Transcription
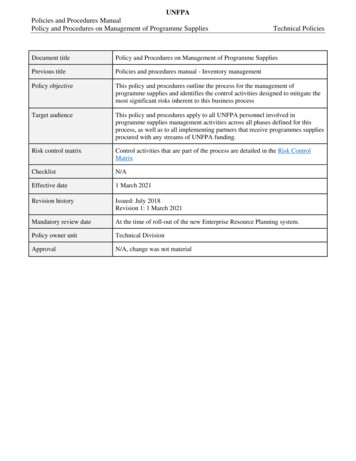
Policies, Procedures,Management GuidelinesPediatric Sickle Cell Disease ProgramUniversity of FloridaDepartment of PediatricsDivision of Pediatric Hematology/OncologyVishwas S Sakhalkar, MDMedical DirectorLevette Dunbar, MDPhysicianLynn Davidson, RNNurse CoordinatorSpecial thanks to Amos Kedar, MD who originally wrote the above guidelinesRevised: Jan 2009Note: These guidelines do not indicate an exclusive course of treatment or serve as a standardof care. Variations based on a physician's best medical judgment may be appropriate inindividual cases.11
TABLE OF CONTENTSPediatric Sickle Cell Program3Policies and Procedures5Management Guidelines for the Infant and Young Child11Management Protocol for Febrile Infants and Children16Antibiotic therapy in Patients With Known Allergies to Penicillin and/or Cephalosporin18What to do When Your Child has Fever (Handout)19Management of Acute Chest Syndrome20Outpatient Assessment and Management of Vaso-Occlusive Episodes22Inpatient Management of Severe Sickle Cell Vaso-Occlusive Episodes24Management Guidelines for Aplastic Crisis28Acute Splenic Sequestration30Management Guidelines for Priapism32Chronic RBC Transfusion Management Protocol34Iron chelation protocol35Exchange transfusion37Deferoxamine (Desferal) Infusion Orders40Peri-Operative Management41Dental Management of Children with Sickle Cell Disease43Leg Ulcers in Sickle Cell Disease45Hydroxyurea Information46Gallstones4812
Pediatric Sickle Cell ProgramThe information on the following pages has been designed to acquaint health care providers, viz.,physicians, physician assistants, nurses, fellows, residents, orstudents; with the functions andactivities of the Pediatric Sickle Cell Program at the University of Florida in Gainesville, Fl.PurposeThe Sickle Cell program is a component of the division of Pediatric Hematology/Oncology andis designed to provide consultation, comprehensive specialty medical care,psychosocial/financial support, and education/information to patients with sickle cell disease andtheir families.LocationThe Sickle Cell clinic is located at the Shands Medical Plaza on the second floor.AddressPediatric Specialty Clinic2000 SW Archer RoadGainesville, Florida 32610-0383Clinic DaysPatients with sickle cell disease are seen in the clinic on any scheduled clinic day but are mainlyseen on Mondays and Wednesdays.Primary CareThe sickle cell program does not provide primary care. All patients are encouraged to have aprimary care physician or neighborhood clinic to provide routine immunizations, offeranticipatory guidance, and be available to assist with the acute care of sickle cell relatedproblems.Program PersonnelVishwas S Sakhalkar, MDLevette Dunbar, MDLynn Davidson, RNMedical Director (352) 392-5633Physician (352) 392-5633Nurse Coordinator (352) 265-8250 ext 88239Hematology-Oncology AttendingsWilliam Slayton, MD, Interim Chief, Pediatric Hematology/OncologyAmy Smith, MD13
Hematology-Oncology Physician Assistants/ARNPJerry Janiec, PA-CWilliam K Higgins, PA-CStephanie Bryan, PA-CRachel Nettle, ARNPPamela Snyder, ARNPHillary Bess, ARNPAnn Robinson, PA-CHematology-Oncology FellowsAngela Rivers, MDPaul LoDuca, MDClinic NursesDonna McAffe, RNChristie Glenn, RNDax Balch, RNSocial WorkersSandra Powers, MSWChild Life SpecialistJenna PriestOther faculty physicians, fellows, and nurses as well as residents, medical students, nursingassistants, phlebotomist, and other consultants also participate in the management of sickle cellpatients as needed.Satellite ClinicsWe participate in several satellite clinics in the State of Florida that are sponsored by theChildren’s Medical Services (CMS). These clinics are held four times a year in Daytona Beach,and 10 times a year in Tallahassee. Staffs participating in these outpatient clinics are Dr.Vishwas Sakhalkar, Dr. Levette Dunbar and Ms. Lynn Davidson, physician assistants as well asCMS nurses. The staffs will usually service 20-25 patients (with non-acute issues) a clinic. Ifcomplex treatment is recommended, the patients are referred to Gainesville. Phone follow-upconsultations on these patients continue throughout the year. While most of these are patientscovered by CMS, a limited number of consultations of non-CMS patients take place by priorarrangements.Special thanks to Dr. Amos Kedar who originally wrote the above guidelines14
Policies and ProceduresI.Frequency of Outpatient Visits1.Initial Visit: Infants diagnosed by the Newborn Screening Program of Florida should beseen by the Pediatric Sickle Cell Program before 3 months of age. The purpose of theinitial clinic visit is to perform hematological studies, confirm the exact diagnosis,perform family studies, if desired, and to provide initial education and counseling to theparents. For newly diagnosed patients, a follow-up visit occurs one month later todiscuss the results of the confirmatory studies with the family, and to review issuesregarding prophylactic penicillin, spleen palpation, genetics, and routine healthmaintenance. Older patients with an established diagnosis of sickle cell disease are seenat 3 to 12 month intervals as appropriate for age.Follow-up Outpatient Visits At each routine visit a CBC and reticulocyte count shouldbe done to document steady state values (which may change during the first several yearsof life). A comprehensive metabolic panel may be done yearly on patients over 5 yearsof age. Oxygen saturation is measured at every visit in patients over 2 years of age, ifpossible. Routine visits usually occur at the following minimum intervals. Children areseen more often if clinically indicated. For children with a private pediatricianknowledgeable about sickle cell disease, the interval between follow up visits can bedoubled.Sickle Cell Anemia and Sickle Beta Zero-Thalassemia Less than 2 years of age: every 3 months 2 years to 5 years of age: every 4 months Over 5 years of age: every 6 months.Hemoglobin SC Disease and Sickle Beta-Plus Thalassemia, and Hemoglobin EDisease Less than 2 years of age: every 3 months 2 years to 5 years of age: every 4 months Over 5 years of age: Document in the medical record, inform and educate the parentsand referring physician. They should be seen every 6 to 12 months.S-Hereditary Persistence of Fetal HemoglobinThese patients have hemoglobin F of 15% or more and the hemoglobin is homogenouslydistributed (i.e. each red blood cell has some hemoglobin F on Kliehauer-Betke stain).Please note: This diagnosis can only be made at 3-4 years of age, since this is whenpermanent hemoglobin distribution settles in. Once a diagnosis is made, they usuallyneed annual visits. Some children carrying this diagnosis may actually have a mild formof sickle cell anemia and may need closer follow-up.15
IIClinic Follow up After Hospital Discharge at University of Florida1.Vaso-Occlusive (painful) Event: Keep next regularly scheduled clinic appointment.2.Fever, Rule out Sepsis (with negative blood cultures) with or without pain: Keeppreviously scheduled appointment.3.Acute Chest Syndrome: Follow up within 7 days after discharge for physicalexamination, hemogram, reticulocyte count, pulse oximetry and an X-ray, if needed, todocument clearance of infiltrate. Pulmonary function testing should be arranged 2 monthsafter discharge.4.Aplastic Crisis: Follow up from 2 to 7 days later (depending upon patient’s dischargehemoglobin and reticulocyte count). Upon return to clinic, children should wear masksand be isolated from other patients until their reticulocyte count has risen over 1-2%.Siblings with sickle cell anemia who have not had an aplastic crisis should have ahemogram and reticulocyte count performed at once and again 7-14 days later due to thecontagiousness of parvovirus B19.5.Acute Splenic Sequestration Crisis (ASSC): Follow up 1 to 3 days later for ahemogram, check spleen size, and a general clinical status, until spleen size andhemogram are stable.6.Following elective surgery: Keep regularly scheduled clinic appointment.III.Use of Penicillin to Prevent Pneumococcal Infection1.Penicillin Prophylaxis in Sickle Cell Anemia and S-Beta-Zero Thalassemia Disease.Prophylaxis penicillin is initiated in all babies suspected of having sickle cell anemia orsickle beta-zero thalassemia at 1 to 3 months of age. Prophylaxis consists of penicillinVK 125 mg BID until 36 months of age and 250 mg BID thereafter. Tablets (crushed ifnecessary, for infants and small children) are preferred to suspension because of the short14 day shelf life and requirements for refrigeration of the suspension. Once prophylacticpenicillin is begun, it is continued until 5 years of age (exception noted below). Thesame protocol is followed for infants suspected of having S-C disease and S-Beta-Plusthalassemia.2.Based on the results of the PROPS II study, we recommend that routine prophylacticpenicillin be discontinued in all patients at five years of age (one month after the seconddose of pneumococcal polysaccharide vaccine is administered) with the exception of thefollowing. Parents may choose to continue prophylactic penicillin, and any patient whohas had a splenectomy should be placed on prophylactic penicillin for life. Patients whohave had a documented pneumococcal bacteremia should also receive penicillinprophylaxis indefinitely. Except for the above patients, penicillin prophylaxis is16
discontinued one month after the second dose of pneumococcal polysaccharide vaccine isadministered at 5 years of age.3.1Other Issues Regarding Penicillina.Routine prescription refills are given only during clinic visits and/or by telephoneduring working hours. At night or during the weekends sufficient medication isprescribed to cover the patient until the next regular working day. The family isinstructed to call the clinic for further refills.b.Prophylactic penicillin is generally not taken when the child is receivingtherapeutic antibiotics for another reason. The parent should be reminded toresume the penicillin following completion of the other antibiotic. Children whoare allergic to cephalosporin should remain on penicillin even while takinganother antibiotic to prevent sensitization.c.Children with a proven allergy to penicillin should receive prophylaxis witherythromycin. Children up to age 3 years of age should receive 125 mg bid andchildren over 3 years of age should receive 250 mg bid.7
IVImmunizations1.Pneumococcal Vaccine:Children with sickle cell disease are at high risk of invasive pneumococcal infection.Heptavalent pneumococcal conjugate vaccine (Prevnar) is recommended for universaluse in children 23 months and younger; to be given concurrently with otherrecommended childhood vaccines at 2, 4, 6 and 12 to 15 months of age. For children 7 to23 months old who have not received previous doses of Prevnar, administration of areduced number of doses is recommended. Two doses of Prevnar are recommended forchildren 24 to 59 months old at high risk of invasive pneumococcal infection-includingchildren with functional, anatomic, or congenital asplenia; infection with humanimmunodeficiency virus; and other predisposing conditions-who have not beenimmunized previously with Prevnar. Recommendations have been made for use of 23valent pneumococcal polysaccharide (23PS) vaccine in high-risk children at 2 years, 5years of age and later, to expand serotype coverage. High-risk children should be givenvaccines at the earliest possible opportunity. Use of antibiotic prophylaxis in childrenyounger than 5 years with functional or anatomic asplenia, including children with sicklecell disease, continues to be recommended. Children who have not experienced invasivepneumococcal infection and have received recommended pneumococcal immunizationsmay discontinue prophylaxis after 5 years of age.18
Recommended Immunization Schedule for Persons Aged 0 Through 6 Years—United States 2009For those who fall behind or start late, see the catch-up scheduleVaccine Age BirthHepB1Hepatitis B2Rotavirus3Diphtheria, Tetanus, Pertussis1month24612151819–23months months months months months months monthsHepBseefootnote 14–6yearsHepB2RVRVRVDTaPDTaPDTaP4seefootnote 3DTaPHaemophilus influenzae type bHibHibHibHib5PneumococcalPCVPCVPCVPCVInactivated PoliovirusIPVIPV42–3yearsDTaPPPSVIPVIPVRange ofrecommendedagesCertainhigh-riskgroupsInfluenza (Yearly)Influenza67Measles, Mumps, Rubella8VaricellaMMRsee footnote 7MMRVaricellasee footnote 8VaricellaHepA (2 doses)9Hepatitis A10MeningococcalThis schedule indicates the recommended ages for routine administrationof currently licensed vaccines, as of December 1, 2008, for children aged0 through 6 years. Any dose not administered at the recommended ageshould be administered at a subsequent visit, when indicated and feasible.Licensed combination vaccines may be used whenever any componentof the combination is indicated and other components are not contraindicatedand if approved by the Food and Drug Administration for that dose of1. Hepatitis B vaccine (HepB). (Minimum age: birth)At birth: Administer monovalent HepB to all newborns before hospital discharge. If mother is hepatitis B surface antigen (HBsAg)-positive, administer HepBand 0.5 mL of hepatitis B immune globulin (HBIG) within 12 hours of birth. If mother’s HBsAg status is unknown, administer HepB within 12 hours ofbirth. Determine mother’s HBsAg status as soon as possible and, ifHBsAg-positive, administer HBIG (no later than age 1 week).After the birth dose: The HepB series should be completed with either monovalent HepB or acombination vaccine containing HepB. The second dose should beadministered at age 1 or 2 months. The final dose should be administeredno earlier than age 24 weeks. Infants born to HBsAg-positive mothers should be tested for HBsAg andantibody to HBsAg (anti-HBs) after completion of at least 3 doses of theHepB series, at age 9 through 18 months (generally at the next well-child visit).4-month dose: Administration of 4 doses of HepB to infants is permissible when combinationvaccines containing HepB are administered after the birth dose.HepA SeriesMCVthe series. Providers should consult the relevant Advisory Committee onImmunization Practices statement for detailed recommendations, includinghigh-risk conditions: nically significant adverse events that follow immunization shouldbe reported to the Vaccine Adverse Event Reporting System (VAERS).Guidance about how to obtain and complete a VAERS form isavailable at http://www.vaers.hhs.gov or by telephone, 800-822-7967. Administer PPSV to children aged 2 years or older with certain underlyingmedical conditions (see MMWR 2000;49[No. RR-9]), including a cochlearimplant.6. Influenza vaccine. (Minimum age: 6 months for trivalent inactivatedinfluenza vaccine [TIV]; 2 years for live, attenuated influenza vaccine [LAIV]) Administer annually to children aged 6 months through 18 years. For healthy nonpregnant persons (i.e., those who do not have underlyingmedical conditions that predispose them to influenza complications) aged2 through 49 years, either LAIV or TIV may be used. Children receiving TIV should receive 0.25 mL if aged 6 through 35 monthsor 0.5 mL if aged 3 years or older. Administer 2 doses (separated by at least 4 weeks) to children aged youngerthan 9 years who are receiving influenza vaccine for the first time or whowere vaccinated for the first time during the previous influenza season butonly received 1 dose.7. Measles, mumps, and rubella vaccine (MMR). (Minimum age: 12 months) Administer the second dose at age 4 through 6 years. However, the seconddose may be administered before age 4, provided at least 28 days haveelapsed since the first dose.2. Rotavirus vaccine (RV). (Minimum age: 6 weeks) Administer the first dose at age 6 through 14 weeks (maximum age:14 weeks 6 days). Vaccination should not be initiated for infants aged15 weeks or older (i.e., 15 weeks 0 days or older). Administer the final dose in the series by age 8 months 0 days. If Rotarix is administered at ages 2 and 4 months, a dose at 6 months isnot indicated.8. Varicella vaccine. (Minimum age: 12 months) Administer the second dose at age 4 through 6 years. However, the seconddose may be administered before age 4, provided at least 3 months haveelapsed since the first dose. For children aged 12 months through 12 years the minimum intervalbetween doses is 3 months. However, if the second dose was administeredat least 28 days after the first dose, it can be accepted as valid.3. Diphtheria and tetanus toxoids and acellular pertussis vaccine (DTaP).9. Hepatitis A vaccine (HepA). (Minimum age: 12 months) Administer to all children aged 1 year (i.e., aged 12 through 23 months).Administer 2 doses at least 6 months apart. Children not fully vaccinated by age 2 years can be vaccinated atsubsequent visits. HepA also is recommended for children older than 1 year who live in areaswhere vaccination programs target older children or who are at increasedrisk of infection. See MMWR 2006;55(No. RR-7).(Minimum age: 6 weeks) The fourth dose may be administered as early as age 12 months, providedat least 6 months have elapsed since the third dose. Administer the final dose in the series at age 4 through 6 years.4. Haemophilus influenzae type b conjugate vaccine (Hib).(Minimum age: 6 weeks) If PRP-OMP (PedvaxHIB or Comvax [HepB-Hib]) is administered at ages2 and 4 months, a dose at age 6 months is not indicated. TriHiBit (DTaP/Hib) should not be used for doses at ages 2, 4, or 6 monthsbut can be used as the final dose in children aged 12 months or older.5. Pneumococcal vaccine. (Minimum age: 6 weeks for pneumococcal conjugatevaccine [PCV]; 2 years for pneumococcal polysaccharide vaccine [PPSV]) PCV is recommended for all children aged younger than 5 years.Administer 1 dose of PCV to all healthy children aged 24 through 59months who are not completely vaccinated for their age.10. Meningococcal vaccine. (Minimum age: 2 years for meningococcal conjugatevaccine [MCV] and for meningococcal polysaccharide vaccine [MPSV]) Administer MCV to children aged 2 through 10 years with terminal complementcomponent deficiency, anatomic or functional asplenia, and certain otherhigh-risk groups. See MMWR 2005;54(No. RR-7). Persons who received MPSV 3 or more years previously and who remainat increased risk for meningococcal disease should be revaccinated with MCV.CS103164The Recommended Immunization Schedules for Persons Aged 0 Through 18 Years are approved by the Advisory Committee on Immunization Practices (www.cdc.gov/vaccines/recs/acip),the American Academy of Pediatrics (http://www.aap.org), and the American Academy of Family Physicians (http://www.aafp.org).Department of Health and Human Services Centers for Disease Control and Prevention
Recommended Immunization Schedule for Persons Aged 7 Through 18 Years—United States 2009For those who fall behind or start late, see the schedule below and the catch-up scheduleVaccine Age 7–10 years11–12 years13–18 yearsTetanus, Diphtheria, Pertussis1see footnote 1TdapTdapHuman Papillomavirus2see footnote 2HPV (3 doses)HPV SeriesMCVMCVMCVMeningococcal3Range ofrecommendedagesInfluenza (Yearly)Influenza4Pneumococcal5PPSVHepatitis A6HepA SeriesHepatitis B7HepB SeriesIPV SeriesInactivated upsMMR SeriesMeasles, Mumps, Rubella9Varicella SeriesVaricella10This schedule indicates the recommended ages for routine administrationof currently licensed vaccines, as of December 1, 2008, for children aged7 through 18 years. Any dose not administered at the recommended ageshould be administered at a subsequent visit, when indicated and feasible.Licensed combination vaccines may be used whenever any component ofthe combination is indicated and other components are not contraindicatedand if approved by the Food and Drug Administration for that dose ofthe series. Providers should consult the relevant Advisory Committee onImmunization Practices statement for detailed recommendations, includinghigh-risk conditions: nically significant adverse events that follow immunization shouldbe reported to the Vaccine Adverse Event Reporting System (VAERS).Guidance about how to obtain and complete a VAERS form isavailable at http://www.vaers.hhs.gov or by telephone, 800-822-7967.1. Tetanus and diphtheria toxoids and acellular pertussis vaccine(Tdap). (Minimum age: 10 years for BOOSTRIX and 11 years for ADACEL )5. Pneumococcal polysaccharide vaccine (PPSV). Administer at age 11 or 12 years for those who have completed therecommended childhood DTP/DTaP vaccination series and havenot received a tetanus and diphtheria toxoid (Td) booster dose. P ersons aged 13 through 18 years who have not received Tdapshould receive a dose. A 5-year interval from the last Td dose is encouraged when Tdap isused as a booster dose; however, a shorter interval may be used ifpertussis immunity is needed.2. Human papillomavirus vaccine (HPV). (Minimum age: 9 years) A dminister the first dose to females at age 11 or 12 years. A dminister the second dose 2 months after the first dose and thethird dose 6 months after the first dose (at least 24 weeks after thefirst dose). A dminister the series to females at age 13 through 18 years if notpreviously vaccinated.3. Meningococcal conjugate vaccine (MCV). A dminister at age 11 or 12 years, or at age 13 through 18 years ifnot previously vaccinated. A dminister to previously unvaccinated college freshmen living ina dormitory. M CV is recommended for children aged 2 through 10 years withterminal complement component deficiency, anatomic or functionalasplenia, and certain other groups at high risk. See MMWR2005;54(No. RR-7). P ersons who received MPSV 5 or more years previously andremain at increased risk for meningococcal disease should berevaccinated with MCV.4. Influenza vaccine. A dminister annually to children aged 6 months through 18 years. F or healthy nonpregnant persons (i.e., those who do not haveunderlying medical conditions that predispose them to influenzacomplications) aged 2 through 49 years, either LAIV or TIV may be used. A dminister 2 doses (separated by at least 4 weeks) to children agedyounger than 9 years who are receiving influenza vaccine for thefirst time or who were vaccinated for the first time during the previousinfluenza season but only received 1 dose. A dminister to children with certain underlying medical conditions(see MMWR 1997;46[No. RR-8]), including a cochlear implant.A single revaccination should be administered to children withfunctional or anatomic asplenia or other immunocompromisingcondition after 5 years.6. Hepatitis A vaccine (HepA). A dminister 2 doses at least 6 months apart. H epA is recommended for children older than 1 year who live inareas where vaccination programs target older children or who areat increased risk of infection. See MMWR 2006;55(No. RR-7).7. Hepatitis B vaccine (HepB). A dminister the 3-dose series to those not previously vaccinated. A 2-dose series (separated by at least 4 months) of adult formulationRecombivax HB is licensed for children aged 11 through 15 years.8. Inactivated poliovirus vaccine (IPV). For children who received an all-IPV or all-oral poliovirus (OPV) series,a fourth dose is not necessary if the third dose was administered atage 4 years or older. I f both OPV and IPV were administered as part of a series, a total of4 doses should be administered, regardless of the child’s current age.9. Measles, mumps, and rubella vaccine (MMR). If not previously vaccinated, administer 2 doses or the second dosefor those who have received only 1 dose, with at least 28 daysbetween doses.10. Varicella vaccine. For persons aged 7 through 18 years without evidence of immunity(see MMWR 2007;56[No. RR-4]), administer 2 doses if not previouslyvaccinated or the second dose if they have received only 1 dose. For persons aged 7 through 12 years, the minimum intervalbetween doses is 3 months. However, if the second dose wasadministered at least 28 days after the first dose, it can be acceptedas valid. For persons aged 13 years and older, the minimum intervalbetween doses is 28 days.The Recommended Immunization Schedules for Persons Aged 0 Through 18 Years are approved by the Advisory Committee on Immunization Practices (www.cdc.gov/vaccines/recs/acip),CS103164the American Academy of Pediatrics (http://www.aap.org), and the American Academy of Family Physicians (http://www.aafp.org).Department of Health and Human Services Centers for Disease Control and Prevention
Catch-up Immunization Schedule for Persons Aged 4 Months Through 18 YearsWho Start Late or Who Are More Than 1 Month Behind—United States 2009The table below provides catch-up schedules and minimum intervals between doses for children whose vaccinations have been delayed. A vaccineseries does not need to be restarted, regardless of the time that has elapsed between doses. Use the section appropriate for the child’s age.CATCH-UP SCHEDULE FOR PERSONS AGED 4 MONTHS THROUGH 6 s, Pertussis3Minimum Interval Between DosesDose 2 to Dose 3Dose 3 to Dose 48 weeksMinimum Agefor Dose 1Dose 1 to Dose 2Birth4 weeks6 wks4 weeks4 weeks26 wks4 weeks4 weeks(and at least 16 weeks after first dose)8 weeks (as final dose)if first dose administered at age 12-14 monthsNo further doses neededif first dose administered at age15 months or older4 weeks6 wksif current age is younger than 12 months8 weeks (as final dose)4if current age is 12 months or older andsecond dose administered at younger thanage 15 monthsNo further doses needed8 weeks(as final dose for healthy children)if first dose administered at age 12 months orolder or current age 24 through 59 months4 weeksif current age is younger than 12 months8 weeks(as final dose for healthy children)if current age is 12 months or olderNo further doses neededNo further doses neededfor healthy children if previous doseadministered at age 24 months or older4 weeksfor healthy children if first dose administeredat age 24 months or olderInactivated Poliovirus66 wks4 weeksMeasles, Mumps, Rubella712 mos4 weeksVaricella812 mos3 monthsHepatitis A912 mos6 months8 weeks (as final dose)This dose only necessary forchildren aged 12 months through59 months who received 3 dosesbefore age 12 monthsif previous dose administered at age15 months or olderif first dose administered at younger thanage 12 monthsPneumococcal 56 months34 weeks4 weeks6 wks6 months4if first dose administered at younger thanage 12 monthsHaemophilusinfluenzae type b4Dose 4 to Dose 58 weeks (as final dose)This dose only necessary forchildren aged 12 months through59 months who received 3 dosesbefore age 12 months or forhigh-risk children who received3 doses at any age4 weeks6CATCH-UP SCHEDULE FOR PERSONS AGED 7 THROUGH 18 YEARSTetanus,Diphtheria/Tetanus, Diphtheria,Pertussis10Human Papillomavirus114 weeks107 yrsif first dose administered at younger thanage 12 months4 weeks6 monthsif first dose administered at age 12 months or older9 yrsRoutine dosing intervals are recommended11HepatitisA912 mos6 monthsHepatitisB1Birth4 weeks(and at least 16 weeks after first dose)6 wks4 weeks4 weeksInactivated Poliovirus6Measles, Mumps, Rubella712 mos6 monthsif first dose administered atyounger than age 12 months8 weeks4 weeks64 weeks3 monthsVaricella812 mosif the person is younger than age 13 years4 weeksif the person is aged 13 years or older1. Hepatitis B vaccine (HepB). Administer the 3-dose series to those not previously vaccinated. A 2-dose series (separated by at least 4 months) of adult formulation Recombivax HB is licensedfor children aged 11 through 15 years.2. Rotavirus vaccine (RV). The maximum age for the first dose is 14 weeks 6 days. Vaccination should not be initiated forinfants aged 15 weeks or older (i.e., 15 weeks 0 days or older). Administer the final dose in the series by age 8 months 0 days. If Rotarix was administered for the first and second doses, a third dose is not indicated.3. Diphtheria and tetanus toxoids and acellular pertussis vaccine (DTaP). The fifth dose is not necessary if the fourth dose was administered at age 4 years or older.4. Haemophilus influenzae type b conjugate vaccine (Hib). Hib vaccine is not generally recommended for persons aged 5 years or older. No efficacy data areavailable on which to base a recommendation concerning use of Hib vaccine for older children andadults. However, studies suggest good immunogenicity in persons who have sickle cell disease,leukemia, or HIV infection, or who have had a splenectomy; administering 1 dose of Hib vaccine tothese persons is not contraindicated. If the first 2 doses were PRP-OMP (PedvaxHIB or Comvax ), and administered at age 11 monthsor younger, the third (and final) dose should be administered at age 12 through 15 months and atleast 8 weeks after the second dose. If the first dose was administered at age 7 through 11 months, administer 2 doses separated by 4weeks and a final dose at age 12 through 15 months.6. Inactivated poliovirus vaccine (IPV). For children who received an all-IPV or all-oral poliovirus (OPV) series, a fourth dose is notnecessary if the third dose was administered at age 4 years or older. If both OPV and IPV were administered as part of a series, a total of 4 doses should be administered,regardless of the child’s current age.7. Measles, mumps, and rubella vaccine (MMR). Administer the second dose at age 4 through 6 years. However, the second dose may beadministered before age 4, provided at least 28 days have elapsed since the first dose. If not previously vaccinated, administer 2 doses with at least 28 days between doses.8. Varicella vaccine. Administer the second dose at age 4 through 6 years. However,
The Sickle Cell clinic is located at the Shands Medical Plaza on the second floor. Address Pediatric Specialty Clinic 2000 SW Archer Road Gainesville, Florida 32610-0383 Clinic Days Patients with sickle cell disease are seen in the clinic on any scheduled clinic day but are mainly seen on Mondays and Wednesdays. Primary Care