Transcription
2 019B E N E F I T SG U I D EM A N AG E M E N T1
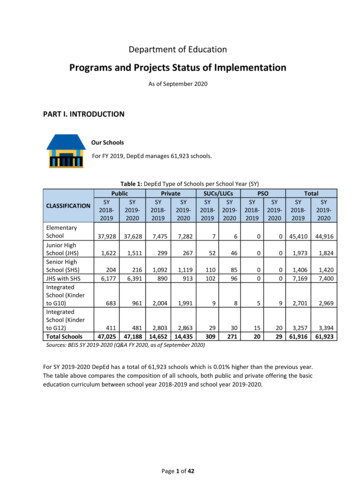
TABLE OF CONTENTS3. Welcome4.Elections5. Benefits At-A-Glance6.Medical Plan Options7.Wellness Program7. Non-Smoking Incentive8.Understanding your HRA9-10.Medical11.Blue Cross Online Visits12. Blue 365 Resources and Discounts12-13.Blue Member Secured Services14. Understanding BCN’s Referral Process15. BCN Woman’s Choice Program16.Durable Medical Equipment and Supplies17-18.BCN Health Care While Traveling19. Dental20.Vision21. Basic Life and AD&D22. Voluntary Life and AD&D23.Short Term Disability24.Long Term Disability25-26. FSA27. Employee Assistance Program28. WillPrep Services29-30. Accident31. Whole Life32.Hospital Indemnity33. Mandatory Notices34-35. Medicare Part D Notice36-38. CHIP Notice39. Resources2
WELCOMEGardner-White Furniture is pleased to offer anexcellent benefit program. These health and welfarebenefits are designed to protect you and yourfamily while you are an active employee. Weencourage you to carefully review this informationand share it with your covered dependents.EligibilityHealth and welfare benefits are available toall full-time regular employees. Medicalcoverage is available for all employees whoqualify based on Federal ACA requirements.Dependent EligibilityYour dependents may also be covered under themedical, dental, vision and optional life benefits.Eligible dependents include: Your legal spouse. Medical:Your children to the end of the calendar yearthey attain the age 26 regardless of theirmarital, student, or financial status. Dental and Vision:Your children to the end of the calendar yearthey attain the age 26 regardless of theirmarital, student, or financial status. Optional Life:Your children to the end of the calendar yearthey attain the age 26 regardless of theirmarital, student, or financial status.Medicare Part D PrescriptionDrug InformationIf you are enrolled in or will be eligiblefor Medicare in the next 12 months,Federal law gives you more choices forprescription drug coverage. See pages34-35 for more information.New Hire Waiting PeriodAs a condition of eligibility for benefits, employees mustcomplete a one-month bona fide employment-basedorientation period.Eligible employees may enroll for benefits on the firstof the month following 60 days after they completethe orientation period. If elected, coverage will beeffective on that date if you completed the necessaryonline enrollment. As a new employee you have up to30 days after your eligibility date to make your benefitselections. If you do not enroll within the first 30 daysof your eligibility date, you will not be eligible forcoverage until the next open enrollment period.Terminating CoverageIf you leave Gardner White for any reason all benefitcoverages will end on your last date of employment.3
ELECTIONSKnowing that every employee has different needs, Gardner-White Furniture’s Employee Benefit Program isspecifically designed to provide basic benefits and allow you the flexibility to elect those levels of coverage youchoose for you and your family.ElectionsIt is important that you make your choices carefully. Changes to those elections can generally only be madeduring the annual open enrollment period. Exceptions will be made for certain changes in status during the year,allowing you to make a mid-year benefit change consistent with the change in status. If you have a change instatus, you must change your benefit elections within 30 days of the qualifying event, or you will need to waituntil the next annual open enrollment period. A change in status includes: Change in legal marital status (marriage, death of spouse, divorce or legal separation) Change in the number of dependents (birth, death, adoption or placement for adoption) Change in the employment status of the employee or the employee’s spouse including begin or terminateemployment, change in eligibility (full time to part time), a strike or lockout, commencement or return froman unpaid leave of absence and a change in worksite Dependent satisfies or ceases to satisfy eligibility requirements (attains a particular age) Alternate open enrollment time frame for spouse or loss of other coverageWhat happens if I do not enroll?If you do not enroll within the required time period, you will not beeligible for benefits until the next annual open enrollment period oryou experience a change in status. You may be subject to waitingperiods or reduced benefits if you decide to enroll at a later date.Will my election choices continue if I do not make changes duringOpen Enrollment?No, you must actively call the enrollment center to make your 2019elections.COBRA Continuation CoverageWhen you or any of your dependents no longer meet theeligibility requirements for your employer’s health and welfareplans, you may be eligible for continued coverage as required bythe Consolidated Omnibus Budget Reconciliation Act of 1986(COBRA). In the event of divorce, legal separation or change independent status, it is your responsibility to notify humanresources within 60 days for complete COBRA detail requirements.Your Tax AdvantageYour contributions for medical, dental, vision and FSA benefits aremade on a pre-tax basis. Your taxable income will be reducedby the amount you contribute for each benefit. You will not payincome tax on the amount you contribute, thus saving you taxdollars. The fact that your taxable income will be lowered doesnot affect your salary-related benefits, which will continue to becalculated upon your base earnings before contributions. You may,however, realize slightly lower Social Security benefits in the futurebecause of this pre-tax feature.4
BENEFITS AT-A-GLANCEWe take pride in offering a benefits program which provides flexibility for the diverse and changing needs of ouremployees. The following is an overview of the benefits provided to eligible employees and their dependents.Benefit PlanMedical/Rx InsuranceBlue Cross Blue Shield of Michigan (BCBSM)Blue Care Network (BCN)Dental InsuranceGuardian Life Insurance CompanyVoluntary Vision InsuranceGuardian Life Insurance CompanyBasic Life / AD&D InsuranceGuardian Life Insurance CompanyVoluntary Term Life InsuranceGuardian Life Insurance CompanyVoluntary Dependent Term Life InsuranceGuardian Life Insurance CompanyVoluntary Short Term DisabilityGuardian Life Insurance CompanyVoluntary Long Term DisabilityGuardian Life Insurance CompanyOptionsEmployer/Employee Paid - 3 Plans Offered BCN HMO: Core Option with HRA ( 1,500 Deductible) BCN HMO: Buy-Down Option ( 4,000 Deductible) BCBS PPO: Buy-up Option ( 500 Deductible)Employer/Employee Paid - 2 Plans Offered First Commonwealth DHMO Guardian PPOVoluntary Benefit - 100% Employee Paid Davis Vision PPOEmployer Paid 25,000 BenefitVoluntary Benefit - 100% Employee Paid Coverage up to 500,000 (increments of 10,000) Evidence of insurability required for late entrantsVoluntary Benefit - 100% Employee Paid Spouse: Coverage up to 10,000 Child(ren): Coverage up to 5,000 Evidence of insurability required for late entrants100% Employer Paid 60% of weekly earnings Maximum weekly benefit of 2,000Voluntary Benefit - 100% Employee Paid 60% of monthly earnings Maximum monthly benefit of 5,000Health Care Flexible Spending AccountTASC Up to 2,000 tax-free for eligible health care expensesDependent Care Flexible Spending AccountTASC Up to 5,000 tax-free for eligible day care expensesEmployee Assistance Program (EAP)Guardian / WorkLifeMattersVoluntary Accident InsuranceUNUMVoluntary Whole Life InsuranceUNUMVoluntary Hospital Indemnity InsuranceUNUM 24/7 services to support you and your family Up to 3 FREE sessionsVoluntary Benefit - 100% Employee Paid Pays a set benefit amount based on the type of injury Wellness BenefitVoluntary Benefit - 100% Employee Paid Earns cash valueVoluntary Benefit - 100% Employee Paid Pays a set benefit amount Wellness BenefitThis guide highlights the main benefits available. For a more complete description, please see the PlanDocuments. If any conflict should arise between this guide and the Plan Documents, the Plan Documentswill govern.5
MEDICAL PLAN OPTIONSGardner-White Furniture offers three medical options with different benefit levels so that you may select theoption that best meets the needs of you and your family. BCN HMO Core Option with HRA ( 1,500 Deductible) BCN HMO Buy-Down Option ( 4,000 Deductible) BCBS PPO Option ( 500 Deductible)HMO Specifics (Only available to Michigan residents) An HMO utilizes a network of participating doctors and hospitals. Coverage is limited to use of in-network providers except in the case of an emergency. You must pick a primary care physician (PCP) and this doctor coordinates all of your health care services. Females using this option may select a PCP as well as an OB/GYN and are not required to obtain referrals forroutine OB/GYN services. If you need to see a specialist, your PCP must give you a referral to a specialist within the network. If yousee a specialist without obtaining a referral, you will either have no benefits for that service or have areduced benefit. To find an HMO provider, go to www.bcbsm.com or call the phone number on the back of your ID card.PPO Specifics Benefits are provided through a Preferred Provider Organization (PPO), where a network of hospitals anddoctors are available for your use. If you use the network, you will receive the highest level of benefits offered by the PPO. Although the network is available, you are not required to use it. You always have the complete freedom toselect any provider whenever you need care. However, the out-of-network benefits are lower and yourout-of-pocket costs will be higher. This option does not require any referrals to see a specialist. To find a PPO provider, go to www.bcbsm.com or call the phone number on the back of your ID card.ElectionsYou may elect medical coverage for yourself; you and your spouse; you and child(ren); or for your entire family.ContributionsYou and Gardner-White Furniture share in the cost of coverage. Please see the ADP benefit portal for informationon your contributions.6
WELLNESS PROGRAMGardner-White Furniture is continuing their wellness program incentive for the 2019 plan year.The below will explain the requirements for both the member and any applicable spouse. In order to qualify forthe incentive, both items must be completed. You and your spouse are eligible for two separate rewards.Wellness Requirements Schedule and obtain your annual physical with your Primary Care Physician. Ask him or her to complete the2019 Annual Wellness Incentive Form. The 2019 Annual Wellness Incentive Form can be found on the ADPbenefits portal. Go to www.bcbsm.com and log in as a member and complete your Health Risk Assessment. You and yourspouse will each need separate logins due to HIPAA. Your results are completely confidential.In order to qualify for the incentive, both the 2019 Annual Wellness Incentive Form and the BCN Health RiskAssessment must be completed within 90 days of your new hire benefits eligibility (or by July 1, 2019 foropen enrollment).IncentiveEach employee and their applicable spouse has the opportunity to earn a 100 gift card to Target. The potentialcombined gift card for both employee and spouse is 200. Please keep in mind in order to qualify for the giftcard, you must complete both the Health Assessment as well as have your Primary Care Physician complete the2019 Annual Wellness Incentive Form within the specified time frame.Please note: The gift card is a taxable benefit and must be reported as income at the end of the year under yourW2 earnings.NON-SMOKING INCENTIVEGardner-White Furniture will continue to provide the non-tobacco incentive contribution rates for 2019.Gardner-White offers a wellness incentive in the form of reduced weekly employee contributions if you and yourspouse are both non-tobacco users.Blue Cross Blue Shield and Blue Care Network offer resources to assist you on your tobacco free journey.To qualify as a non-tobacco user, you must be tobacco free for the last 12 months.All non-tobacco members will receive the reduced contributions as of 4/1/2019 (or your initial effective date fornew hires), however, you must confirm and verify that you are a non-tobacco user at the time of your enrollment.If the required documentation is not received within 30 days of your effective date, your payroll deductions willchange to the standard contribution. In addition, if a member ceases to actively participate in a tobaccocessation program throughout the year they will move back to the standard contribution rate.Please be advised that any reporting and information obtained in regards to a member’s participation status willbe used only for the purposes of certifying willingness to comply and will be kept completely confidential.7
BCN HMO with HEALTH REIMBURSEMENT ACCOUNT(HRA) - UNDERSTANDING YOUR HRABlue Care Network (BCN) CORE HMO Plan Includes Health Reimbursement Account (HRA)Although your BCN CORE plan has a deductible of 4,000 Single/ 8,000 Family, Gardner-White Furniture’s HRAplan will contribute up to 2,500 per person or 5,000 per family for services that are applied to the deductible asshown below:What is an HRA?HRA’s are health care accounts funded by your employer to help cover employees’ out-of-pocket costs whenthey receive health care services. Member carry a single medical ID card with a BCN HMO - HRA Designation A continuous care process that is seamless for HRA and medical services Hassle-free coverage with no reimbursement paperwork You receive a single Explanation of Benefits statement that tracks your deductible and coinsuranceobligations and your HRA balances You can view your balances online at www.bcbsm.com through Member Secured Services The plan utilizes the same extensive BCN provider network.BCN HMO Plan DeductibleRequirementYour DeductibleResponsibility 4,000 Single/ 8,000 Family 1,500 Single/ 3,000 FamilyDeductibleBCN HRA Reimburses(Employer Funded Account)Up to 2,500 Single/ 5,000 FamilyAs a reminder, the BCN Buy-Down HMO does not include the HRA aspect and truly does have a 4,000 Single/ 8,000 Family Deductible.8
MEDICALBoth Blue Care Network HMO Plans (Core and Buy-Down) will renew and accumulate the deductible and annualout-of-pocket maximum on a plan year basis. This means that all deductibles and out-of-pocket maximums willrestart as of April 1 each year.BCN HMOHRA 4,000 per member 8,000 per family 1,500 per member 3,000 per family 6,350 per member 12,700 per familyNoneBuy-Down Plan 4,000 per member 8,000 per family 4,000 per member 8,000 per family 6,350 per member 12,700 per familyNone 20 copay 20 copaySpecialist Visit 40 copy after deductible 40 copy after deductiblePreventive Care/Screening/Immunization100% covered;deductible does not apply100% covered;deductible does not apply80% after deductible80% after deductibleImaging (CT/PET Scans, MRIs) 150 copay after deductible 150 copay after deductibleEmergency Room Care 150 copay after deductible 150 copay after deductibleUrgent Care 50 copay 50 copayOnline Visit 20 copay 20 copayTier 1A - Value Generics 6 copay 6 copayTier 1B - Generics 40 copay 40 copayTier 2 - Preferred Brand 60 copay 60 copayTier 3 - Non-Preferred Brand 80 copay 80 copayTier 4 - Preferred Specialty20% coinsurance (max 200)20% coinsurance (max 200)Tier 5 - Non-Preferred Specialty20% coinsurance (max 300)20% coinsurance (max 300)Deductible(4.1.19 - 3.31.20)Member Deductible ResponsibilityAnnual Out-of-Pocket MaximumLifetime Dollar MaximumPrimary Care VisitDiagnostic Test (x-ray, blood work)Prescription Drugs9
MEDICALBlue Cross Blue Shield PPO Plan will renew as of April 1, however the deductible and annual out-of-pocket maximums accumulate on a calendar year basis (January 1 – December 31).BCBS PPO PlanDeductible(1.1.19 - 12.31.19)Annual Coinsurance MaximumAnnual Out-of-Pocket Maximum(includes deductibles, coinsurance and copays)In-Network 500 per member 1,000 per family 1,500 per member 3,000 per family 6,350 per member 12,700 per familyLifetime Dollar MaximumOut-of-Network 1,000 per member 2,000 per family 3,000 per member 6,000 per family 12,700 per member 25,400 per familyNonePrimary Care Visit 20 copay60% coinsuranceSpecialist Visit 20 copay60% coinsurance100% covered;deductible does not applyNot coveredDiagnostic Test (x-ray,blood work)80% coinsurance60% coinsuranceImaging (CT/PET scans, MRIs)80% coinsurance60% coinsuranceEmergency Room Care 150 copay 150 copayUrgent Care 20 copay60% coinsuranceOnline Visit 20 copay 20 copayPreventive Care/Screening/ImmunizationPrescription DrugsGeneric 15 copay for 30-day supply; 30 copay for 90-day supplyPreferred Brand-Name Drugs 30 copay for 30-day supply; 60 copay for 90-day supply;Non Preferred Brand-Name Drugs 60 copay for 30-day supply; 120 copay for 90-day supply10In-Network copay plus anadditional 25% of the approvedamountIn-Network copay plus anadditional 25% of the approvedamountIn-Network copay plus anadditional 25% of the approvedamount
BLUE CROSS ONLINE VISITSWhen you use Blue Cross Online VisitsSM (previously called 24/7 online health care), you will have access to onlinemedical and behavioral health services anywhere in the US.You can rest assured knowing you and your covered family members can see and talk to: A doctor for minor illnesses such as a cold, flu or sore throat when your primary care doctor is notavailable. A behavioral health clinician or psychiatrist to help work through different challenges such as anxiety,depression and grief. (Behavioral health visits are available by appointment only.)While online health care should not replace your relationship with your primary care physician, it can beinvaluable when: Your doctor isn’t available You can not leave home or your workplace. You are on vacation or traveling for work. You are looking for affordable after-hours care.How do I get started?Start by doing one of the following: Mobile - Download the BCBSM Online Visits app Web - Visit bcbsmonlinevisits.com Phone - Call 844-606-1608If you are new to online visits, you will need to register with your Blue Cross or Blue Care Network healthplan information.Share information with your primary care physicianTo ensure that your primary care physician knows about all of yourmedical care, let them know when you use online health care. At theend of your visit, check the box to share your visit summary report withyour family doctor or other health care providers.How much does it cost?For medical services, an online visit is based on your office visitcost share. Costs for behavioral health services vary dependingon the type of provider and service received. You will be chargedusing your existing outpatient behavioral health benefits.Questions?For questions regarding online health care, contact:844-606-1608bcbsmonlinevisits.com11
BLUE 365 RESOURCES AND DISCOUNTSwww.blue365deals.comDiet/Weight ControlWhen you are managing your weight and aiming for better nutrition, you deserve all the support you can get.FitnessNo pain, no gain? Not necessarily so, but there is no getting around the health-filled benefits of breaking a sweat.Find a fitness plan that fits you.Diet/Weight ResourcesThe quickest way to a healthier diet is through the brain. These resources make understanding how to eat right asnap.Stress ManagementStress creates “wear and tear” on the body. Find more information on how to manage stress effectively to stayhealthy.Quality CareTo improve your peace of mind, Blue365 is here to help you find quality care when you need it most.Complementary and Alternative MedicineFor a more well-founded and holistic approach to your healthcare, explore avenues of alternative medicine.BLUE MEMBER SECURED SERVICESBlueCard ProgramWhen you are a Blue member, you take your healthcare benefits with you - across the country and around theworld. The BlueCard Program gives you access to doctors and hospitals almost everywhere, giving you the peaceof mind that you will be able to find the healthcare provider you need. Within the United States, you are coveredwhether you need care in urban or rural areas. Outside of the United States, you have access to doctors andhospitals in nearly 200 countries and territories around the world through the BlueCard Worldwide Program.When you need healthcare outside the US, Puerto Rico and US Virgin Islands1. Always carry your Blue Cross and Blue Shield ID card.2. Contact your Blue Plan before leaving as your health care benefits may be different outside the US, PuertoRico and US Virgin Islands.3. In an emergency, go directly to the nearest hospital or doctor. Call the BlueCard Worldwide Service Centerif hospitalized.4. If you need to located a doctor or hospital, or need medical assistance services, call the BlueCardWorldwide Service Center at 800-810-BLUE (2583) or call collect at 804-673-1177, 24/7. An assistancecoordinator, in conjunction with a medical professional, will arrange a physician appointment orhospitalization, if necessary.5. Call the BlueCard Worldwide Service Center at 800-810-2583 when you need inpatient care. In most cases,you should not need to pay upfront for inpatient care at BlueCard Worldwide hospitals except for theout-of-pocket expenses (noncovered services, deductible, copayment and coinsurance) you normally pay.When cashless access is arranged, the hospital will submit your claim on your behalf.6. Call your Blue Plan for percetification or prior authorization, if necessary. Refer to the phone number onthe back of your ID card.12
BLUE MEMBER SECURED SERVICESYou and your family members can manage your health and health plan online at bcbsm.com.Register for Member Secured Services to access all of our online services.Registering is easy. Here’s how: Visit bcbsm.com Click on the I am a Member tab Click on Register Follow the registration steps that appear on the screenIf you are registering for the first time, you will be asked a few brief questions to verify your identity. This securitystep is required because Member Secured Services offers you personalized online services that containprotected health information. We are committed to protecting your privacy.If you are the Blues subscriber on the account, you will alsobe given the opportunity to “go green” and receive yourExplanation of Benefit Payments statements electronically.Once you register you will be able to: Review you Explanation of Benefit Paymentsstatements online. We’ll send you an email wheneach statement becomes available. In addition toviewing the statements online, you can also savethem as a PDF. View detailed claim and benefit information. Access your pharmacy information. Take an interactive health assessment and receive alifestyle score and tailored action plan. Participate in online health coaching programs soyou can achieve health goals identified by yourhealth assessment. Access extensive, up-to-date health content,including multimedia components like podcasts andvideos. Find and compare doctors and hospitals based onfactors most important to you, like cost and quality. Save money on the healthy products and servicesyou use everyday through our member savingsprograms, Health Blue XtrasSM and Blue365 .All features may not be available, depending on your plan.Questions?For Web registration or access help, call 888-417-3479.For benefit, eligibility or claims information, call theCustomer Service number on the back of your BluesIDcard.13
UNDERSTANDING BLUE CARENETWORK’S REFERRAL PROCESSYour doctor is your health partnerYour primary care physician, or PCP, is responsible for the care you receive, from preventive health services totreatment for illness. As your health care partner, your PCP makes sure that you get the care you need when youneed it.Getting carePCPs provide many services in their offices, and they arrange for specialist care or special tests. Your networkgynecologist or obstetrician can also refer you to specialists for OB/GYN-related services. Specialists decide onthe services and the number of visits required for treatment.Extensive network of specialistsOur network includes thousands of specialists. More than likely, your PCP or OB-GYN will refer you to someonehe or she knows professionally. Sometimes the specialist may even be part of the same group as your PCP.When you do not need a referralYou do not need a referral for behavioral health services, but you must be seen by a provider who is in yourplan’s network. Also, female members do not need a referral to see a gynecologist or obstetrician in your plan’snetwork for annual well woman visits and obstetrical care (Woman’s Choice program). Your OB-GYN can alsorefer you for specialist care, but only for OB-GYN-related services.Chiropractic servicesBCN and BCN Advantage members must have a referral from their PCPs for chiropractic services. Thechiropractor must also get BCN approval before providing manipulations or other physical medicine services forBCN members.Referrals for specialist careYour PCP manages your health care through a referral process with these guidelines: Your PCP refers you to a specialist. Check that the specialist is in your plan’s network. Also ask if there’sanything else you need to do to ensure coverage. You may need special approval from BCN for certain services. You need approval from BCN for all servicesfrom specialists who are not in your plan’s network. Only your PCP or OB-GYN can refer you for specialist care. If the service requires a referral and your PCP or OB-GYN does not refer you, you are responsible for thecharges. Changing your PCP while a specialist is treating you may change your treatment authorization. Check withyour new PCP.Questions?If you have questions about the referral process, please call the Customer Service number on the back of yourmember ID card. The TTY number is 711.14
BLUE CARE NETWORK’S WOMAN’SCHOICE PROGRAMYou choose. No referral needed.Woman’s Choice is a self-referral program. This means for routine women’s health services, you may visit certainBlue Care Network-contracted specialists without a referral from your primary care physician.Find a Woman’s Choice doctor at bcbsm.com/find-a-doctor.Women’s health servicesWoman’s Choice health specialists include obstetrician-gynecologists, gynecologic oncologists, reproductiveendocrinologist
the incentive, both items must be completed. You and your spouse are eligible for two separate rewards. Wellness Requirements Schedule and obtain your annual physical with your Primary Care Physician. Ask him or her to complete the 2019 Annual Wellness Incentive Form. The 2019 Annual Wellness Incentive Form can be found on the ADP benefits .