Transcription
FINAL PROGRAM AND ABSTRACT BOOK2nd Dietitians workshop on PKURome, Italy - March 22, 2012
General informationVenueThe workshop takes place at the:Rome Marriott Park HotelVia Colonnello Tommaso Masala, 5400148 Rome, ItalyLanguageThe official language of the workshop is English.Scientific secretariatSerono Symposia International FoundationSalita di San Nicola da Tolentino, 1/b00187 Rome, ItalyJunior Project Manager: Simona GaudiosiTel.: 39-06-420 413 308Fax: 39-06-420 413 677E-mail: simona.gaudiosi@seronosymposia.orgSerono Symposia International Foundationis a Swiss Foundation with headquarters in14, rue du Rhône, 1204 Geneva, SwitzerlandOrganizing secretariatMeridiano Congress InternationalVia Mentana, 2/B - 00185 Rome, ItalyCongress coordinator: Sara GuglielminiTel.: 39 (0)6 88595 211 - Fax: 39 (0)6 88595 234E-mail: s.guglielmini@meridiano.it1
2nd Dietitians workshop on PKUSerono Symposia International Foundation workshop on:2nd Dietitians workshop on PKURome, Italy - March 22, 2012Aim of the workshopDietary restriction of phenylalanine is the mainstay of treatment of phenylketonuria (PKU). Other treatment options (i.e. BH4) usedas an alternative treatment or in combination with diet therapy are also important. Aim of this workshop is to share practice, latestresearch and developments in the dietary management of PKU patients.Learning objectives Examine the management of PKU, particularly concerning issues of supplementation and assessment of nutritional status.Explore developments, latest research and progress surrounding diet therapy.Consider the many issues and challenges of dietary treatment and appraise different management strategies.Consider patient education and motivation.Target audienceDietitians and nutritionists and any health professional interested in the dietary and nutritional management of PKU.AccreditationSerono Symposia International Foundation (www.seronosymposia.org) is accredited by the European Accreditation Council forContinuing Medical Education (EACCME ) to provide the following CME activity for medical specialists. The EACCME is an institutionof the European Union of Medical Specialists (UEMS), www.uems.netThe conference “2nd Dietitians workshop on PKU” (March 22, 2012 - Rome, Italy) is designated for a maximum of 6 (six) hours ofEuropean CME credits (ECMEC). Each medical specialist should claim only those credits that he/she actually spent in theeducational activity. EACCME credits are recognized by the American Medical Association (AMA) towards the Physician'sRecognition Award (PRA). To convert EACCME credit to AMA PRA category 1 credit, please contact the AMA.Accreditamento ECM per partecipanti italianiSSIF SRL (Società Scientifica di Formazione Internazionale) provider Scientifico No. 13753 ha sottoposto, secondo la prassi indicatadal Ministero della Salute, la richiesta di accreditamento del congresso “2nd Dietitians workshop on PKU” (23-24 marzo - Roma,Italia), n. riferimento provider 13753, n. riferimento evento 12000636 - Medico Chirurgo e n. riferimento 12000637 - Dietista, allaCommissione Nazionale per la Formazione Continua che provvederà a comunicare i crediti formativi concessi per l’evento.All Serono Symposia International Foundation programs are organized solely to promote the exchange and dissemination of scientific and medical information. No formsof promotional activities are permitted. There may be presentations discussing investigational uses of various products. These views are the responsibility of the namedspeakers, and do not represent an endorsement or recommendation on the part of Serono Symposia International Foundation. This program is made possible thanks tothe unrestricted Educational grants received from: Centre d’Esclerosi Multiple de Catalunya, ComtecMed, Congrex Sweden, Congrex Switzerland, Cryo-Save, Datanalysis,Esaote, European Society of Endocrinology, Fondazione Humanitas, Fundación IVI, ISFP International Society for Fertility Preservation, ISMH International Society of Men’sHealth, K.I.T.E., Merck Serono, Sanofi-Aventis, University of Catania, Vall d'Hebron University Hospital.2
Learning effectiveness projectThe world of CME is changing with many different live and online formats, and Serono Symposia International Foundation(SSIF) is continually trying to improve its CME activities.With your participation in a structured series of evaluations, SSIF can provide cutting-edge learning activities designed to giveyou the greatest value from the time you invest.SSIF is running the learning effectiveness project for this meeting.You will be involved in three main steps: During the conference: you will be asked to complete a questionnaire at the beginning and at the end of the workshop toassess the program in various domains. Post-event: three weeks after the event we will email you a short questionnaire which will give you the opportunity to tellus how much of what you learned has had an affect on your know-how and daily practice. Follow-up: three-months after the event, we will contact you with the final questionnaire.We will collate and analyse your responses and use the results to improve and develop our ongoing programs.Of course, we commit to maintaining the confidentiality of the information you provide and we will inform you about the resultsof the process regarding the activity that you attended.Thank you very much for participating in this project!follow us onPKU Academyhttp://twitter.com/PKU Academy3
Scientific organizerAnita MacDonaldDietetic DepartmentThe Children’s HospitalBirmingham, UKScientific committeeKristina MotzfeldtDepartment of PediatricsWomen and Children’s divisionSection for specialized medicineand unit for newborn screeningOslo University Hospital,RikshospitaleKirsten AhringPKU DepartmentThe Kennedy CentreBagsvaerd, DenmarkAmaya Bélanger-QuintanaUnidad de EnfermedadesMetabólicasServicio de PediatríaHospital Ramon y CajalMadrid, SpainMartine RobertHôpital Universitaire des EnfantsReine-FabiolaBrussels, BelgiumKatharina DokoupilDepartment of Metabolismand NutritionDr. von Hauner Children's HospitalUniversity of MunichMunich, GermanyJúlio César RochaCentro de Genética MédicaJacinto de MagalhãesInstituto Nacional de SaúdePorto, PortugalMargreet van RijnSection of Metabolic DiseasesBeatrix Children's HospitalUniversity Medical Center GroningenGroningen, NetherlandsHulya Gokmen-OzelFaculty of Health SciencesDepartment of Nutritionand DieteticsHacettepe UniversityAnkara, TurkeyAnna Maria LammardoDepartment of PediatricsSan Paolo HospitalUniversity of MilanMilan, ItalyAnita MacDonaldDietetic DepartmentThe Children’s HospitalBirmingham, UK4
List of speakers and chairmenKirsten AhringPKU DepartmentThe Kennedy CentreBagsvaerd, DenmarkAnita MacDonaldDietetic DepartmentThe Children’s HospitalBirmingham, UKAmaya Bélanger-QuintanaUnidad de enfermedades metabolicasServicio de PediatriaHospital Ramon y CajalMadrid, SpainKristina MotzfeldtDepartment of PediatricsWomen and Children’s divisionSection for specialized medicineand unit for newborn screeningOslo University Hospital, RikshospitaletOslo, NorwayLaurie BernsteinInherited Metabolic Diseases (IMD) clinicThe Anschutz Medical CampusUniversity of ColoradoAurora, USAJúlio César RochaCentro de Genética MédicaJacinto de MagalhãesInstituto Nacional de SaúdePorto, PortugalAnnet M. BoschDepartment of PediatricsAcademic Medical Center (AMC) AmsterdamAmsterdam, NetherlandsFriedrich K. TrefzMedical Centre GammertingenKreiskliniken Reutlingen GmbHGammertingen, GermanyKatharina DokoupilDepartment of Metabolism and NutritionDr. von Hauner Children's HospitalUniversity of MunichMunich, GermanyMargreet van RijnSection of Metabolic DiseasesBeatrix Children's HospitalUniversity Medical Center GroningenGroningen, NetherlandsFrançois FeilletCentre de Référence desMaladies Héréditaires du MétabolismeHôpital d’Enfants, CHU BraboisVandoeuvre les Nancy, FranceEleanor WeetchNutrition and DieteticsNational Society for Phenylketonuria UKand Adult Metabolic DietitianNorthern General Hospital, SheffieldBarnsley, South Yorkshire, UKHulya Gokmen-OzelFaculty of Health SciencesDepartment of Nutrition and DieteticsHacettepe UniversityAnkara, TurkeyShauna KearneyDepartment of PsychologyThe Children’s HospitalBirmingham, UKAnna Maria LammardoDepartment of PediatricsSan Paolo HospitalUniversity of MilanMilan, Italy5
Scientific ProgramThursday - March 22, 201208.40 Welcome and introductionAnita MacDonald (UK)Session ISession IIIMicronutrient status and PKUChairs: Kirsten Ahring (Denmark)Chairs: Anna Maria Lammardo (Italy)Parallel workshops11.50 Parallel workshops1. Education and motivation of patients: whatworks in PKU?Laurie Bernstein (USA)09.00 L1: Micronutrient intake vs nutritionalbiochemistry: does it all add up?2. Maternal PKUEleanor Weetch (UK)Kristina Motzfeldt (Norway)Speaker 1: François Feillet (France) on vitaminsSpeaker 2: Anita MacDonald (UK) on minerals3. Assessing nutritional statusJúlio César Rocha (Portugal)Hulya Gokmen-Ozel (Turkey)09.50 Roundtable discussion: should we routinelymeasure micronutrient markers in all patients withPKU?Led by: François Feillet (France)Led by: Anita MacDonald (UK)Led by: Júlio César Rocha (Portugal)4. Introducing Sapropterin with dietMargreet van Rijn (Netherlands)Amaya Bélanger-Quintana (Spain)12.40 Lunch and rotation of workshop10.10 Coffee Break13.40 Parallel workshopsSession IIOral presentations1. Education and motivation of patients: whatworks in PKU?Laurie Bernstein (USA)Chairs: Kristina Motzfeldt (Norway) - Eleanor Weetch (UK)10.40 Oral presentations: 4 original contributions2. Maternal PKUEleanor Weetch (UK)Kristina Motzfeldt (Norway)OP1: Case Study of R.P.: Managing Levels inToddlers with Diet and SapropterinNicole Pallone (Canada)3. Assessing nutritional statusJúlio César Rocha (Portugal)Hulya Gokmen-Ozel (Turkey)OP2: SMS text message reminder service forPhenylketonuria patients to monitorphenylalanine concentrationsSara Boocock (UK)4. Introducing Sapropterin with dietMargreet van Rijn (Netherlands)Amaya Bélanger-Quintana (Spain)OP3: Trace Element Status in Adult Patients withPhenylketonuriaSara Boocock (UK)OP4: A model of comprehension of low Phe diet ina family with PKU childNatalia Usurelu (Republic of Moldova)6
Session IV Case studiesSession V14.30 Case studies in PKUChairs: Anita MacDonald (UK)Chairs: Amaya Bélanger-Quintana (Spain)CS1: Dosage of Sapropterin in overweight patientsKatharina Dokoupil (Germany)Quality of lifeCS2: Managing illness with diet and SapropterinHulya Gokman-Ozel (Turkey)16.10 L2: Quality of Life vs. strict dietary control? Is oneat the cost of the other?Annet M. Bosch (Netherlands)CS3: Managing pregnancy with SapropterinFriedrich K. Trefz (Germany)Session VI Workshops round upCS4: Managing a second diagnosis withSapropterinKirsten Ahring (Denmark)16.50 Workshops round up17.50 Final conclusionsAnita MacDonald (UK)Comment by expert panel: psychologist, dietitian,physicianAmaya Bélanger-Quintana (Spain)Margreet van Rijn (Netherlands)Shauna Kearney (UK)18.00 End of the Workshop15.40 Tea break7
Disclosure of faculty relationshipsSerono Symposia International Foundation adheres to guidelines of the European Accreditation Council for Continuing MedicalEducation (EACCME) and all other professional organizations, as applicable, which state that programs awarding continuingeducation credits must be balanced, independent, objective, and scientifically rigorous. Investigative and other uses forpharmaceutical agents, medical devices, and other products (other than those uses indicated in approved product labeling/packageinsert for the product) may be presented in the program (which may reflect clinical experience, the professional literature or otherclinical sources known to the presenter). We ask all presenters to provide participants with information about relationships withpharmaceutical or medical equipment companies that may have relevance to their lectures. This policy is not intended to excludefaculty who have relationships with such companies; it is only intended to inform participants of any potential conflicts soparticipants may form their own judgments, based on full disclosure of the facts. Further, all opinions and recommendationspresented during the program and all program-related materials neither imply an endorsement, nor a recommendation, on the partof Serono Symposia International Foundation. All presentations solely represent the independent views of the presenters/authors.The following faculty provided information regarding significant commercial relationships and/or discussions of investigational ornon-EMEA/FDA approved (off-label) uses of drugs:Kirsten AhringDeclared no potential conflict of interestAmaya Bélanger-QuintanaDeclared to be member of: Merk Serono PKU European Scientific Advisory board, Europeannutritionist expert panel and Kamper advisory board.Laurie BernsteinDeclared receipt of grants and contracts from Biomarin and Nutricia. Declared receipt of honorariaor consultation fees by Applied Nutrition and Nutricia.Sarah BoocockDeclared no potential conflict of interest.Annet M. BoschDeclared receipt research grant by Danone. Declared to be member of a company advisory board:Merk Serono and Danone.Katharina DukoupilDeclared receipt of grants and contract from Merck Serono. Declared receipt of honoraria orconsultation fees by Merck Serono.François FeilletDeclared receipt of honoraria or consultation fees by Geuggue, Biomarin, Merk Serono and Nutricia.Declared to be member of Merck Serono and Nutricia advisory boards.Hulya Gokmen-OzelDeclared receipt of honoraria or consultation fees by: Merck Serono.Shauna KearneyDeclared no potential conflict of interest.Anna Maria LammardoDeclared no potential conflict of interest.Anita MacDonaldDeclared receipt research grants from Nutricia, Vitaflo, Cambrooke Foods and Merck Serono.Declared to receipt of honoraria or consultation fees by Merck Serono and Nutricia.Kristina MotzfeldtDeclared to be member of European Nutritional Expert Panel in PKU Merck Serono. Declaredparticipation in a company sponsored speaker’s bureau sponsored by SHS International.Nicole PalloneDeclared receipt of grants and contract from Biomarin and declared to be member of CanadianPKU and allied disorders Inc.Júlio César RochaDeclared receipt of honoraria or consultation fees by Merck Serono. Declared to be member of theEuropean Nutritionist Expert Panel on PKU – Merck Serono.Friedrich K. TrefzDeclared receipt of honoraria or consultation fees by Merck Serono.Declared to be member of EPG and KAMPER advisory boards.Natalia UsureluDeclared receipt of grants and contracts from Association of Rehabilitation of Children with PKU,Association ”ACASA”, CORDAID and Janivo Foundations.Margreet van RijnDeclared receipt of grants and contracts from Nutricia. Declared receipt of honoraria or consultationfees by Nutricia and Merck Serono.Eleanor WeetchDeclared no potential conflict of interest.8
Abstracts
L1 - “Micronutrient intake vs nutritional biochemistry:does it all add up?” -- Focused on vitaminsFrançois FeilletCentre de Référence des Maladies Héréditaires du Métabolisme, Hôpital d’Enfants, CHU Brabois, Vandoeuvre les Nancy, FranceVitamins intake and nutritional status in PKUIntroductionThe nutritional vitamin status results of the vitamin intake and the bioavailability of the vitamin in relation with the dietary referenceintake for age. As animal proteins act as the principal vectors for many micronutrients, there is a risk for vitamins deficiencies inpatients with a low-protein diet. On another hand, the vitamins supplementation of amino acids mixtures used in inborn error ofmetabolism can exceed the daily requirement because sometimes, this supplementation did not take into account the vitamin intakecoming from the natural proteins. Moreover, some patients can use more than one AA mixture every day, which makes thecalculation of the nutritional intake more and more complex.The multiplication of the amino acids mixturesDuring the last 30 years, the number and the quality of the AA mixtures increased constantly. The macronutrients composition ofthese mixture differ importantly from one AA mixture to another. For example, some very concentrated AA mixture do not containany fat in their composition, but they still have the same content of vitamins A, D and E which are fat soluble vitamins. The absorptionand the bioavailability of such vitamins in a no-fat substitute must be decrease compared with those which would be observed witha fat containing substitute. Today the vitamins composition of the AA mixtures is mainly calculated from the daily recommendedintake or from the legal content of micronutrient for medical food which is determined per 100 Kcal (which is a nonsense for the lowcaloric AA mixtures). This shows that the simple evaluation of the vitamin content of the AA mixture is not sufficient to really estimateits nutritional efficiency of the patients.The necessity of a yearly nutritional follow-upConsecutively, there is a real need for a yearly nutritional follow-up of these micronutrients to assess the real nutritional status ofour patients.The assessment of the vitamins nutritional status can be based on the recognition of the (rare) clinical signs of deficiencies of thesemicronutrients and/or on the biological measurement of these vitamins. Excesses in vitamin status are usually determined on thebiological assessment. Most often, this biological assessment is based on the analysis of the plasmatic values of vitamins but theseparameters are not always reliable with the real vitamin status. As an example, retinol status must be calculated in conjugation ofplasma RBP and the α-tocopherol status mainly reflects the plasma triglycerides levels. For some other vitamins as thiamin andriboflavin, the single plasmatic value only reflect the recent intake but not the chronic nutritional status of this vitamin. For someother the analysis of some secondary metabolites (pyridoxal phosphate for B6 or methylmalonic acid for B12) are more reliable todetect a vitamin deficiency but their analysis are less available and more expensive than the simple plasmatic dosage of the vitamin.Despite all these imperfections, the vitamins plasmatic analysis are often the only assessment performed in PKU patients.The cost of the analysisThese analysis are often very costly, and are not always reimbursed by insurances or national social security. Then all vitamins (andminerals) should not be performed in all patients every year. The vitamins without any safe upper levels or which have never beenshown to be deficient in PKU should be skipped of this nutritional follow up (thiamine, riboflavin, pyridoxin, biotin for example). Someothers must be systematically checked as cobalamin, which has been found deficient in many PKU patients, mainly those who areon a vegan like diet and who do not take any (or not enough) vitamins supplements.Who must beneficiate of the nutritional follow up?All patients must have a minimal nutritional assessment every year but some patients have an increase risk of nutritional deficiency,mainly due to the deficiency of animal protein in their diet.For example PKU patients are at risk of developing micronutrient deficiency if:- They fail to adhere to their phe-free amino acids (AA) mixtures (which contain the vitamins supplements).- They have mild hyperphenylalaninemia, treated with a low protein diet (containing mainly vegetable proteins without amino acidsmixture)- They are with BH4 and managed to stop their amino acids mixtures in combination with a low-protein diet mainly composed ofvegetable proteins.10
Folates, an example of vitamin in excess?The risk of excess which can be deleterious can exist for some vitamins. Most of the AA mixture contain more or less the total dailyrequirement intake for vitamins and minerals. As an example, the folates content of these mixtures goes from 25 μg/10 g of AA to133 μg/10g of AA. But, as these patients can eat vegetables which have a high content in folates (beans, spinach, asparagus, salad,cereals), the recommended daily intake is often surpassed. If the beneficial effect of folates supplementation has been demonstratedin many situation (Neural tube defects prevention for example) we must also keep in mind that the excess of folates has beenincriminated in facilitating colon cancer. An improvement in the folates composition of some AA mixture could be done to avoid theseexcesses which have no interest and which could be deleterious.ConclusionThe assessment of the vitamins status in patients treated by a low protein diet is very important. A complete screening must be donein some centers to improve the composition of the amino acids mixtures in the future. For the vast majority of patients, the onlyfollow up of the vitamins which can be deficient seems sufficient for the follow up of the patients and less costly for the society.11
L1 - “Micronutrient intake vs nutritional biochemistry:does it all add up?” -- Focused on mineralsAnita MacDonaldDietetic Department, The Children’s Hospital, Birmingham, UKMicronutrients in PKU: trace mineralsIn PKU optimal nutrient status is challenging when a substantial proportion of nutrient intake is from non-natural sources. Whennutrients are from artificial sources, defining the optimal intake of each nutrient and estimating their bioavailability is particularlytaxing. Results of studies are difficult to interpret when different biomarkers of nutrient status are tested, varying reference targetranges based on dissimilar diets and populations are used, and adherence to diet and protein substitute is commonly undefined.Relatively little is reported about trace mineral status using protein substitutes based on natural protein sources such asglycomacropeptide, the biochemical and clinical impact of any change in micronutrient composition of protein substitutes thatmanufacturers have made over the years and micronutrient status of different age groups. Three trace minerals/ minerals will bediscussed.Zinc: protein substitute supplemented with micronutrients is the major source of zinc intake in a low phenylalanine diet. Despitegenerous supplementation in protein substitutes, zinc deficiency is still described. Plasma zinc was low in 25% of 468 samples in a73 patients aged 1 to 17 years of age (MacDonald et al. 2011). Patients were mainly compliant with diet therapy. In PKU, the majorsource of zinc is added to the phenylalanine-free protein substitute; and it is probable that its bioavailability of zinc is sub-optimal.The bioavailability of zinc is affected by the copper, calcium and iron content of the diet, all of which compete for absorption. Reliablevalidated measures of zinc status are unavailable. Plasma or serum zinc is the most commonly used markers but do not necessarilyreflect cellular zinc status.Selenium: In humans, selenium is an essential component of antioxidant enzymes such as glutathionine peroxidase a trace elementthat functions as cofactor to protect membranes and essential proteins from potentially damaging effects of reactive oxygen andlipid peroxides. The content of selenium in foods depends upon the selenium content of the soil where plants or animals are raised.In the earlier years of dietary management, biochemical selenium deficiency was commonly reported mainly because proteinsubstitutes were not supplemented with selenium. The only reported clinical symptom of selenium deficiency in PKU is a dysrythmicventricular tachycardia in a 9-month old infant (Greeves et al. 1990). Long term BH4 therapy has been associated with improved longterm selenium status in PKU patients. Selenium is measured in plasma, serum, and red cells and by estimating tissue glutathionineperoxidase activity.Iron: Studies either demonstrate no deficiency or poor status. In iron deficient patients, no correlation has been demonstratedbetween iron intake and any index of iron status.Assessing vitamin and mineral status: Many factors affect blood sample analysis and its interpretation including blood samplequality, sample storage, and interlaboratory variation, and lack of age specific reference ranges. In addition diurnal variation, fastingstatus, acute infections, inflammatory stress may alter results observed.References:1. Greeves LG, Carson DJ, Craig BG, McMaster D Potentially life-threatening cardiac dysrhythmia in a child with selenium deficiency and phenylketonuria. ActaPaediatr Scand, 1990, 79 (1990): 1259-62.2. MacDonald A, Lee P, Davies P, Daly A, Lilburn M, Gokmen Ozel H, Preece MA, Hendriksz C, Chakrapani A. Long-term compliance with a novel vitamin andmineral supplement in older people with PKU. J Inherit Metab Dis. 31 2008: 718-23. Epub 2008 Oct 22.12
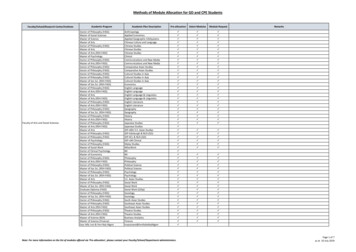
CS1 - Dosage of Sapropterin in overweight patientsKatharina DokoupilDepartment of Metabolism and Nutrition, Dr. von Hauner Children's Hospital, University of Munich, Munich, GermanyThis is a case report about a male patient with PKU, 36 years old. His body weight is 127 kg and his height 185 cm resulting in a bodymass index (BMI) of 37 kg/m². He is married and has two healthy children. Currently he works as a male nurse.For PKU treatment the patient followed a vegetarian diet with no Amino Acid Supplements and a calculated mean daily Phe-intakeof 2500 mg. At this, his blood Phe-levels ranged between 8.2- 11.5 (mean 9.6 mg/dl). Because he complained about increasingconcentration disabilities, Sapropterin was considered as a treatment option. Molecular genetic analysis revealed an unclear BH4responsive Genotype (N167I/ G272X). However, previous testing for BH4-responsiveness resulted in a Phe-reduction of 30 %.Hence, treatment with Sapropterin was tried starting with concentrations of 4.7 mg/kg up to 7 mg/kg.Table: Phe-levels (from daily collected blood samples) before and under Sapropterin (Phe-intake: 2500 mg/d)Blood Phe level(mg/dl)Blood Phe level(μmol/l)mean9.6577.3range8.2 - 11.5492-690mean6,6396,9range5.1 - 9.0306 - 540mean4.8290.1range2.9 - 6.6174 - 396Pre Phase(15.07. - 02.08.2010)Beginning with Sapropterin 600 mg/d (4,7 mg/kg)(07.08. - 23.08.2010)Increased dose of Sapropterin 900 mg/d (7 mg/kg)(25.08. - 12.10.2010)ConclusionsThe patient benefits from Sapropterin therapy: A dosage of 7 mg/kg body weight resulted in a relevant (50%) and significant (P 0.001) decrease of blood-Phe levels, and a better neurological outcome without eating a strict low Phe diet. There is no need for AAsupplements and for special low protein food. As consequence of this, outside eating remains easy and comfortable.Sapropterin dosage is not easy to establish in obese patients with PKU. We suggest to start with a lower dose and then to adapt itstep by step according to the patient's individual needs.13
CS2 - Managing illness with diet and SapropterinHulya Gokman-OzelFaculty of Health Sciences, Department of Nutrition and Dietetics, Hacettepe University, Ankara, TurkeyThis case report was aimed to show the effect of BH4 on blood phenylalanine (Phe) level in illness. BS is a 5 years and 2 months oldgirl living in Turkey. There is no consanguinity between parents. She was 2 months old when she was diagnosed with the newbornscreening. Her blood Phe level was 26.6 mg/dL. There was no mutation analysis.BH4 was given 20 mg/kg/day and blood phe level decreased from 32.92 mg/dl to 16.04 mg/dl at the 48th hour of the test (48%). Shewas BH4 responsive. Daily phe intake was increased 10 mg/kg on a weekly basis after BH4 treatment started and blood phe checkedevery week. Drug was administrated once a day in the morning before breakfast. There was no any concurrent medication.Her daily Phe intake was 20 mg/kg, daily total protein intake was 1.5 g/kg and daily protein intake from protein substitute was 15.1g. She was on low protein foods, vegetables and fruits and did not use normal bread, rice, pasta and animal foods before BH4treatment. Her energy intake was around 1300 kcal/day. Her daily Phe intake increased 3 fold to 65 mg/kg with BH4. She was on100 ml milk or yoghurt, 1/2 egg, 25 g meat, normal bread, rice, pasta, fruits and vegetables after BH4 treatment. Her median bloodphe level was 5.39 mg/dL (2.99 to 14.5 mg/dL) when she was on BH4. During the first 11 week of the treatment all blood phe levelswere within normal ranges (median 4.75 mg/dL). From 12nd week of the treatment blood phe increased to median 7.59 mg/dL.Since she had frequent fewer, urinary tract infection and her blood Phe level increased to between 12 and 14 mg/dL for several times,BH4 was stopped. She was not on free diet and needed 7 g protein from protein substitute before BH4 was stopped.Her weight-for-age Z-scores (WAZ), height-for-age Z-score (HAZ) and weight-for-height Z-score (WHZ) were 0.35, -0.54 and 1.03respectively before BH4 treatment. Her WAZ and WHZ scores increased to 0.59 and 1.32 respectively (p 0.05). HAZ score (-0.56) didnot change just before BH4 was stopped.Biochemical nutritional status, cognitive functioning, executive functioning, mood, quality of life was not measured when she was onBH4.References:1 - Chappel SC, Howles C 1991 Reevaluation of the roles of luteinizing hormone and follicle-stimulating hormone in the ovulatory process. Human Reproduction6 1206-1212.2 - Filicori M, Cognigni GE, Pocognoli P et al. 2003 Current concepts and novel applications of LH activity in ovarian stimulation. Trends in Endocrinology andMetabolism 14, 267-273.14
CS3 - Managing pregnancy with SapropterinFriedrich K. TrefzMedical Centre Gammertingen, Kreiskliniken Reutlingen GmbH, Gammertingen, GermanyEven evidence based recommendations for pre- and post conceptional phenylalanine (phe) restricted dietary treatment inphenylketonuria (PKU) pregnancies are widely accepted. However, overall treatment success for the MPKU offspring isunsatisfactory. Clinical experiences show tha
University of Colorado Aurora, USA Annet M. Bosch Department of Pediatrics . Department of Nutrition and Dietetics Hacettepe University Ankara, Turkey Shauna Kearney Department of Psychology The Children's Hospital . Northern General Hospital, Sheffield Barnsley, South Yorkshire, UK.