Transcription
Presented for the AAPC National ConferenceApril 4, 2011Penny Osmon, BA, CPC, CPC-I, CHC, PCSDirector of Educational Strategies - Wisconsin Medical Societypenny.osmon@wismed.orgCPT codes, descriptions and material only are Copyright 2010 American Medical Association. All Rights Reserved. No fee schedules, basicunits, relative values or related listings are included in applicable FARS/DFARS restrictions to government useObjectives Participants will learn appropriate billing guidelinesfor hospitalist services Participants will become familiar with differentcoding scenarios specific to hospitalists Participants will be able to document their servicesand choose the correct level based on theirdocumentation Participants will identify areas of documentationthat have potential gaps1
Common Codes For Hospitalistsp(9999 3) Initial HospitalCare (99221‐99223) Subsequent Hospital Care (99231‐99233) Observation/Inpatient Care (99234‐99236) Initial and Subsequent Observation &Discharge99224‐99226,99217)g (99218‐99220,(9999994 9999 7) Hospital Discharge (99238, 99239) Critical Care (99291, 99292)Initial Hospital Care99221-992232
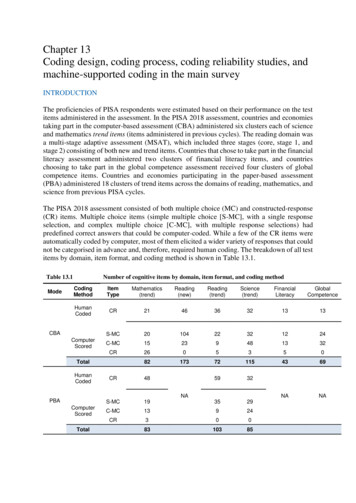
Initial Hospital Care99221Level IHistory Detailed HPI 4 ROS 2-9 PFSH (2 of 3)99222Level IIComp HPI 4 ROS 10-14 PFSH (3 of 3)99223Level IIIComp HPI 4 ROS 10-14 PFSH (3 of 3)ExamDetailedComprehensive eTypically30 minTypically50 minTypically70 minInitial Hospital Care CPT Codes 99221‐992239999 3 Documentation must meet 3 of 3 key elements Physician order must be for inpatient Service can be split/shared Both providers must personally document thecomponents personally performed Both providers billing a split/shared visit must beemployed by the same group3
Hospital Admits Initial Hospital Caret a hospitalosp ta caou d be bed o Initialcaree codes sshouldbilledon ttheedate the face‐to‐face service actually occurs(Principles of CPT Coding) If physician admits from a different site of service, allother services provided are considered part of theadmission (CPT 2011) Medicare patients: Multiple initial hospital carecodes can be billed be for the same encounter bymultiple providers for the same patientInitial Hospital Modifier“MedicareMedicare OnlyOnly”AI – Principal Physician of Record Informational modifier Used by “admitting” physician on initial hospital carecodes4
HistoryReview of Definitions HPI: History of Present Illness (Chief Complaint Required) LiDiQli Si TiiCModifying Factors, Associated Signs & Symptoms ROS: Review of Systems Constitutional, Eyes, ENMT, Cardio, Resp, GI, GU, MS,Integumentary, Neuro, Psych, Endocrine, Heme/Lymph,Allergic/Immunologic PFSH: Past Medical, Family and Social History Medical: Current meds, Allergies, Illnesses/Injuries, etc Family: negative or noncontributory Social: Marital status, Tobacco/Alcohol, Education,Employment, etcROS Example Review of systems: A 10‐point review of systems isotherwise negative.negative No fever or chills.chills No chest pain.pain Noother complaints. If a complete ROS was medically necessary to beperformed and a complete 14 organ system was reviewed,more appropriate verbiage would be:ROS: No chest pain, fever or chills, all other systemsreviewed and were negative5
Historyy DG: If the pphysicianis unable to obtain a historyyfrom the patient or other source, the recordshould describe the patient’s condition or othercircumstance which precludes obtaining a history History can be obtained from: Family members/friends Chart Nursing or other staffFamily HistoryFamily history: noncontributory Frequently seen with elderly patients. Code 99222 and 99223 require family history Non‐contributory family history notdocumented Preferred verbiage Family history: negative for heart disease6
Exam “Tips” Neck supple No neck lymphadenopathy Extremities are body parts and several different organsystems could be examined, specify what was examined HEENT: acronym, need to specify 95 DG Comprehensive – 8 organ systems 97 DG Comprehensive – 2 bullets in each of 9 body systems Look for other medically necessary systems Neuro, Psych, etc.Initial Hospital Care Unit/Floor time includes: Provider present in the hospital unit and/or at thebedside of the patient Reviewing the patient’s chart, Examining the patient, Writing notes/orders, Communicating with other professionals and thepatient’s family on the floor7
Split/Shared Care If the Initial Hospital Care service is split/sharedbetween two providers, both providers need topersonally document what components of service theyperformed It must be clear from the documentation that bothface‐to‐faceproviders had a faceto face encounter with the patientand personally performed at least one of the 3 keyelements, history, exam or medical decision‐makingSplit/Shared CareNon‐Qualifying Documentation “Patient seen” or “seen and examined” and signed by thephysician “Seen and examined and agree with above” (or “agree withplan”), signed by the physician “I have personally seen and examined the patientindependently, reviewed the PA's Hx, exam and MDM andagree with the assessment and plan as written” signed by thephysician8
Split/Shared CareNon‐Qualifying Documentation “As above” signed by the physician Documentation by the NPP stating “The patient wasseen and examined by myself and Dr. X., who agreeswith the plan” with a co‐sign of the note by Dr. X No comment at all by the physician, or only a physiciansignature at the end of the noteSplit/Shared Qualifying Examples Upon examination, wound appears to be pinking upwell, continue dressing changes as ordered. Agreewith NP’s history and plan. Mr. Jones lungs sound better today and he reportsless shortness of breath at night.night Reviewed and agreewith NP’s plan.9
Subsequent Hospital Care99231 - 99233Subsequent Hospital Care99231Level I99232Level II99233Level IIIHistory Prob Focused HPI: 1-3 ROS: n/a PFSH: n/aExp Prob Focused HPI: 1-3 ROS: 1 PFSH: n/aDetailed HPI 4 ROS 2-9 PFSH: n/aExamProb FocusedExp Prob imeTypically15 minTypically25 minTypically35 min10
Subsequent Hospital Care Requires 2 of the 3 key elements Only need ‘interval’ history It is not necessary to record information about the PFSH Need to document CC, pertinent HPI and ROS Assessment and plan should be documented for each service Codes are ‘per day’ If two or more providers from the same specialty perform amedically necessary visit, the accumulation of bothproviders’ work can only be billed under one of theproviders Service can be split/shared“Interval History”DG: A ROS and/or PFSH obtained during anearlier encounter does not need to be re‐recorded if there is evidence that the physicianreviewed and updated the previousinformation. The review and update may bedocumented by: Describing any new ROS and/or PFSH informationor noting there has been no change in theinformation; and Noting the date and location of the earlier ROSand/or PFSH11
Inpatient Consultations99251‐99255Inpatient Consults: Medicare UUse theh InitialI i i l HospitalH i l CareCcodesd 99221‐99223 If documentation doesn’t meet lowest level (99221)report the appropriate Subsequent Hospital Care code(99231‐99233)12
Consultations CPT Guideline ‐ Concurrent Care“Concurrent care is the provision of similarservices (eg, hospital visits) to the same patientby more than once physician on the same day.Wh concurrent care isi provided,id d no speciali lWhenreporting is required.”Concurrent Care in Global SurgeryThe Medicare physician fee schedule payment amountfor surgical procedures includes all services (e.g.,evaluation and management visits) that are part of theglobal surgery payment; therefore, contractors shallnot pay more than that amount when a bill isfragmented for staged procedures.IOM 100‐04, Chapter 12, 30.6.9.2 (A)13
Consultations CPT Guideline G id li“A consultation is a type of evaluation and managementservice provided by a physician at the request of anotherphysician or appropriate source to either recommendcare for a specific condition or problem or to determinewhether to accept responsibility for ongoing managementh patient’si ’ entirei care or ffor theh care off a specificifioff thecondition or problem.”Consultations CPT Guideline Written or verbal request MUST be made byphysician or appropriate source and . Documented in patient’s medical record by either Requesting physician or appropriate source; or The consulting physician14
Consultations CPT Guidance“Consultation codes should not be reported by thephysician who has agreed to accept transfer of carebefore an initial evaluation ” Consultation codes may be reported if thedecision to accept transfer of care cannot be madeuntil after the initial consultation evaluation,regardless of site of service.Consultations CPT Guidance If the receiving physician agrees to providemanagement for “some or all” of a patient’scondition prior to the initial evaluation, it is notappropriate for the receiving physician to report aconsultation code15
Observation ServicesCPT Codes for Observation Initial Observation Care 99218‐99220 Used when stay is less than 8 hours on the same calendar dayor the stay is greater than one calendar day Only billed by admitting physician Observation Discharge99 99217 Observation or Inpatient Hospital Care 99234‐99236 Used when stay is greater than 8 hours on the same calendarday16
Observation ServicesSame Calendar DayInpatient Care 8 hours99221-99223 Discharge code 8 hours99234-99236Provider mustsee twiceObservation Care 8 hours99218-99220 Discharge code 8 hours99234-99236Provider mustsee twiceTwo Calendar DaysObservation CareDay 1: 99218-99220Day 2: 99217Documentation Insufficient?If the documentation doesn’t meetthe lowest level of service, report99499Observation Documentation Dated and timed pphysician’syadmittingg ordersregarding the care the patient is to receive while inobservation Admit to “Observation” & reason Physician should document his/her physical presence Physician should document his/her provision ofobservation care17
Observation Documentation Provider should document the number ofhours the patient remained in theobservation care status Provider should personally document theadmission and discharge noteObservation Services If a patient is admitted to the hospital after receivinghospital observation care services on the same date,only the Initial Hospital Care Code (eg, 99222) isreported The initial hospital care code selected to report theservices related to both the observation care and initialhospitalhi l care shouldh ld includei l d allll off theh E/M servicesiprovided on that date by the attending physician18
Subsequent Observation Coding CPT codesd 99224‐992266 New for 2011 Place of service is outpatient (22) Medicare vs. CPT guidelines Billed ONLY by the admitting physician All other physicians bill 99201‐99215 as appropriate Commercial payers Seek guidanceGuidance on Admission Decisions MLN Matters SE 103737 1037.pdf The severity of the signs and symptoms exhibited by thepatient The medical predictability of something adverse happeningto theh patienti The need for diagnostic studies that appropriately areoutpatient services to assist with determination19
Observation Discharge 99217 Final examination of the patient Discussion of the hospital stay Instructions for continuing care Preparation of discharge records99238 - 9923920
Hospital Discharge Documentation Final examination 99238: 30 minutes 99239: 30 minutes Discussion of hospital stay and plan of careto patient and/or all relevant caretakers PreparationPti off didischargehrecords,dprescriptions and referral forms Must document total time spentperforming the above activitiesHospital Discharge DocumentationAccordingg to Medicare,, “There must bedocumentation supporting a face‐to‐faceencounter when billing a discharge serviceon the date of death. If the provider doesnot see the patient prior to the time ofdeath or make the pronouncement ofdeath face‐to‐face, no E/M service may bebilled for that date of service.”21
Hospital Discharge DocumentationAccording to the AMA CPTAssistant,CPT AssistantMarch 1998, if a patient dies in thehospital, and the physician is present topronounce the patient's death, completesthe death summary, and talks with thedd patient'si ' family,f il theh appropriateideceasedhospital discharge code 99238‐99239 canbe reportedAdditional Documentation Information ShouldSh ld bbe billbilledd on ththe actualt l dayd faceftot facefoccurs If more than 30 minutes spent on discharge services,time must be documented in the medical record tosupport billing the 99239 code If medically necessary, subsequent visits can beg day”ybilled on the “actual discharge Physician must be physically present to pronouncedeath22
Critical Care Services ‐ Adult99291, 99292Critical Care Services Definition: “A critical illness or injury acutely impairsone or more vital organ systems such that there is ahigh probability of imminent or life threateningdeterioration in the patient’s condition; and The physician must devote his/her full attention to thepatient and,and therefore,therefore cannot provide services to anyother patient during the same time period” (CPT 2011)23
Critical Care Services Critical care services do not have to be provided in acritical care unit Seeing a patient in the critical care unit does notautomatically constitute critical care Only one physician can bill for any one minute ofi i l care providedid dcriticalReporting and Documenting Time The critical care time you bill can include only the timeth t iis dthatdevotedt d solelyl l tot one patientti t Time does not need to be continuous Time spent in the following activities can count towardthe critical care time: Time spent at the bedside with the patient Time spent on activities that contribute to the patientpatient’ss care,caresuch as reviewing old records and lab and imaging results,and consulting with other physicians Time spent with family, whether to obtain a history or todiscuss treatment options when a patient is unable toparticipate24
Critical Care InclusionsBelow are services included in Critical Care that cannot be billed separatelyTheseinclude:Thi l d Gastric intubation (43752, 43753) Interpretation of blood gases Interpretation of data stored in computers such as ECG’s, blood pressure, hematological data (99090)Interpretation of cardiac output (93561‐93562)Interpretation of chest x‐rays (71010‐71020)Pulse Oximetry (94760‐94762)Temporary transcutaneous pacing (92953)Vascular access procedures (36000, 36410, 36415, 36591,36600)Ventilator management (94002‐94004, 94660, 94662)Critical Care Services Cardiopulmonary resuscitation (CPR, code92950) is reported separately from critical careservices, and the time spent performing CPR isnot counted in total critical care time The time spent performing CPR is subtractedfrom the total critical care time Time spent performing separately reportableprocedures needs to be subtracted from thetotal critical care time25
Critical Care Documentation Example Pleasenote critical45 minutesbeyondPli i l care time:iibd allllbillable procedure spent entirely focused on thispatient’s care Critical care time began upon arrival at 1306 hours.Time out of the room was 2036 hours. Over thestay a total of 120 minutescourse of the patients ED stay,was spent in critical care delivery. This time does notinclude time spent performing other billable services.Documentation Do’s Additional key elements to include in documentation: Interventions taken to keep the patient fromimminent or life threatening deterioration The high complexity of decision‐making andthought processes that kept the patient from eitherdeteriorating or further deterioration Specifics of what was done to support vital systemg failure,, includinggfunctions or to address anyy organlabs, x‐rays and/or medical tests/procedures Time spent providing critical care services State “excludes” time spent performing separatelybillable services26
Billing Scenarioswww.cms.hhs.gov/manualsScenario 1Dr. Williams, a hospitalist, admits Mrs. Jones to thehospital from the ED at 11:30 am. He performs anddocuments an initial hospital care code of 99222. At11:30pm, Dr. Adams another hospitalist in the samegroup, (same specialty) sees Mrs. Jones and additionalmedical decision making occurs related to the admittingdiagnosis. Can Dr. Adams bill for his visit?27
Answer 1“If more than one evaluation and management (face‐to‐face)service is provided on the same day to the same patient bythe same physician or more than one physician in the samespecialty in the same group, only one evaluation andmanagement service may be reported unless the evaluationand management services are for unrelated problems.Instead of billing separately, the physicians should select alevel of service representative of the combined visits andsubmit the appropriate code for that level.Physicians in the same group practice who are in the samespecialty must bill and be paid as though they were a singlephysician.”IOM 100‐04, Chapter 12, Section 30.6.5Scenario 2An orthopedic surgeon admits a Medicare patientffromtheh ER andd planslsurgery ffor a hihip ffracture thehnext day. He requests that Dr. Smith, the internalmedicine hospitalist, see the Medicare patient onthe same day for chronic hypertension and pre‐operative clearance.How would this be billed?28
Answer 2The orthopedic surgeon will bill for the initial hospitalcare (99221–99223) and use modifier AI to indicate he isthe principal physician of record. The hospitalist willbill another initial hospital code (99221‐99223) based onwhat was performed and documented.Scenario 3Following the hip replacement surgery, theorthopedic surgeon requests the consultinghospitalist to manage the hypertension of thepatient during the surgical global period while thepatient remains in the hospital.What codes would the hospitalist report?29
Answer 3The hospitalist would need to report the appropriatesubsequent hospital codes for the services performedrelated to the hypertension.IOM 100‐04, Chapter 12, Section 30.6.10 (H)Scenario 4Hospitalist is called by the nurse at 6:45 am topronounce death. The hospitalist is face to facewith the patient and pronounces death. A dischargesummary is dictated.Is this billable?30
Answer 4Only the physician who personally performs thepronouncement of death shall bill for the face‐to‐faceHospital Discharge Day Management Service, CPT code99238 or 99239. The date of the pronouncement shallreflect the calendar date of service on the day it wasperformed even if the paperwork is delayed to adate.subsequentqIOM 100‐04, Chapter 12, Section 30.6.9.2 (E)Scenario 5Patient is admittedddbby generall surgeon forf electivelsurgery on Monday. The surgeon does not have a face toface visit with the patient in the hospital until Tuesdaymorning. Hospital protocol requires that a hospitalistround all patients on the day of admission. A hospitalistperforms a routine visit on the patient during eveningrounds.roundsWhat can the hospitalist bill?31
Answer 5The answer is nothing. Per CMS, if the hospitalist wascalledduell d to see theh patientid to medicaldi l necessityi (not(protocol), a subsequent visit would be payable.Scenario 6HospitalistHi li admitsd i patientiat 9am ddocumentingiand performing a 99222. The patient expires at3pm. The hospitalist is face to face with the patientand pronounces death. A dictated dischargesummary is performed.What can be billed by the hospitalist?32
Answer 6Carriers pay only the initial hospital care code when appg onpatient is admitted as an inpatientand dischargedthe same day. They do not pay the hospital dischargemanagement code on the date of admission. Carriersmust instruct physicians that they may not bill for bothan initial hospital care code and hospital dischargemanagement code on the same date.Chi 30.6.9.16(C)IOM 100‐04, Chapter12, SSectionScenario 7Hospitalist A sees the patient on 7/20 and completesthe discharge summary. Patient is scheduled fordischarge on 7/21 in the morning. Hospitalist Brounds prior to the discharge and sees the patientbriefly.What is billed?33
Answer 7The E/M discharge day management visit shall bereported for the date of the actual visit by the physicianor qualified nonphysician practitioner even if the patientis discharged from the facility on a different calendardate.IOM 100‐04, Chapter 12, 30.6.9.2 (B)7/20 – Bill Hospital Discharge7/21 – Potentially could bill subsequent visit Q&A34
DisclaimerThe information presented and responses to the questionsposed are not intended to serve as coding or legal advice.advice Manyvariables affect coding decisions and any response to the limitedinformation provided in a question is intended only to providegeneral information that might be considered in resolvingcoding issues. All coding must be considered on a case‐by‐casebasis and must be supported by appropriate documentation inthe medical record. Therefore, the Wisconsin Medical Societypayersrecommends consultingg directlyy with py to determinespecific payers’ guidance regarding appropriate coding andclaim submission. The CPT codes that are utilized in codingclaims are produced and copyrighted by the American MedicalAssociation (AMA). Specific questions regarding the use ofCPT codes may be directed to the AMA.35
2 Common Codes For Hospitalists Initial Hospital Care (99221 ‐9999 3)223) Subsequent Hospital Care (99231‐99233) Observation/Inpatient Care (99234‐99236) Initial and Subsequent Observation & Discharge (99218‐99220, 9999 4224‐99226, 9999 7)217) Hospital Discharge (99238, 99239) Critical Care (99291, 99292)