Transcription
3/29/2015Tracheostomy Tubes and Speaking ValvesMississippi Speech-Language-Hearing AssociationApril 1, 2015Presenter Leigh Anne Baker, M.S.,CCC-SLP, BCS-S Passy-Muir Inc. ClinicalConsultant Director of ClinicalEducation at SouthernUniversity in Baton Rouge,LAlbaker@passy-muir.comFinancial Disclosure: Passy-Muir, Inc. has provided financial support for my travel to Jackson and aspeaking fee for this presentation.Non-Financial Disclosure: I receive a salary from Southern University as the Director of ClinicalEducation for the Department of Speech-Language PathologyDisclosure StatementLearning Objectives: Passy-Muir, Inc. has developed and patenteda licensed technology trademarked as thePassy-Muir Tracheostomy and VentilatorSwallowing and Speaking Valve. Thispresentation will focus primarily on the biasedclosed position Passy-Muir Valve and willinclude little to no information on otherspeaking valves. Tracheotomy andTracheostomy Tubes Passy-Muir Valves InterprofessionalEducation and PracticeIndications for Tracheostomy TubeTracheostomy and mechanical ventilationcan have devastating effects oncommunication and swallowing. Prolonged intubationLong-term mechanical ventilationPermanent tracheostomy tubeInability to intubate due to traumaAirway protection/secretion removalAirway anomalyPatient comfortFacilitate weaningOral feeding and communication optionsA tracheostomy tube does not prevent aspiration1
3/29/2015There are many choices of tubes!!!!Parts of a tracheostomy tubeNeck flange15 mm connectorTube shaftInflation lineCuffPilot port with one wayvalveTracheostomy Tubes Single Lumen/CannulaTypes of Tubes Double Lumen/Cannula MATERIALS– PVC, Silicone, Metal– Metal Reinforced SHAPE– Curved, Angular, Nonpre formed LENGTH– Standard– Extra length Proximal Distal Adjustable FlanCalculating Tube Size Anterior/PosteriorDiameter of trachea– Male:18 /- 5mm– Female: 12 /- 3 mmSINGLE LUMENDOUBLE LUMENFENESTRATEDMRI COMPATIBLE– Conditional Subglottic Suction TRACH TALK CUFFS– Air, water, or foam– Double cuffed– Un-cuffed Custom MadeJackson Metal Tracheostomy Tubes ATS Consensus: Thetracheostomy tubeshould take up no morethan 2/3 the innerdiameter of thetrachea.(for pediatrics, no adult standard) Original Styletrachea ImprovedI.D.tube Permanent 15mmAdapterKamel, et al 20092
3/29/2015Cuff ChoicesNot all Trach Sizes are Equal AIR FILLED – minimalleakSize 6.0 Tracheostomy TubeIDOD LPortex6.0 8.3 55.0 TTS : WATER FILLED –minimal occlusion (canbe air filled)Bivona6.0Shiley6.4 10.8 74.0SCT FOME-Cuff – selfsealing6.08.88.370.067.0– Contraindicated forPassy-Muir Valve useEarly Tracheostomy (7-10 days) May:Complications of the Tracheostomy Tube Reduce incidence ofHospital-AcquiredPneumonia Reduce injury to larynx Improve patient comfort Allow for oralcommunication and oraldiet and requirement forless sedation Improve oral hygiene Improve secretionmanagementClinical Complications of the TracheostomyAirflowClinical Complications (Continued) Lack of vocal productioncommunication Decreased sense ofsmell/taste Limited airflow throughupper airway Reduced cougheffectiveness Complications of long termcuff inflation Psychologicalcomplications-agony, fear,panic, frustration Removal of naturalfiltration andhumidification system Cycle of irritation andsecretion production Decreased Sensation inthe oropharynx Poor secretionmanagement(Siebens, Tippet, Kirby, & French, 1993)3
3/29/2015Clinical Complications (Continued) Lack of subglotticpressure (0cmH20) Decreased physiologicPEEP (positive endexpiratory pressure)AirflowTracheostomy Tube Effect on Swallowing: Scar tissue formation fromthe tracheotomyprocedure may affix thetrachea to overlying tissuesand the larynx may notmove freelyIf the tube is too large forthe patient’s trachea,patient may feeldiscomfort and maycompensate with reducedlaryngeal excursionEibling & Gross,1996; Gross, Atwood, Grayhack, & Shaiman ,2003Tracheostomy Tube Effect on Swallowing Impaired oralpharyngeal pressure Impaired hyolaryngealelevation/excursion Impaired glottic closure Reduced subglotticpressures and reducedsensation Muscle disuse atrophyTracheostomy and Aspiration Does a cuff preventaspiration? Definition Incidence of aspiration– 50% - 87% rate for trachand vent patients1– 75% silent aspiration2– Aspiration around thecuff31.Elpern et al., 1987, 1994, 2000; Tolep et al., 19962.Davis & Stanton, 2004; Elpern et aI., 19943.Bone, Davis, Zuidema, & Cameron, 1974; Elpem et al.,1987; Nash, 1988; Pavlin, VanNimwegan,& Hombein, 1975; Ross & White, 2003Complications of Cuff Inflated cuffs can tetherlarynx– Larynx does not elevate Epiglottis does projectdown to protect airway– Larynx does not moveanteriorly Esophagus does notincrease its diameter,creating the vacuumenvironment for foodbolus transitionCuff mismanagement associated with: Tracheal stenosis Granulation tissueformation Tracheal erosion Tracheoesophagealfistula Tracheal dilation Esophageal impingement Reflux Necrosis and TraumaAmathieu, R. et al. (2012). British Journal of Anaesthesia. 109(4):578-83.4
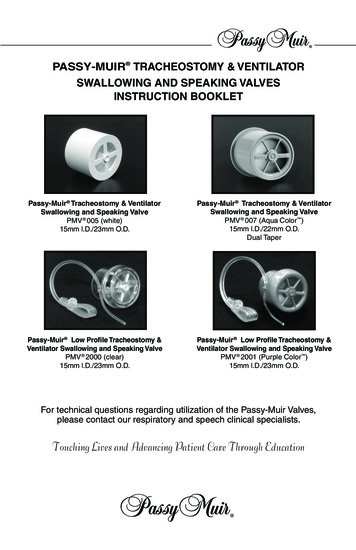
3/29/2015Cuff Deflation Benefitsaspiration1, 2 Reduces Improves laryngealelevation2,3 Weaning time was shorter average of 3 days versus 8days4 Fewer respiratory infectionsincluding ventilatorassociated pneumonia(20% vs. 36%) 4 Swallowing better andimproved more frombaseline41. Davis, et al. (2002). Journal of Intensive Care Medicine. 17(3): 132-135.2. Ding, R. & Logeman, J. (2005). Head & Neck. 27(9):809-133. Amathieu, R., et al. British journal of anaesthesia109.4 (2012): 578-583.4. Hernendez, et al. (2013). Intensive Care Medicine. 39(6):1063-70The Passy-Muir Tracheostomy & VentilatorSwallowing and Speaking ValvePMA 2000 Oxygen AdapterCuff deflation Adequate ventilation can still be achieved withthe tracheostomy tube cuff deflated.1 Cuff deflation during continuous positive airwaypressure (CPAP) has been associated with stablerespiratory parameters and allowed patients tovocalize and swallow. 21. Bach, J. & Alba, J. (1990). Tracheostomy Ventilation: A study of efficacy with deflated cuffs and cuffless tubes. Chest, 97: 679-83.2. Conway, D. & Mackie, C. (2004). The effects of tracheostomy cuff deflation during continuous positive airway pressure. Anaesthesia, 59: 652657.PMV 2000 (clear) and PMV 2001 (Purple)PMV 007 (Aqua Color )5
3/29/2015PMV 2020 with Jackson ImprovedCare, Cleaning, and Lifetime of the Passy-Muir Speaking Valves Average lifetime of 2 monthsHow Does The Valve Work?Patented “no leak” designOpens only during activeinspirationCloses at end inspirationRemains closed t/oexpiratory cycleAir is re-directed thru theupper airwayOffers a buffer tosecretionsDESIGN VIDEOPhysiologic Benefits of Passy-Muir valve“Set Yourself and Your Patient Up For Success!” RestoresVoice/Communication Improves Swallowing Restores Physiologic PEEP Improves SecretionManagement Improves Oxygenation Promotes Weaning andDecannulation May Decrease Risk ofAspiration May improve exercise andbalance Improves Smell & Taste6
3/29/2015Team t ticianCognitive Status-Awake,ResponsiveAttempting to Communicate– limited sedation needsMedically StableAble to Tolerate CuffDeflationAble to Manage SecretionsorallyHave a patent upper airwayRespiratory TherapistPlacement GuidelinesPatient educationPeer educationPatient positionSuctioningAchieve complete cuffdeflation Use the warning labelprovided withpackaging To Assess for Upper Airway Patency Deflate cuff Ask patient to inhale Finger occlude andvoice or cough onexhalation Use mirrors, cotton,whistles or bubbles toassist with the oralexhalation process Pressure from trach(whoosh)Patient Assessment OxygenationVital SignsBreath SoundsColorWOB - abdominalsPatient ResponsivenessFactors Affecting Upper Airway PatencyTracheostomy tube sizeEdemaGranulation tissueVocal fold paresis inadductor position Tracheal stenosis Secretions 7
3/29/2015Downsizing the Tracheostomy Improves expiratorypressures1 Improves speaking valveand cappingrecommendations,comfort and tolerance1 Associated with earlieroral intake and reducedlength of stay2 Improves weaning forspontaneous breathingtrials3Other Considerations to Increase Airflow Cuffless Fenestrated Consider ENT consult1. Johnson , JD et al. (2009). The Clinical Respiratory Journal 2009; 3: 8–14.2. Fisher, D. et al. (2013). Respiratory Care. 2013 Feb;58(2):257-63.3. Hernandez, G. et al. (2013). Intensive Care Medicine. Jun;39(6):1063-70Ventilator Criteria Suggestions Patient on .60 FiO2 PEEP requirements of 10cm H2O PIP less than 40cm H2OTube Position is ImportantPatient Guidelines Patient Education Peer Education – teamapproach! Body Position andPosture Position of Head andNeck Achieve Cuff Deflation –slowly! (Pulmonary Toilet) 100% Cuff Deflation isMandatoryPlacement of Passy-Muir Valve Gentle quarter turn twist while stabilizing the flange oftracheostomy tube8
3/29/2015Ventilation Terminology“Must Knows” for Passy-Muir Valve Use! FiO2 oxygen % ( 60%) PEEP positive end expiratory pressure( 10cmH2O)– Pressure in our lungs at end exhalation (the air we cannever exhale that maintains lung inflation) Vt volume of delivered vent breath (cc’s) PIP/PAP peak airway pressure ( 40)Assessment Criteria Observe pre-cuff deflation PIPObserve pre-cuff deflation exhaled VtAchieve cuff deflation – slowly over 5 minutesLook for 40 - 50% loss of exhaled VtLook for significant drop in PIPQ: What does this indicate?– How much driving pressure from the machine is requiredto deliver the set VtAssessment CriteriaA: This assessmentindicates that thepatient can exhalearound the properlysized tracheostomytube, and the airwayabove the cuff is mostlikely patent.Cuff Inflated-Closed CircuitAssessment Criteria 100% cuff deflation Patient must be able to exhale past thetracheostomy tube and through upper airway Assess air leak/decreased ventilation Compensate with ventilator changesCuff Deflated-Open Circuit250cc5 cmH20.30FiO2PEEPPIP25cmH2O0 9
3/29/2015Passy-Muir Valve In-lineVentilator Adjustments500cc0 cmH20.30FiO2PEEPPIP10cmH2O700cc0 cmH20PEEPVt500cc0ccVentilator Assessment and Adjustments PEEP on/off Volume compensation during cuff deflation– Increase Vt in small increments to achieve pre-cuffdeflation pressures (PIP) Use low pressure alarm as disconnect/indirect lowexhaled Vt alarm (set above 10cm H20) Set high pressure limit appropriately (10–15cm H20above the PIP)Review Adjust PEEP Slow cuff deflation Monitor pressure/volumeloss Place Passy-Muir Valve Compensate forvolume/pressure loss Time limit PS breaths Set alarms appropriatelyPIP20cmH2O.30FiO215cm H2030cm H20Vt700cc0ccVentilator Assessment and Adjustments Pressure versus flow trigger Pressure Support (PS)– Use E-Sense, inspiratory cycle off, or set I-time to time limitPS breath Pressure Control– Set I-Time Consider NIPPV modeVentilator Alarms forPassy-Muir Valve Applications Low exhaled Vt Low pressure alarm – MUST be set 5 to 10 cm belowPIP High pressure alarm – Should be set 10cm abovePIP10
3/29/2015HumidificationVentilator ConnectionsDual-Axis Swivel Heat/moisture exchanger (HME) is ineffective Use heated humidified system Remove Passy-Muir Valve for medicatedtreatmentOmni-Flex 15mmx22mmStep Down Adapter22/22mmSilicone AdaptorCuff Inflated-Closed CircuitCuff Deflated-Open CircuitPEEP300cc300ccVT150cc25cmH2O300ccPIPPMV In-linePEEP150cc5 cmH20VT0 cmH2012cmH2OPIPVentilator Adjustments300cc0 cc0 cmH200 cc0 PIP11
3/29/2015Ventilator Assessment and AdjustmentsVentilator Assessment and Adjustments Volume Compensation During Cuff Deflation– Increase VT in small increments to achieve pre-cuffdeflation pressures (PIP) PEEP Off Volume compensationduring cuff deflation Pressure Compensation During Cuff Deflation– Seldom increase PC (sometimes decrease) in smallincrements to achieve audible voice and adequateventilationUse low pressure alarm asdisconnect/indirect lowexhaled Vt alarm (set above10cm H20)Set high pressure limitappropriately (10-15cm H20above the PIP)Flow/Time Limit Pressure Support BreathsFlow limit The pressure supportbreath by increasing the% flow deceleration thatmust be reached priorto breath termination– Ranges 20 to 80%Patient Assessment Time limit Set Ti time– A typical setting for mostadults is 1 secondReview Adjust PEEP Slow cuff deflation Monitor pressure/volumeloss Place Passy-Muir Valve Compensate forvolume/pressure loss Time/flow limit PSbreaths Set alarms appropriatelyLimiting Pressure Support BreathsOxygenationVital SignsBreath SoundsColorWOB - abdominalsPatient ResponsivenessAssess for back pressure(PSSH sound)12
3/29/2015The IHI Triple Aim Interdisciplinary Education andPractice ges/default.aspxPatient/Family Engagement Promote patient/family engagement for selfmanagement and assistance with functional goalsetting with a focus on#1Strategies to Improve Patient Experienceof CareRoles/Responsibilities – Function– Impact on the patient’s ability to participate in life– Outcomes that matter to the patient. RESULT:– Quicker weaning and increased speaking valve use (Speed& Harding, 2012)– Shorter decannulation time and length of stay (Tobin &Santamaria, 2008)Promise Tracheostomy TeamSpeech-Language PathologistRespiratory TherapistNurseCertified Nursing AssistantPhysicianPhysical TherapistOccupational TherapistRehabilitation TechnologistDietitian13
3/29/2015Specialized Role of the Speech-LanguagePathologist Completing communication and swallowingevaluations and treatments specific to the patientwith a tracheostomy tube and mechanicalventilation Leading or facilitating the communicationbetween the team and the patients in manyaspects of care, including patient education ontracheostomy care, speaking valve placementand safety for oral intake.Tracheostomized/Ventilated Patient Tracheostomy tube size and fitPresence or absence of a cuffUpper airway patencyVentilator settings (mode, respiratory rate, PEEP,FiO2)Documentation/Technology Speech-Language Pathologists must streamlinethe documentation process and utilize innovativetechnology to reduce the per capital cost ofhealth care (e.g., team meetings, rounds, ongoingcompetency trainings, policies and procedures).– Ad Hoc Committee on Reframing theProfessions (December 2013)Things I needed to know but didn’t Transdisciplinary skills––––––Oral and tracheal suctioningPEG tubesNasogastric tubesIVsVentilators (what it did, what the setting meant)Interaction between the tracheostomy tube andventilatorSpecialized Role of the Speech-LanguagePathologist Result:– Individualized care– Early intervention (Burkhead, L, 2011)– Increase staff efficiency– Burkhead, L. (2011). Swallowing Evaluation and VentilatorDependency – Considerations and Contemporary Approaches.Perspectives on Swallowing and Swallowing Disorders(Dysphagia) March 2011 20:18-22.Documentation General staffing meetingsTracheostomy team meetingsCompetency trainingPolicies and procedures14
3/29/2015Technology Benefits of cuff deflation Speaking valve use DecannulationCollaborative Education Benefits of speech therapy services for thetracheostomized and ventilated patient:– Cuff deflation and speaking valve use– Tracheostomy systems– Augmentative and alternative communication Result:– Improved patient outcomesExpertise of the Speech-LanguagePathologistSLP can provide specialized training for otherdisciplines Higher level of skilled training and competency– Post-graduation through continuing education efforts andon-the-job training.– My expertise came from: Continuing education coursesOn-The-Job trainingConsulting workSpeaking engagementsSkills that SLP may need training on RT Training Group of SLPsSuctioningIndications for tracheostomyComplications of tracheostomy tubesRelationship between respiration and swallowingTechnology and interventionsCuff managementSpeaking valve useTracheostomy careVentilator settings and alarms15
3/29/2015Things SLP can train RT on Speaking valve useTechniques for speaking and swallowingAirway patencyBenefits of cuff deflationJoint Roles and Responsibilities Speech-Language Pathologist and RespiratoryTherapist– Result: Indications for early intervention. Discipline-specific and transdisciplinary roles andresponsibilities Specialized collaborations between SLPs and RespiratoryTherapistsTracheostomy Teams Positive Outcomes:– increased speaking valve use– quicker weaning and decannulation– reduction in adverse events– potential for financial savings for institutions Cameron et al. (2009) - Tracheostomy Review andManagement Service Yu, M. (2010) Wilcox and Schmidt (2009)#2Strategies for Reducing Per Capita Costs(Speed and Harding, 2012; Leblanc et al., 2010; Garrubba etal., 2009; Tobin and Santamaria, 2008; Norwood et al., 2004).Direct vs. Consultative Model Speech-Language Pathologists must shift the focusfrom direct service to a consultative model– (Ad Hoc Committee on Reframing the Professions ofSpeech-Language Pathology and Audiology, December2013) The patient and family are educated and trainedto practice between visits, for example: use ofspeaking valves, tracheostomy care, andoral/tracheal suctioning. Result: Continuum of CareInterprofessional Education Examples of interprofessional education– Co-curricular education (in-services, webinars withmultidisciplinary attendance)– Core competences for collaborative practice– Formal vs. informal activities Staff meetings Lunch and Learn with vendors16
3/29/2015Educating Future Clinicians Benefits of having clinical practicum participantsengaged in transdisciplinary care Concurrent supervision by Speech-LanguagePathologists and professionals outside ofcommunication sciences and disorders (Ad HocCommittee on Interprofessional Education,November 2013).– Respiratory Therapist – tracheostomy care– Nurse – PEG tube– Dietitian – diet modificationsFacilitate Communication If speech-language pathologistsfacilitate communication betweenhealth care providers and patients– enhance medical environments (e.g., ICU) for bettercommunication. Result: Health care providers and patients willcomprehend and participate more effectively inmanaging their medical conditions and careTeam Development Prove process success by:– Collecting outcome measures– Obtaining media coverage for public education– Presentations at health care conferences to furtherchanges in healthcare practices.#3Strategies to Improve the Health ofPopulationsOutcome Measures Speech-language pathologists must utilizeoutcomes measures with data collection thatfocuses on quality care with reduced costs topatients and to healthcare. Results: weaning rates, decannulation rates,adverse event rates, aspiration rates, oral intakeprogression, and length of stay.Where we are today New mind sets Faster consults More aggressive treatments sooner Results:– Buy-In from other professionals– Marketing opportunities– Successful programs17
3/29/2015Interprofessional Education and atory icianRespiratory TherapistTracheostomy Teams Increased speaking valve useImproved decannulation timeReduce Length of Stay (LOS)Reduced costsSpeed, Lauren, and Katherine E. Harding. Journal of Critical Care (2012).Interprofessional Practice What the SLP and RT can do together:– Co-treat during speech and swallowing treatments– Collaboratively reassess as needed– Provide interprofessional treatment plansMulti-disciplinary Tracheostomy WeaningProtocols Increase amount ofpatients decannulated Reduce time todecannulation Assign clearresponsibilities to teammembers “The tracheostomy tubedecannulation process iswell suited for therapistimplementedprotocols.”Christopher, KL. (2005). Respiratory Care, Vol 5018
3/29/2015Speech Techniques to Increase VocalizationNow that my patient has on the Passy-Muirvalve, and I have a successfulinterprofessional team in place, whattreatment should I do?What’s the problem? Is the patient mouthing words?Airway patency issues?Vocal fold paresis/paralysis?Poor breath support?Poor coordination?Cognitive/linguistic issues?Candidate for downsize or decannulation?Candidate for vocal techniques/technologies?SebastianIs the patient mouthing words? Yes Patient Assessment: The patient tolerates thevalve and vitals are WFL No voiceTechniques: Ask the patient to cough,hum, blow For children: Play, tickleAirway patency issues Noted by desaturation,difficulty breathing,incomplete exhalationthrough upper airway,pressure from trach tubeupon removal of valve Diagnosis of trachealmalacia or stenosis Muffled voiceWhat can I do:Assess airway patencyDownsizeXLT Distal trach to bypassan obstruction ENTconsult/bronchoscopy 19
3/29/2015Tube Position is ImportantVideo: Patency IssuesVideo: Patency Issue ResolvedVocal fold paresis/paralysis Vocal Folds in abductedposition– Good tolerance ofvalve– Whispery voice– Cough is weakPoor Breath Support Voice “runs out of air” Typical for patients withspinal cord injury,neuromuscular disorders What can I do: ENT consult Vocal fold adductionexercises once assessedby ENTPoor breathing/speaking coordination What can I do: Diaphragmatic breathingexercises Expiratory musclestrength training Vent may causeincoordination Patient may speak oninhalation andexhalation What can I do? Set i-time on ventilator Increase/decrease setrespiratory rate Coordinate speech onexhalation20
3/29/2015APPLICATION AND PLACEMENT OF THE PASSY-MUIR VALVECognitive-Linguistic Deficits: Traumatic brain injury Stroke ApraxiaPatient in Coma with Passy-Muir Valve What can I do? Place the Passy-Muir Valve Continue with speechtherapy treatmentDownsizing the Tracheostomy Tube Improves expiratorypressures1 Improves speaking valveand cappingrecommendations,comfort and tolerance1 Associated with earlieroral intake and reducedlength of stay2 Improves weaning forspontaneous breathingtrials3Other Considerations to Increase Airflow Cuffless Fenestrated Consider ENT consult1. Johnson , JD et al. (2009). The Clinical Respiratory Journal 2009; 3: 8–14.2. Fisher, D. et al. (2013). Respiratory Care. 2013 Feb;58(2):257-63.3. Hernandez, G. et al. (2013). Intensive Care Medicine. Jun;39(6):1063-70DecannulationPre-Decannulation Improves cough and swallow which are indicatorsof decannulation Removal of the trach is first recommendation byCDC to reduce pneumonia How can we decannulate faster?-Early speaking valve use-Protocols-Tracheostomy team21
3/29/2015Post DecannulationCandidates for Decannulation Consider the original reason for the trach Weaned from mechanical ventilation, effectivecoughing, no significant upper airway lesion1 Absence of distress, stable arterial blood gases,hemodynamic stability, absent fever1 A peak cough flow of 160 liters/minute2 Survey: patient’s level of consciousness, cougheffectiveness, secretions, oxygenation31. Christopher, K.(2005). Respiratory Therapy. 50(4):538 –54.2. Bach & Saporito, (1996). Chest. 110(6): 1566-71.Stelfox, H. et al (2009). Respiratory Care. 54(12): 1658-68.Vocal Technologies/Techniques:Techniques for Swallow Management Technologies:– Blom Trach– Capping– AAC devices Techniques:– Blowing activities with visual feedback– Digital occlusion– Visual and tactile sensory feedback to elicit voice onsetDisuse Atrophy Mechanical ventilationcan cause atrophy, andinjury of diaphragmaticmuscle fibers “Patients in intensivecare lose about 2% ofmuscle mass a dayduring their illness.”1 Muscle weaknesspredicts pharyngealdysfunction21.2.Jaber, S.et al, 2011; Griffiths, BMJ, 1999Mirzakhani, H. et al Anesthesiology. 2013Cuff deflation Cuff deflation must beachieved to fully assessthe pharyngeal stage ofthe swallow. “An individual who is somedically fragile as topreclude cuff deflationis not usually acandidate for significantoral intake.”Dikeman, K, Kazandjian, M, 200322
3/29/2015Effect of Mechanical Ventilation on Swallowing: Ventilator modes with apre-set breath may pushair at a time the patientis trying to maintainairway closure for aswallow. If the cuff is deflated,without a Passy-Muir valve, a translaryngealleak may occur oninspiration andexpiration.Cuff Deflation Benefits for Swallow Reduces aspiration1, 2Improves laryngealelevationWeaning time was shorterin cuff deflated -averageof 3 days versus 8 days3Fewer respiratory infectionsincluding ventilatorassociated pneumonia incuff deflated group (20%vs. 36%) 3Swallowing better in cuffdeflated group andimproved more frombaseline31. Davis, et al. (2002). Journal of Intensive Care Medicine. 17(3): 132-135.2. Ding, R. & Logeman, J. (2005). Head & Neck. 27(9):809-133. Hernendez, et al. (2013). Intensive Care Medicine. 39(6):1063-70Early Use of a Passy-Muir Valve forSwallowing Evaluation and RehabilitationSwallowing TreatmentEarly placement of the Passy-Muir Valve mayprovide “physical therapy” to the upper airway,helping to reduce effect of muscle atrophy, andimprove pharyngeal and laryngeal swallowingfunction.”Burkhead, 2007 One Way Valve Reduces Aspiration Further Improved scores onpenetration-aspiration scale1 Restores expiratory airflow2 Improves laryngealclearance2 Improved secretion ratingscale3 Maintain lung volumes4 Restores subglottic airpressure51.2.3.4.5.Re-connects the upper andlower airway and normalizesthe aerodigestive tract andprevents disuse atrophy.Allow patients tocommunicate orally andactively participate inhealthcare decision making.Perform swallow treatmentas if your patient did nothave a tracheostomy tubeonce the Passy-Muir Valveis in place.Goal of decannulationWhat’s the problem? Reduced base of tongue strength? Reduced laryngeal elevation? Reduced vocal fold closure?Suiter, D. Head and Neck. 2005. Sep;27(9):809-13Prigent, Helene. Intensive Care Med. 2012 June38(1):85-90.Blumenfeld, L. Oral Abstract Presented at Dysphagia Research Society Annual Meeting 2012Gross, R., et al. (2006). The Laryngoscope, 116:753-761Eibling, D., & Gross, R. (1996). Annals of Otology, Rhinology, & Laryngology, 105(4):253-8.23
3/29/2015Therapy: Frequent Swallow Techniques withthe Passy-Muir Valve Base of tongueweaknessFrequent Swallow Techniques with the PassyMuir Valve Vocal fold adductionexercises– Forceful phonation(/ha-ha)– Coughing, throatclearing– Pressure against aresisting force– Masako Maneuver Laryngeal excursion– Pitch gliding– Effortful swallow– Mendelsohn Maneuver Vocal Fold abduction– Sniff and breathe outthrough mouthVENTILATOR APPLICATION OF THE PASSY-MUIR VALVEVideo from Madonna swallow exercise https://www.youtube.com/watch?v d168L1E8tX0&list UUrJ BmcqlCosF1heNCiLWKg&feature c4overviewCompensatory swallowing strategies No StrawsSmall Bites/SipsAssistance/Supervision withMealsSit UprightDon’t Talk While EatingEat SlowlyAlternate Solids & LiquidsDouble/Multiple SwallowsClear Throat after SwallowingEffortful SwallowLingual sweepStraw progressionLiquid washVisual inspection s/p swallowImposed rest breaks Chin Tuck toHead Tilt toLRChew food on the L RHead Turn to L RCheck for DenturesCrush medications-Consult MDfirstAvoid foods with small piecesRemain upright for minutesThicken LiquidsAvoid certain foodsVerbal/Visual/Tactile CuesBite size awarenessPosture or position during andafter eatingCompensatory Strategies and Diet Modifications Generally the same asnon-trach/non-ventilatordependent patientsModifications in diet textures NDD Level 1: Dysphagia-Pureed (homogenous, verycohesive, pudding-like, requiring very little chewingability). NDD Level 2: Dysphagia-Mechanical Altered (cohesive,moist, semisolid foods, requiring some chewing). NDD Level 3: Dysphagia-Advanced (soft foods thatrequire more chewing ability). Regular (all foods allowed). McCullough, G. , Pelletier, C. & Steele, C. (2003,November 04). National Dysphagia Diet: What toSwallow?. The ASHA Leader24
3/29/2015Liquids Proposed terms for liquids and correlating viscosityranges:1. Thin 1-50 centiPoise (cP)2. Nectar-like 51-350 cP3. Honey-like 351-1,750 cP4. Spoon-thick 1,750 cPTreatment Considerations Coordinate breathing andswallowing.Time the swallow withhigher lung volumes.Improve cough.Mobilize lung and oralpharyngeal secretions.Expiratory muscle strengthtraining.– The Breather– Acapella– EMT McCullough, G. , Pelletier, C. & Steele, C. (2003,November 04). National Dysphagia Diet: What toSwallow?. The ASHA LeaderVENTILATOR APPLICATION OF THE PASSY-MUIR VALVEAssessing Cough StrengthPeak Cough Expiratory Flow Greater than 160L/min are needed toclear secretionsRespiratory Muscle Training Therapy to assist in lungexpansion, coughingand airway clearance– Acapella– The BreatherMiller, R.G. et.al.(2009). Neurology 13; 73(15): 1218-1226FEES Before and After Passy-Muir Valve http://www.passy-muir.com/pmvideos Liza Blumenfeld, MS, CCC-SLP, Scripps MemorialHospital, La Jolla, CASensory Awareness Non‐food taste stimulationThermal stimulationTaste stimulationTactile and verbal cues25
3/29/2015Q and AThank you!26
Improve oral hygiene Improve secretion management Complications of the Tracheostomy Tube Clinical Complications of the Tracheostomy Clinical Lack of vocal production-communication Decreased sense of smell/taste Limited airflow through upper airway Reduced cough effectiveness Complications of long term cuff inflation