Transcription
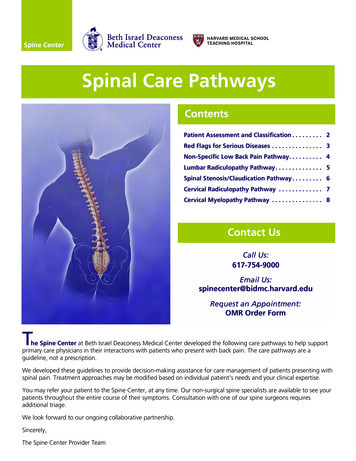
Spinal Care PathwaysContentsPatient Assessment and Classification . . . . . . . . . 2Red Flags for Serious Diseases . . . . . . . . . . . . . . . 3Non-Specific Low Back Pain Pathway. . . . . . . . . . 4Lumbar Radiculopathy Pathway. . . . . . . . . . . . . . 5Spinal Stenosis/Claudication Pathway . . . . . . . . . 6Cervical Radiculopathy Pathway . . . . . . . . . . . . . 7Cervical Myelopathy Pathway . . . . . . . . . . . . . . . 8Contact UsCall Us:617-754-9000Email Us:spinecenter@bidmc.harvard.eduRequest an Appointment:OMR Order FormThe Spine Center at Beth Israel Deaconess Medical Center developed the following care pathways to help supportprimary care physicians in their interactions with patients who present with back pain. The care pathways are aguideline, not a prescription.We developed these guidelines to provide decision-making assistance for care management of patients presenting withspinal pain. Treatment approaches may be modified based on individual patient’s needs and your clinical expertise.You may refer your patient to the Spine Center, at any time. Our non-surgical spine specialists are available to see yourpatients throughout the entire course of their symptoms. Consultation with one of our spine surgeons requiresadditional triage.We look forward to our ongoing collaborative partnership.Sincerely,The Spine Center Provider Team
Clinical Decision MakingSTEP 1: Assess your patient (diagnostic triage)Conduct a focused history and physical examination evaluating:Duration,severity andlocation ofpain/symptomsHistory ofinjury, previousback pain orsurgeryRisk factors forpotentiallyseriousconditionsPresence andseverity ofneurologicdeficitsExacerbatingand relievingfactorsInfluence of pain andtreatment on ability toperform activities ofdaily living, mood,ability to sleep andaddictive behaviorPsychosocialrisk factors Depression IPVOther riskfactors Smoking BMIPresence of Red Flags AlgorithmSee page 3ClassifyNon-SpecificLow BackPain(NSLBP)See page 4LumbarRadiculopathySpinal MyelopathyUnilateral legpain belowthe knee(with/withoutnumbness andweakness)Back painassociated withintermittent leg painthat is aggravatedby standing orwalking andrelieved by sittingNeck andradiating armpain/numbness,oftenaccompanied bymotor or sensorydisturbancesUnsteadiness ofgait, weakness,numb/clumsyfingersSee page 5See page 6See page 7See page 8Throughout this booklet you will see the following icons to help guide you in your clinical decision making.Refer toPhysical TherapyConsiderImaging-2-Consult withSpine Center
Presence Of Red Flags AlgorithmRed Flags for Serious DiseasesPresence of Red FlagsFRACTURECANCERINFECTIONTraumatic injury/onsetcumulative traumaSteroid use historySaddle anesthesia(numbness in theperineum)New onset urinaryretentionNew onsetbowel/bladderincontinenceProgressive weakness(sudden difficulty withambulating or inabilityto ambulate)Men age 50Red flags for seriousdiseases (refer to table)Cancer historyWomen age 50Male with diffuseosteoporosis orcompression fractureDiabetes mellitusInsidious onsetNo relief at bedtime orworsens when supineConstitutional symptoms(e.g. fever, weight loss)Go toEmergency DepartmentFurther evaluation by PCPor consult with Spine CenterHistory UTI/otherinfectionIV drug useHIVImmune suppressionPrevious surgeryGI Risk Factors Assess risk factors for GI complications associated with NSAIDsHistory of GI bleeding, peptic ulcer, cardiovascular disease, Heliobacter pylori positiveHigh dose, chronic, or multiple NSAIDsConcomitant use of low-dose aspirin, anticoagulants, corticosteroids, or selective serotonin reuptake inhibitorsAge 60 yearsSevere rheumatoid arthritis disabilityIf no GI risk factors NSAID If also elevated cardiovascular risk (assume onlow-dose aspirin or otherantiplatelet medication) naproxen plus PPIIf any GI risk factor NSAID plus PPI, or Cyclo-oxygenase-2 (COX-2) selective inhibitor (similar action,cost may differ).However, if: NSAID not tolerated COX-2 Very high GI risk (e.g. prior GI bleed) if possible avoid NSAIDs/COX-2.If cannot avoid, then COX-2 plus PPI If also elevated cardiovascular risk (assume on low-dose aspirin or otherantiplatelet medication) if possible avoid NSAIDs/COX-2. If cannot avoid, thenassess patient to prioritize GI and cardiovascular risks. If primary concern is: Very high GI risk COX-2 plus PPI Very high cardiovascular risk naproxen plus PPI-3-
Patient presents withNon-Specific Low Back Pain (NSLBP)STEP 1: Patient AssessmentEducateSTEP 2Reassure patient on the favorable prognosis (see linked patient education material on bidmc.org/spinecenter)Advise patients to stay activeDiscourage bed restPromote self‐management (carry on with normal activities as much as possible)Discourage lumbar supportsAvoid the followinginvestigationsA. Diagnostic imagingRadiological imaging is notrecommended for acute NSLBPfor patients 50 years of agePlain radiographs are optionalfor patients 50 years of ageB. EMG is not recommended foracute NSLBPC. Laboratory testingNot recommended unlessspecific illness is suspectedESR, CBC if cancer or infectionis suspectedPrescribe medicationfor pain relief(if needed)Prescribe PhysicalTherapyNon‐narcotic analgesics‐ Acetaminophen‐ NSAIDs (refer to page 3,GI Risk Factors)4-6 weeks, then reassessFor patients whose pain is madeworse by physical activity orexercise (these patients may benefitfrom therapeutic exerciserecommendations)Active treatments havedemonstrated greater efficacythan passive therapiesMuscle relaxantsAvoid NarcoticsPrescribe integrated medicine:- Massage therapy- AccupunctureSTEP 3Follow-up Visit (4-6 weeks after initial visit)Reassess patient status 4-6 weeks after initial visitif symptoms fail to resolveExclude serious pathology (Red Flags)Review psychosocial risk factorsSTEP 4Patient remainssymptomaticPatient has shownimprovementKeep going: transition to homeexercise program (a few patientsmay still require sessions with thephysical therapist)Consider imagingX-rays, 4-6 weeksMRI w/o contrast, 12 weeksConsult with Spine Center-4-
Patient presents withLumbar RadiculopathyUnilateral leg pain below the knee (with/without numbness and weakness)STEP 1: Patient AssessmentAdditional AssessmentSTEP 2Conduct detailed neurological exam including motor, sensory testing, reflexIf there are any symptoms of urinary or bowel and bladder symptomatology (including urinary retention orincontinence) then a rectal exam needs to be done to exclude cauda equina syndromeConduct a supine Straight Leg Raise (SLR) /‐ forward flexion, hyperextension and slump tests to assessL4, L5, S1Conduct a Femoral Stretch Test (FST) to assess L1, L2, L3 nerve root irritabilityIdentify the type of pain and exacerbating factorsPerform a complete lower extremity physical examination to rule out a musculoskeletal cause of the painConsider serious medical causes of radiculopathy (e.g. demyelinating disease, vitamin B12 deficiency,syphilis, herpes, diabetes and others)EducateAdvise patient in theacute phase to avoidheavy lifting or aggravatingmovements, thoughstaying active is veryimportantPrescribe PhysicalTherapy4-6 weeks, then reassessPrescribe medicationfor pain relief(if needed)Neuropathic pain medicationtrial: Gabapentin, Pregabalin,Tramadol, etc. (short course)Avoid narcoticsSTEP 3If symptoms unresolvedConsider imagingSTEP 4MRI w/o contrastDepending on pain severityand time course, consultwith Spine CenterConsult withSpine Center-5-
Patient presents withSpinal Stenosis/ClaudicationBack pain associated with intermittent leg pain that is aggravated by standing or walking and relieved by sittingSTEP 1: Patient AssessmentClinical DiagnosisSTEP 2Diagnostic tests not routinely indicatedNo imaging studies if no Red FlagsRule out diagnoses; i.e. vascular claudicationMedical TreatmentEducationExercise to tolerance; avoid harm (pain/numbnessfollowing exercise that persists for hours)Medication (Avoid Narcotics)Physical Therapy 4 weeksNeeds improvementFirst Follow‐Up Visit(4‐6 weeks after initial visit)STEP 4STEP 3ImagingSpine radiography;MRI w/o contrastMRI DoesNot ShowCompressionNot a neurocompressivedisorderFurther work-up forneuropathy/other pathology/vascular claudicationMRI ShowsCompressionConsult withSpine Center-6-Improvement in pain and functionPhysical therapy withtransition to home programContinue what has helpedRegular follow‐up(every 6 months)
Patient presents withCervical RadiculopathyNeck and radiating arm pain/numbness, often accompanied by motor or sensory disturbancesSTEP 1: Patient AssessmentAdditional AssessmentConduct detailed neurological exam including motor, sensory testing, reflexIdentify the type of pain and exacerbating factorsPerform a complete upper extremity physical examination to rule out a musculoskeletal cause of the painConsider serious medical causes of radiculopathy (e.g. demyelinating disease, vitamin B12 deficiency,syphilis, herpes, diabetes and others)Weakness and/or Functional Decline?NoYesNon-progressive neurologic deficit or no neurologic deficitSTEP 2Prescribe medicationfor pain relief(if needed)Prescribe PhysicalTherapy4-6 weeks, then reassessNeuropathic pain medicationtrial: Gabapentin, Pregabalin,etc.Tramadol (short course)Avoid narcoticsSTEP 4STEP 3No improvementImagingSpine radiography; MRI w/o contrastConsult with Spine CenterDegree of urgency dependsupon progression ofsymptomsConsult with Spine Center-7-Depending on pain severityand time course, consultwith Spine Center(no imaging required)
Patient presents withCervical MyelopathyUnsteadiness of gait, weakness, numb/clumsy fingersSTEP 1: Patient AssessmentAdditional AssessmentConduct detailed neurological exam including motor, sensory testing, reflexIdentify the type of pain and exacerbating factorsPerform a complete lower extremity physical examination to rule out a musculoskeletal cause of the painConsider serious medical causes of radiculopathy (e.g. demyelinating disease, vitamin B12 deficiency,syphilis, herpes, diabetes and others)YesWeakness and/or Functional Decline?EducateSTEP 2NoPrescribe therapyAdvise against activities predisposing to fallsWarn re: symptoms to watch forPrescribe medication for pain reliefAcetominophenAnti-inflammatoryPhysical therapy for:‐ Gait training/balance training‐ Strength trainingOccupational therapy for:‐ Activities of daily livingNo improvementImagingSTEP 3Urgency depends upon severity and progression ofsymptoms. If concerned, consult with Spine Center.Cervical spine x-raysMRICT-myelogram if contraindication to MRISTEP 4MRI showssignificant spinal cord compression,that is, cord effacement, or intramedullary signal change, spinal corddeformity, severe stenosisConsult withSpine Center forcervical myelopathyMRI does not showspinal cord pathologyCervical myelopathyis not presentConsider other pathology (e.g.multiple sclerosis, brain pathology,amyotrophic lateral sclerosis, folateor B12 deficiency, peripheral neuropathy) and manage accordingly.Consider referral to neurology.-8-
Spinal Care Pathways T he Spine Center at Beth Israel Deaconess Medical Center developed the following care pathways to help support primary care physicians in their interactions with patients who present with back pain. The care pathways are a