figure 4 Schematic representation of the meniscal effect on contact pressure in theknee. Contact area is increased by 50% with addition of menisci. This reduces contact pressures.FemurMeniscusTibiaFigure 6 Perimeniscular capillary plexus (thick arrow) providing blood supply to theouter third of the meniscus.the knee when the foot is planted.Symptoms of an acute meniscus tearinclude swelling, pain along the jointline, catching, locking and a specificinjury. Often times these tears canbe diagnosed by taking a thoroughhistory and completing a physicalexamination. An MRI may be usedto assist in making the diagnosis. Ifan athlete suffers a meniscal tear,the three options for treatmentinclude: non-operative rehabilitation,surgery to trim out the area of tornmeniscus, or surgery to repair (stitchtogether) the torn meniscus. Thetreatment chosen will depend onthe location of the tear, the athlete’ssport, ligamentous stability of theknee and any associated injury.2 Thelocation of tear is important becausethe outer portion of the meniscushas a good blood supply whereas2UWSPORTSMEDICINE.ORG621 SCIENCE DRIVE MADISON, WI 53711 the inner portion has a very poorblood supply. Figure 6 shows theblood vessels (perimeniscular capillaryplexus) entering the outer portionof the meniscus.3 This blood supplyis necessary for a tear or a repair toheal. Without an adequate bloodsupply, the area of torn meniscus willhave to be removed.After mensical surgery, rehabilitationwith a physical therapist or athletictrainer is needed to restore range ofmotion, strength, movement controland guide the athlete’s return to sport.When the meniscus is repaired theremay be a period of restricted kneeflexion, especially during weightbearing, to protect the repair suturesand the meniscus. The rehabilitationguidelines are presented in a criterionbased progression. Specific timeframes, restrictions and precautionsare given to protect healing tissuesand the surgical repair/reconstruction.General time frames are also given forreference to the average individual ,but individual patients will progress atdifferent rates depending on their age,associated injuries, pre-injury healthstatus, rehabilitation compliance andinjury severity. The size and locationof the meniscal tear may also affectthe rate of post-operative progression.4 6 0 2 E A S T PA R K B LV D . M A D I S O N , W I 5 3 7 1 8
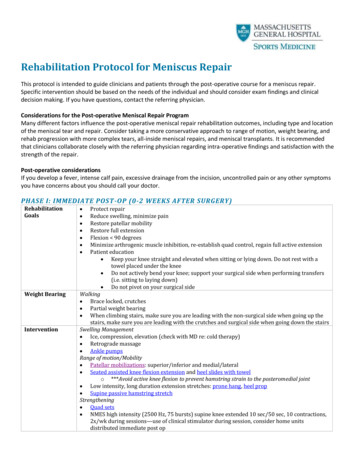
Rehabilitation Guidelines For Mensical RepairPHASE I (Surgery to 4 weeks after surgery)Note: The physician may extend this phase to 6 weeks for large repairs.3Appointments Rehabilitation appointments begin 3-5 days post-operatively and thenapproximately 1 time per weekRehabilitation Goals Precautions The patient may gradually wean from two crutches to one crutch to no crutchesas long as the knee is in the locked knee brace, and there is no increase in painor swelling for 4 weeks. Knee brace locked for all weight bearing activities for 4 weeks Do not flex the knee past 90 Range of Motion Exercises Suggested Therapeutic Exercise Cardiovascular Exercise Upper body circuit training or upper body ergometerProgression Criteria 4 weeks after surgery Pain-free gait without crutches No effusion (swelling)Protection of the post-surgical kneeRestore normal knee extensionEliminate effusion (swelling)Restore leg controlKnee extension on a bolsterProne hangsSupine wall slidesHeel slides (caution with posterior medial meniscus repair secondary to thesemimembranosus insertion) Knee flexion off the edge of the tableQuadriceps setsStraight leg raises4 way leg lifts in standing with brace on for balance and hip strengthAbdominal isometricsUWSPORTSMEDICINE.ORG621 SCIENCE DRIVE MADISON, WI 53711 4 6 0 2 E A S T PA R K B LV D . M A D I S O N , W I 5 3 7 1 8
Rehabilitation Guidelines For Mensical RepairPHASE II (begin after meeting Phase I criteria, usually 4 weeks after surgery)4Appointments Rehabilitation appointments are once every 1-2 weeksRehabilitation Goals Single leg stand control Normalize gait Good control and no pain with functional movements, including step up/down,squat, partial lunge (between 0 and 60 of knee flexion)Precautions No forced flexion with passive range of motion with knee flexion or weightbearing activities that push the knee past 60 of knee flexion Avoid post-activity swelling No impact activitiesSuggested Therapeutic Exercise Cardiovascular Exercise Non-impact endurance training: stationary bike, Nordic track, swimming, deepwater running or cross trainerProgression Criteria Normal gait on all surfaces Ability to carry out functional movements without unloading affected (injured)leg or pain, while demonstrating good control Single leg balance greater than 15 secondsNon-impact balance and proprioceptive drillsStationary bikeGait drillsHip and core strengtheningStretching for patient-specific muscle imbalancesQuadriceps strengthening, making sure that closed chain exercises occurbetween 0 and 60 of knee flexionUWSPORTSMEDICINE.ORG621 SCIENCE DRIVE MADISON, WI 53711 4 6 0 2 E A S T PA R K B LV D . M A D I S O N , W I 5 3 7 1 8
Rehabilitation Guidelines For Mensical RepairPHASE III (begin after meeting Phase II criteria, usually 3 months after surgery)Appointments Rehabilitation appointments are once every 1 to 2 weeksRehabilitation Goals Good control and no pain with sport and work specific movements, includingimpactPrecautions Post-activity soreness should resolve within 24 hours Avoid post-activity swelling Avoid posterior knee pain with end range knee flexionSuggested Therapeutic Exercise Impact control exercises beginning 2 feet to 2 feet, progressing from 1 foot tothe other and then 1 foot to the same foot Movement control exercises beginning with low velocity, single plane activitiesand progressing to higher velocity, multi-plane activities Strength and control drills related to sport specific movements Sport/work specific balance and proprioceptive drills Hip and core strengthening Stretching for patient specific muscle imbalancesCardiovascular Exercise Replicate sport or work specific energy demandsReturn To Sport/Work Criteria Dynamic neuromuscular control with multi-plane activities without pain orswellingThese rehabilitation guidelines were developed collaboratively by Marc Sherry, PT, DPT, LAT, CSCS and theUW Health Sports Medicine physician group.Updated 11/2017REFERENCES1. Ulrich GS and Aronczyk SP. The basicscience of meniscus repair. Tech in Ortho,8(2): 56-62, 1993.2. Fowler PJ and Pompan D. Rehabilitationafter mensical repair. Tech in Ortho, 8(2):137-139, 1993.3. Arnoczky SP and Warren RF.Microvasculature of the human meniscus.Am J Sport Med, 1982.At UW Health, patients may have advanced diagnostic and /or treatment options, or may receive educational materials that vary from this information. Please be aware that this information is not intended to replacethe care or advice given by your physician or health care provider. It is neither intended nor implied to be a substitute for professional advice. Call your health provider immediately if you think you may have a medicalemergency. Always seek the advice of your physician or other qualified health provider prior to starting any new treatment or with any question you may have regarding a medical condition.Copyright 2017 UW Health Sports MedicineUWSPORTSMEDICINE.ORG621 SCIENCE DRIVE MADISON, WI 53711 4 6 0 2 E A S T PA R K B LV D . M A D I S O N , W I 5 3 7 1 8SM-101781-175
UW Health Sports Medicine physician group. Updated 11/2017 REFERENCES At UW Health, patients may have advanced diagnostic and /or treatment options, or may receive educational materials that vary from this information. Please be aware that this information is not intended to replace the