Transcription
June 22, 2022V.3 6-22-2022 FNL
LETTER FROM PARAMOUNT PRESIDENTPage 6COMMUNICATE WITH PARAMOUNTPage 7CLAIMSPage 13UTILIZATION MANAGEMENTPage 17BEHAVIORAL HEALTHPage 25MyParamount: Online PortalParamounthealthcare.com: WebsiteProvider Inquiry and Provider RelationsOutreach ActivitiesProvider NoticesProvider NewsProvider NewsletterMember EducationImportant Contact InformationUpdate Your Contact InformationHow to Submit a ClaimElectronicPaper ClaimsHIPAA 5010 TransactionsClaim RequirementsPayment Processing GuidelinesSubmission Timely FilingProcedure/Diagnosis CodesCode Editing SoftwareOverviewUtilization Care Management ProcessCare Management ProgramCare Management GoalsRole of PhysicianHow to Make a Referral to Care ManagementReferralsOutpatientInpatient/Acute CarePrior AuthorizationsTruCare ProAuth PortalProvider AppealsRequired DocumentationLevels of AppealAppeal Filing TimeframeRetrospective ReviewsPeer-to-Peer ReviewsBehavioral Health Redesign (Medicaid)Prior AuthorizationsCommercial and Elite MedicareHospital and Inpatient Observation AdmissionsOutpatient Services2
QUALITY IMPROVEMENTPage 28POPULATION HEALTHPage 31PHARMACYPage 36OverviewQuality MeasuresPractitioner and Provider RequirementsHEDIS CAHPS Paramount Access StandardsClinical Practice GuidelinesOverviewHow It WorksCondition-Specific ProgramsAsthma, CHF, CKD, COPD, Diabetes,Depression, Migraine Headache,Osteoporosis Fracture, Post Cardiac Event,Reproductive HealthPrescription Drug CoverageCommercial, Marketplace ExchangeAdvantage MedicaidElite MedicarePrior Authorizations and ExceptionsCommercial, Marketplace Exchange, Advantage MedicaidMedicareSpecialty Drugs and Specialty NetworkInfusions/InjectionsLimited Medical SuppliesOver-the-Counter Drug CoverageDrug FormularyCommercialMarketplace ExchangeAdvantage MedicaidPARAMOUNT PRODUCT LINESMEDICAID MANAGED CARE PLANOverviewMember Enrollment and EligibilityMember ID CardNew Member Welcome MaterialsEnrollmentDisenrollmentProvider Guidelines and ProceduresFinancial Responsibility Notification ProcedureMember Rights and ResponsibilitiesMember Termination ProcedureHealthchekLead Testing RequirementPrenatal Risk Assessment ProcedureSterilization, Hysterectomy, Abortion Procedures3Page 40
MEDICAID PLAN CONTINUEDMember Services24/7 Nurse LineMember Services Call CenterInterpreter ServicesTransportation AssistanceMember Incentive ProgramsPrenatal to Cradle RewardsCradle to Crib RewardsNFL Healthy RewardsMEDICARE PLANSPage 51COMMERCIAL HEALTH PLANSPage 58OverviewMember Enrollment and EligibilityOverview of PlansEligibilityEnrollmentDisenrollmentMember ID CardMember Welcome MaterialsStar RatingProvider Guidelines and ProceduresMember Rights and ResponsibilitiesMember Notification of Network ChangesMember Services24/7 Nurse LineInterpreter ServicesMember Services Call CenterPersonal Call Center RepLive ChatOnline Member PortalMember ProgramsAnnual Physical ExamDental BenefitHearing BenefitMeal BenefitOver-the-Counter BenefitSilver Sneakers Virtual Doctors' VisitsWellness IncentivesWorldwide CoverageOverviewMember Enrollment and EligibilityOverview of PlansEnrollmentMember ID CardMember Welcome MaterialsProvider Guidelines and ProceduresMember Rights and ResponsibilitiesMember Termination Procedure4
COMMERCIAL PLANS CONTINUEDMember Programs/Services24/7 Nurse LineMember Services Call CenterPersonal Call Center RepLive ChatOnline Member PortalSummary of Benefits and CoverageDependent Child CoverageVirtual Doctors' VisitsMARKETPLACE EXCHANGE PLANSPage 63DENTAL PLANSPage 66COMPLIANCEPage 67OverviewMember Enrollment and EligibilityOverview of PlansEligibilityEnrollmentProvider Guidelines and ProceduresMember Termination ProcedureMember Services and Programs24/7 Nurse LineMember Services Call CenterPersonal Call Center RepLive ChatOnline Member PortalSummary of Benefits and CoverageVirtual Doctors' VisitsWellness IncentiveHIPAA Requirements and InformationDuties of ProvidersUses and Disclosures of PHIWritten AuthorizationsUnintentional DisclosuresCybersecurityStark I, II & IIIAnti-KickbackFalse Claims ActAntitrust ComplianceCompliance HotlineFraud, Waste and Abuse (FWA)IntroductionDefinitionMission and GoalsExamplesResponse and ReportingPrepayment FWA ActivitiesPost-payment FWA Claims System AuditsPost-payment RecoveriesClaims AuditsProvider/Practitioner Education5
Dear Paramount Provider:Thank you for being a valued Paramount partner. Please know, we arealways looking for ways to make your job easier. The purpose of thismanual is to serve as your guide to navigating Paramount policies,programs, processes, procedures, and member benefits for each of ourplans.At Paramount, high-quality, responsive, and simplified insurance is whatdrives us. The health and satisfaction of our members is our top priority.We consistently work to create innovative insurance products that meetthe demands of our members throughout their lives.Remember, you can access the myParamount online portal or callour provider inquiry team at 888-891-2564 for claim and priorauthorization statuses, member benefits and eligibility.Our provider relations team is on hand if you have additional questions.Please call 800-891-2542. In addition, stay informed on Paramount’slatest provider news by visiting ParamountHealthcare.com/provider news.We look forward to our continued partnership and to meeting our sharedgoal of reaching optimal outcomes for patient members.Thank you,Lori A. Johnston, President, Paramount Health Care6
COMMUNICATE WITH PARAMOUNTOur goal is to ensure that you, our providers, always have convenient access to the informationyou need from Paramount.The main resources available to you are the MyParamount online portal (the best place to start),our paramounthealthcare.com/providers website, and our provider inquiry and provider relationsteams.In addition, we have outreach activities in place to bring important announcements and helpfulnews right to you.MYPARAMOUNT: ONLINE PORTALThe myParamount portal is your central resource for claims, prior authorizations, and membercoverage details. The online portal is password protected and HIPAA compliant. It allows you to: Find participating providersSend and receive messages to/from our provider inquiry team through the messagecenterSubmit and view claims information, such as diagnosis and procedure codes, andpayment statusSubmit and view prior authorizationsView and download EOPs (explanations of payment)View member eligibility and benefits information, including their health insurancecarrier, policy number, and effective dates of coverageView panels of members assigned to primary care providersTo register for an account, please take the following steps:1. Visit myParamount.org2. Choose “Provider Registration” in the top right corner3. Review and accept the Terms of Use Agreement, which states that our portal is inaccordance with HIPAA privacy regulations and Paramount policies. Then, click“Next”4. Enter your tax ID, your 5-digit Paramount provider ID or NPI number, and a recentclaim number (for access to claims information). Then, click “Next”5. Complete the registration instructions, and then click “Submit”6. Once you have completed these steps, you will receive an email with a link to finishyour registration.Note: We recommend designating an administrator from your practice. Theadministrator can assign access levels to other members of the practice,designate user roles, and add or remove additional users.7
PARAMOUNTHEALTHCARE.COM: WEBSITEVisit our website: ParamountHealthcare.com/providers. There, you’ll find Paramount providernews updates, medical and reimbursement policy libraries, information on prior authorizationcriteria, prescription drug benefits and electronic claims submission, as well as details on ourcondition management, utilization management, and member incentive programs. We alsoprovide a tools and resources section with commonly used documents, forms and frequentlyasked questions.PROVIDER INQUIRY AND PROVIDER RELATIONS DEPARTMENTSIf you cannot find the information you need on MyParamount orparamounthealthcare.com/providers, please contact Paramount’s provider inquiry team at 888891-2564. Representatives are available to assist you Monday – Friday, 8:30 a.m. – 5 p.m.For more complex issues, please work with your provider relations representative. You can callprovider inquiry or provider relations at 800-891-2542 to get connected with your designatedprovider relations representative.OUTREACH ACTIVITIESParamount uses a variety of methods to communicate with its provider network, includingprovider notices sent via email and fax, updates posted on paramounthealthcare.com on theprovider news page, twice-a-year Network News newsletter, direct phone calls, and in-personoutreach.Provider Notices8
Paramount sends frequent email and fax communications to its network regarding policychanges, new program requirements, and important announcements to keep you informed.Provider Notice sample:To guarantee timely delivery, please ensure that we have your most recent email address onfile. If we do not have your email address or you would like to change it, please complete andsubmit our Provider Information Change Form. Note: Any forms printed from links in this manualare current as of this print date.Provider NewsTo stay up to date on Paramount News and policies, as well as government announcements,please visit the provider news section on our website at ParamountHealthcare.com/providernews.Provider Newsletter9
Published twice a year as a service for our provider and office manager community, theParamount Network News is mailed to offices and posted on our website.Each issue includes valuable information for Paramount providers, such as: Care management referral instructionsClaims management and clinical document suggestionsClinical practice guidelinesHealth care access and availability standards expectationsFormulary and prescribing criteriaMedical Advisory Council decisionsMember rights and responsibilitiesProgram evaluations and survey resultsQuality improvement initiativesSpecial program informationUtilization management practicesMember EducationParamount actively reaches out to members on the following initiatives: Colorectal cancer screenings: Fit Kit information for patients who are due for acolonoscopyDiabetes testing: Annual mailing to members who have missed diabetes testingHepatitis A: Health Information about vaccinationsMedication reconciliation: Member education about medication reconciliationMember incentive programs and other services: Printed and online member materialsPreventive cancer screenings: Annual mailing to members who have missed preventiveservicesIf you would like to learn more about these initiatives or would like to request printed materialsfor your office, please contact Paramount’s provider relations department at 800-891-2542.10
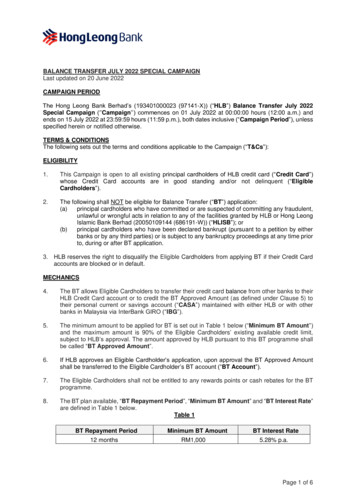
IMPORTANT CONTACT INFORMATIONBelow is a complete list of Paramount departments and contact information for each.DEPARTMENTASSISTANCE AVAILABLECONTACTCredentialingMonday – Friday8:30 a.m. – 5 p.m. New provider applicationsRe-credentialing questionsEmail: PHCCredentialing@ProMedica.orgMember ServicesMedicaidMonday - Friday7 a.m. – 7 p.m. Member questions and complaintsPrimary care provider changerequestsInterpreter servicesTransportation issuesSpecial Needs documentationPhone: 800-462-3589Phone (TTY): 888-740-5670Fax: 888-740-0222Commercial,MarketplaceExchange, OBAMonday - Friday8 a.m. – 5 p.m. MedicareApril – SeptemberMonday – Friday8 a.m. – 8 p.m.October – MarchSunday– Saturday8 a.m. – 8 p.m.PharmacyMonday – Friday8:30 a.m. – 5 p.m. Obtaining drug priorauthorizationsPhone: 800-327-3974 (Magellan, medically billeddrugs)Fax: 844-256-2025 (Pharmacy)Provider InquiryMonday – Friday8:30 a.m. – 5 p.m. Member benefits and eligibilityClaim status inquiriesClaim processing issuesReferral/authorization verificationPhone: 419-887-2564Phone (TTY): 888-891-2564Fax: 419-887-2014Fax: 855-448-4705Email: Paramount.ProviderInquiry@ProMedica.orgProvider RelationsMonday – Friday8:30 a.m. – 5 p.m. Provider and office staff educationContract issuesOrientations/webinarsNew product participationrequestsRepresentative office visitrequestsPhone: 800-891-2542Fax: edica.orgInformation/questionsEmail: PHCquality@promedica.org QualityImprovementMonday – Friday8:30 a.m. – 5 p.m.11
Transportation(Medicaid members,only)Monday – Friday7 a.m. – 7 p.m. Modify/cancel ing/pick-upPhone: 866-837-9817Phone (TTY): 800-750-0750Must schedule two business days, andup to 30 business days, In advance.Utilization/CaseManagementMonday – Friday8 a.m. – 6 p.m. Obtaining in-plan and out-of-planprior authorizationsCase/care managementBH out-of-plan requestsGeneral clinical -282-4907844-282-4908Mental health, chemical dependencyGeneral inquiriesHome health careImagingInpatient, acute careMed., surg., DME, genetics, pre-DOut-of-planSNF, rehabilitation, LTACUPDATE YOUR CONTACT AND PROVIDER DIRECTORYINFORMATIONTo ensure our provider directory information is accurate and updated timely, Paramountrequires provider offices to notify the health plan of any of the following demographicchanges: Office locations and phone numbers Hospital affiliations Accepting new patients Additions to office/ group or terminationsParamount is requesting this information be shared as timely as possible, and within 30days of the provider office identifying the change(s). This is to ensure our members andyour patients can reach you when accessing care, and that our provider directoryreflects current and accurate information.12
CLAIMSHOW TO SUBMIT A CLAIMElectronicParamount strongly recommends electronic claims submission, through the provider's preferredclearinghouse or through myParamount portal, TransShuttle.Paramount currently accepts electronic claims submissions from a variety of clearinghouses. Inorder to submit claims using a clearinghouse vendor you will need to sign our Trading PartnerAgreement. Our list of clearinghouses, along with our Trading Partner Agreement form, areavailable on our website.If you would like to learn more about our electronic claims submission process, please visit ourwebsite or contact our Electronic Claims Submission (ECS) system coordinator at 419-8872532.Additionally, myParamount portal, TransShuttle, offers the following benefits to claimsprocessing: Convenient access: Available 24/7 at no additional costEnhanced capabilities: submit corrected claims, and void claimsTimely statuses: Check claims statuses and receive timely notification of changes instatusIf you need access to TransShuttle, please email proivderrelations.paramount@promedica.orgPaper ClaimsPaper claims need to comply with the same standards as those for electronic submissions, setforth by the American National Standards Institute (ANSI).Please review and adhere to the following requirements: 13Paramount will only accept the most current version of the industry standard CMS-1500(02-12) and UB-04 forms printed in red drop-out ink.Printed information should go on the reverse side of the form. All mandatory fields onpaper claim forms must be completed.Black and white versions of claim forms, including photocopied or faxed versions, andresized forms that do not replicate the scale and color of the standard claim form will notbe accepted.The size of the form should be 8 ½ X 11 with the printer pin-feed edges removed alongthe perforations.Forms should be free from excessive creases or tears. Do not fold or staple forms.Forms should be clean and free from stains, notations, strike outs, crossed out orhighlighted information, liquid correction tape, glue, and tape.Please use industry-standard procedure codes, diagnosis codes, location codes andmodifiers.
Paper claims should be mailed to: Paramount, P.O. Box 497, Toledo, OH 43697-0497Nonstandard forms will be returned to the address identified in Box 33 of the CMS-1500 form orBox 1 of the UB-04 form with instructions to resubmit the claim using the appropriate claim form.A new claim with the correct information must be submitted for the claim to be processed.HIPAA 5010 TRANSACTIONSIn 2009, the United States Department of Health and Human Services released a final rule toupdate standards for electronic health care and pharmacy transactions. This was in preparationfor implementing ICD-10 CM codes on October 1, 2015.The new standard is the HIPAA 5010 format. All trading partners and payers must be 5010compliant. For more information, please click here to visit the CMS Adopted Standards andOperating Rules webpage.CLAIM REQUIREMENTSYour National Provider Identifier (NPI) number and Tax Identification Number (TIN) are requiredon all claim’s submissions. Claims submitted without these numbers will be rejected. Pleasecontact your Electronic Data Interchange (EDI) vendor if you have questions regarding wherethese identifying numbers should be placed on your forms.Please note: On paper claims, the NPI number should be placed in the following boxes basedon form type: CMS 1500: Box 24J for the rendering Provider’s NPI and, if applicable, Box 33A for thegroup NPIUB04: Box 56ADA: Box 54 for the treating Provider’s NPI and, if applicable, Box 49 for the group NPIPAYMENT PROCESSING GUIDELINESProviders are responsible for the accuracy of claim submissions. Please adhere to the followingcoding requirements: 14For diagnoses: International Classification of Diseases, 10th Revision, ClinicalModification ICD-10-CMFor professional and outpatient procedures: The Healthcare Common ProcedureCoding System Level 1 (CPT codes), Level 2 and 3 (HCPCS codes)For inpatient hospital claims: ICD-10-PCS (International BD Classification ofDiseases, 10th Revision, Procedure Coding System)Claims must be coded in accordance with the HIPAA transaction code set guidelinesand follow the guidelines within each code set.
SUBMISSION TIMELY FILINGPlease visit the links below to view each the timely filing policy for each plan: Paramount Advantage MedicaidParamount Elite MedicareParamount CommercialPROCEDURE/DIAGNOSIS CODESProviders must bill for services using the most current CMS-approved diagnostic and proceduralcoding available for the date the service or for the date of discharge if the claim is an inpatientfacility claim.CODE EDITING SOFTWAREParamount utilizes comprehensive bundling logic software, which is fully automated to audit andverify the clinical accuracy of claims prior to payment. Our claims editing software applicationcontains a set of rules to address coding inaccuracies such as unbundling, frequencylimitations, fragmentation, up-coding, duplication, invalid codes, mutually exclusive procedures,and other coding inconsistencies. Each rule is linked to a generally accepted coding principle.Guidance surrounding the most likely clinical scenario is applied.The software is sophisticated and has clinical logic based on clinical practice andreimbursement standards, and input from medical experts. The software applies edits that arebased on the following sources: 15Centers for Medicare & Medicaid Services’ (CMS) National Correct Coding Initiative(NCCI) for professional and facility claims. NCCI status code indicator to determinepackaging or discounting, including medically unlikely edits (MUE), exclusive andoutpatient code editor (OCE) edits. These edits were developed by CMS to controlincorrect code combination billing contributing to incorrect payments. Public-domainspecialty society guidance (i.e., American College of Surgeons, American College ofRadiology, American Academy of Orthopedic Surgeons)CMS Claims Processing ManualCMS Medicaid NCCI Policy ManualState Provider Manuals, Fee Schedules, Periodic Provider Updates(bulletins/transmittals)CMS coding resources such as, HCPCS Coding Manual, National Physician FeeScheduleProvider Benefit Manual, Claims Processing Manual, MLN Matters and ProviderTransmittalsAMA resourcesCPT manualAMA websitePrinciples of CPT CodingCoding with ModifiersCPT Assistant
CPT Insider’s ViewCPT Assistant ArchivesCPT Procedural Code DefinitionsHCPCS Procedural Code DefinitionsBilling Guidelines Published by Specialty Provider AssociationsGlobal Maternity Package data published by the American Congress of Obstetriciansand Gynecologists (ACOG)Global Service Guidelines published by the American Academy of Orthopedic Surgeons(AAOS)State-specific policies and procedures for billing professional and facility claimsHealth Plan policies and provider contract considerationsMore information on Paramount code editing can be found in Reimbursement Policy RM013.16
UTILIZATION MANAGEMENTOVERVIEWUtilization management (UM) ensures effective and efficient medical care, including behavioralhealth care. Paramount’s UM Department performs internal reviews of medical policies andmedical criteria through a Medical Policy Steering Committee to ensure Paramount is utilizingthe most current clinically indicated criteria to perform medical necessity reviews. We evaluatethe cost and quality of medical services provided by participating physicians, hospitals, andother ancillary providers. To ensure appropriate utilization, we evaluate both potentialoverutilization and underutilization.Paramount’s UM department maintains the quality, efficiency and appropriateness of healthcareservices provided to Paramount members. We manage all UM activities, including priorauthorization processing, concurrent review, discharge planning, transition of care coordination,and more. Our goal is to ensure Paramount members receive the proper level of care in themost appropriate setting, and that the resources utilized align with their insurance plan benefits.Paramount adheres to nationally recognized criteria, medical policies, and state and federalguidelines to determine medical necessity and appropriateness of services. In addition, internalcriteria standards are in place for appropriateness of care and the existence of coverage whereother sources of standard are not defined.Our program focuses on the following objectives: To assure effective and efficient utilization of facilities and services through an ongoingmonitoring and educational program. Our program is designed to identify patterns ofutilization, such as overutilization, underutilization, and inefficient scheduling ofresources.To assure fair and consistent UM decision-making.To focus resources on a timely resolution of identified problems.To assist in the promotion and maintenance of optimally achievable quality of care.To educate medical providers and other healthcare professionals on appropriate andcost-effective use of healthcare resources.To ensure continuity in the transition of care process by fostering close collaboration withour case management team.For More InformationIf you have questions regarding our UM program, decisions or authorization of care, please visitour webpage or call us. The UM team is available at 800-891-2520, Monday – Friday, 8 a.m. –5:30 p.m. If you need to leave a voicemail after hours, we will return your call in one businessday. You can also visit paramounthealthcare.com/providers to find information anddocumentation related to: 17Medical policiesPrior authorization criteria, decision timeframes, and complete listPopulation health/condition management servicesPublications
Documents and forms: Forms printed from links in this manual are current as of the printdate.UTILIZATION CARE MANAGEMENT PROCESSParamount’s UM departmental operations policies and procedures are reviewed on an annualbasis. These policies and procedures serve as a framework of authority for our operationalteams.Our UM coordinators are authorized to approve prior authorization requests when medicalnecessity criteria are met based upon medical policies, InterQual criteria, clinical criteriasoftware, and/or appropriateness of care and services for covered services. Prior authorizationrequests which fail to meet medical policy and clinical criteria will be escalated to a medicaldirector for final review and determination of medical necessity.Paramount’s medical directors, associate medical directors, clinical directors, and pharmacistsare the only plan representatives who can deny payment for a service based on medicalnecessity/appropriateness.Neither providers nor internal Paramount staff are financially or otherwise compensated toencourage underutilization and/or denials.Paramount works cooperatively with its participating providers to assure appropriatemanagement of all aspects of the members' health care.The primary care provider (PCP) is responsible for coordinating all aspects of themember's health care. Conversely, the member is responsible for coordinating his/her medicaland behavioral health care through their PCP. Although in-network specialist referrals are notrequired by Paramount for claim payment, members are encouraged to seek their PCP’s advicebefore seeking specialist consultation and treatment.CARE MANAGEMENT PROGRAMOur care management program identifies and manages members who are at high risk forcomplex, costly or long-term healthcare needs. Our care managers are registered nurses (RNs)or social workers who: Coordinate care for members who have both behavioral health and medical conditions,often working together to enhance the member’s outcome.Work 1:1 with members and their PCP to ensure that medically appropriate services areprovided in a supportive cost-effective environment.Follow members through the continuum of care from home to office, home health care,in-patient hospitalizations, rehabilitation, skilled nursing facility, and help them transitionhome again.Assist with utilization of participating providers.Care Management Goals 18Treat members in the least restrictive and most cost-effective setting and manner.Empower members to acquire knowledge, decision-making ability, and alteration inlifestyle to promote positive health outcomes.
Support the PCP/specialist by reinforcing the treatment plan.Avoid complications and multiple admissions by early identification of problems anddevelopment of goals.Identify members who are inappropriately over utilizing the emergency room andeducate them to utilize PCPs for care whenever possible.Foster communication between the PCP, specialists, and ancillary providers.Decrease premature delivery by promoting prenatal care.Reduce the cost of care.Coordinate the services of social and public health agencies when applicable.Role of the PhysicianAs the primary care provider (PCP), you are responsible for coordinating all aspects ofmembers’ healthcare needs. Our care managers will assist you with the process.Please help us identify members who: Are experiencing a complicated pregnancyAre at high risk for frequent hospitalizationsAre at high risk for complicated pregnanciesAre potential transplant casesAre oncology patients with complicationsAre medically unstable or complexDo not adhere to their treatment plan, are non-compliant with medication management,and/or miss appointmentsHave special healthcare needsHave drug-seeking behaviorHave behavioral health needsInappropriately utilize the ERNeed specialized careThe Ohio Department of Medicaid (ODM), Center of Medicare & Medicaid Services (CMS), andNational Committee for Quality Assurance (NCQA) expects the evidence-based collaborativeefforts between case management and the primary care physician to influence positively thehealth and well-being of our members.How to Make a Referral to Care Management For medical care management, please send information to:Paramount.CM@ProMedica.org.For behavioral health care management, please send information to:PHCBH@ProMedica.org.A care manager will contact you if more information is needed prior to connecting with themember.19
REFERRALSOutpatientSpecialist Referrals: The primary care provider (PCP) may request a consultation from aparticipating specialist at any time. A referral is not required from Paramount prior toconsultation with any participating specialist.Emergency Room Services: Referrals are not required for treatment of an emergency medicalcondition that manifests itself by such acute symptoms of sufficient severity, including severepain, that a prudent layperson with an average knowledge of health and medicine couldreasonably expect the absence of immediate medical attention to result in any of the following: Placing the health of the individual or, with respect to a pregnant woman, the health ofthe woman, or her unborn child, in serious jeopardy.Serious impairment to bodily functions.Serious dysfunction of any bodily organ or part.Emergency Room services are covered if referred by an authorized plan representative, PCP,or plan specialist. A referral is not required for payment of Emergency Room services for anemergency medical condition; the plan may do retrospective claim review to ensure theappropriate level of service is reimbursed.Out-of-Plan Referrals: These requests are reviewed individually, and determinations are madebased on the patient's medical needs and the availability of services within the Provider Networkto meet these needs.Tertiary Care Services: All referrals to tertiary care centers are reviewed on an individualbasis. The member's medical needs and the availability of the requested services within thenon-tertiary care network are taken into consideration.Predetermination of Benefits/Outpatient Certification: Certain services, procedures, durablemedical equipment, and injectable medications require prior authorization. Additionally,cosmetic surgery and other procedures may be reviewed prospectively, at the request ofproviders an
accordance with HIPAA privacy regulations and Paramount policies. Then, click "Next" 4. Enter your tax ID, your 5-digit Paramount provider ID or NPI number, and a recent claim number (for access to claims information). Then, click "Next" 5. Complete the registration instructions, and then click "Submit" 6.