Transcription
PEBP PPO DENTAL PLAN AND SUMMARY OF BENEFITSFOR LIFE INSURANCEMASTER PLAN DOCUMENTPLAN YEAR 2023(EFFECTIVE JULY 1, 2021 – June 30, 2022)Public Employees’ Benefits Program901 S. Stewart Street, Suite 1001Carson City, Nevada 89701
Table of ContentsTable of ContentsAmendment Log . iiiWelcome PEBP Participant . 1Introduction . 2Suggestions for Using this Document . 3Accessing Other Benefit Information: . 3Participant Rights and Responsibilities. 4You have the right to: . 4You have the responsibility to: . 4The plan is committed to: . 5Summary of PPO Dental Benefits . 6Eligible Dental Expenses . 6Non-Eligible Dental Expenses . 6Out-of-Country Dental Purchases . 6Deductibles . 7Coinsurance . 7Plan Year Maximum Dental Benefits. 7Payment of Dental Benefits . 8Extension of Dental Coverage . 8Dental Pretreatment Estimates. 8Prescription Drugs Needed for Dental Purposes . 9Voluntary PPO Dental Plan Option for Medicare Retirees Enrolled through VIA Benefits . 9Dental Network . 10In-Network Services . 10Out-of-Network Services . 10When Out-of-Network Providers May be Paid as In-Network Providers? . 11Schedule of Dental Benefits . 12Preventive Services . 12Basic Services. 13Public Employees’ Benefits Program2023PPO Dental Plan & Life Insurance Plan Yeari
Table of ContentsMajor Services . 14Benefit Limitations and Exclusions: PPO Dental Plan . 16Self-Funded PPO Dental Claims Administration . 20How Dental Benefits are Paid. 20How to File a Dental Claim . 20Where to Send the Claim Form . 22Dental Appeal Process . 23Written Notice of Denial of Claim . 23Level 1 Appeal . 23Level 2 Appeal . 23Coordination of Benefits (COB) . 26When and How Coordination of Benefits (COB) Applies . 26Which plan Pays First: Order of Benefit Determination Rules . 27The Overriding Rules . 27Administration of COB . 29Coordination with Medicare . 31Coordination with Other Government Programs . 31Third Party Liability . 33Subrogation and Rights of Recovery . 33Basic Life Insurance . 35Eligibility for Life Insurance . 35Coverage . 35Participant Contact Guide . 36Key Terms and Definitions . 39Public Employees’ Benefits ProgramPPO Dental Plan & Life Insurance Plan Year 2023ii
Amendment LogAmendment LogAny amendments, changes or updates to this document will be listed here. The amendment logwill include what sections are amended and where the changes can be found.Public Employees’ Benefits ProgramPPO Dental Plan & Life Insurance Plan Year 2023iii
WelcomeWelcome PEBP ParticipantWelcome to the State of Nevada Public Employees’ Benefits Program (PEBP). PEBP provides avariety of benefits such as medical, dental, life insurance, flexible spending accounts, and othervoluntary insurance benefits for eligible state and local government employees, retirees, andtheir eligible dependents.As a PEBP participant, you may enroll in whichever benefit plan offered in your geographical areathat best meets your needs, subject to specific eligibility and Plan requirements. These plansinclude the Consumer Driven Health Plan (CDHP) with a Health Savings Account (HSA) or a HealthReimbursement Arrangement (HRA), Premier (EPO) Plan, Low Deductible PPO Plan, and HealthPlan of Nevada HMO Plan. (In general, Medicare retirees are required to enroll in a medical planthrough PEBP’s Medicare Exchange vendor). You are also encouraged to research plan provideraccess and quality of care in your service area.This document describes PEBP’s PPO Dental Plan, and Life Insurance Benefits. Active employeesenrolled in a PEBP-sponsored medical plan (CDHP, Premier Plan. Low Deductible PPO Plan, orHealth Plan of Nevada HMO Plan) receive dental and basic life. Retirees enrolled in a PEBPsponsored medical plan receive dental coverage and if eligible, basic life insurance coverage.Eligible retirees enrolled in a medical plan through PEBP’s Medicare Exchange receive basic lifeinsurance and the choice to enroll in PEBP’s voluntary PPO Dental Plan option.PEBP participants should examine this document to become familiar with the PPO Dental Planand basic life insurance benefits. In addition to examining this document, participants areencouraged to read the Master Plan Documents or Evidence of Coverage Certificates (EOCs),Summary Plan Descriptions, and Summary of Benefits and Coverage applicable to their medicalplan. Participants should also examine the PEBP Enrollment and Eligibility, PEBP Active EmployeeHealth and Welfare Wrap Plan Document, PEBP Retiree Health and Welfare Wrap PlanDocument, Section 125, Medicare Exchange HRA Summary Plan Description, and other planmaterials relevant to their benefits. These documents and other materials are available atwww.pebp.state.nv.us or to request a particular document by mail, contact PEBP at 775-6847000 or 800-326-5496 or email member services by selecting the contact us feature in your EPEBP portal member account.In addition, helpful material is available from PEBP or any PEBP vendor listed in the ParticipantContact Guide.PEBP encourages you to stay informed of the most up to date information regarding your healthcare benefits. It is your responsibility to know and follow the plan provisions and otherrequirements described in PEBP’s Master Plan Document and related materials.Sincerely,Public Employees’ Benefits ProgramPublic Employees’ Benefits ProgramPPO Dental Plan & Life Insurance Plan Year 20231
IntroductionIntroductionThis Master Plan Document describes the PEBP self-funded PPO Dental Plan benefits offered toeligible employees, retirees, and their covered dependents. Additional benefits for life insuranceare summarized in this document.This PEBP plan is governed by the State of Nevada.This document is intended to comply with the Nevada Revised Statutes (NRS) Chapter 287, andthe Nevada Administrative Code 287 as amended and certain provisions of NRS 695G and NRS689B.The Plan described in this document is effective July 1, 2021, and unless stated differently,replaces all other self-funded Dental Benefit Plan documents and summary plan descriptionspreviously provided to you.This document will help you understand and use the benefits provided by the Public Employees’Benefits Program (PEBP). You should review it and show it to members of your family who are orwill be covered by the Plan. It will give you an understanding of the coverage provided, theprocedures to follow in submitting claims, and your responsibilities to provide necessaryinformation to the Plan. Be sure to read the Exclusions, and Key Terms and Definitions Sections.Remember, not every expense you incur for health care is covered by the Plan.All provisions of this document contain important information. If you have any questions aboutyour coverage or your obligations under the terms of the Plan, please contact PEBP at the numberlisted in the Participant Contact Guide. The Participant Contact Guide provides you with contactinformation for the various components of the Public Employees’ Benefits Program.PEBP intends to maintain this Plan indefinitely, but reserves the right to terminate, suspend,discontinue, or amend the Plan at any time and for any reason. As the Plan is amended from timeto time, you will be sent information explaining the changes. If those later notices describe abenefit or procedure that is different from what is described here, you should rely on the laterinformation. Be sure to keep this document, along with notices of any Plan changes, in a safe andconvenient place where you and your family can find and refer to them.The benefits offered with the Consumer Driven Health Plan, Premier Plan, Low Deductible PPOPlan, and Health Plan of Nevada include prescription drug benefits, dental coverage, and basiclife insurance as applicable. The medical and prescription drug benefits are described inseparately in the applicable plan’s Master Plan Document or Evidence of Coverage certificate. Anindependent third-party claims administrator pays the claims for the PPO Dental Plan.Per NRS 287.0485 no officer, employee, or retiree of the State has any inherent right to benefitsprovided under the PEBP.Public Employees’ Benefits ProgramPPO Dental Plan & Life Insurance Plan Year 20232
IntroductionSuggestions for Using this DocumentThis document provides important information about your benefits. We encourage you to payattention to the following: The Table of Contents provides you with an outline of the sections.The Participant Contact Guide to become familiar with PEBP vendors and the servicesthey provide.The Participant Rights and Responsibilities section located in the Introduction of thisdocument.The Key Terms and Definitions section explains many technical, medical, and legal termsthat appear in the text.The Eligible Dental Expenses, Schedule of Dental Benefits and Exclusions sections describeyour benefits in more detail.How to File a Dental Claim section to find out what you must do to file a claim.The Appeals Procedures section to find out how to request a review (appeal) if you aredissatisfied with a claims decision.The section on Coordination of Benefits discusses situations where you have coverageunder more than one health care plan including Medicare. This section also provides youwith information regarding how the plan subrogates with a third party who wrongfullycaused an injury or illness to you.Accessing Other Benefit Information:Refer to the following plan documents for information related to dental, life, flexible spendingaccounts, enrollment and eligibility, COBRA, third-party liability and subrogation, HIPAA Privacyand Security and mandatory notices. These documents are available at www.pebp.state.nv.us. State of Nevada PEBP Active Employee Health and Welfare Wrap Plan; Retiree Health andWelfare Wrap PlanConsumer Driven Health Plan (CDHP) Master Plan Document (MPD); CDHP Summary ofBenefits and Coverage for Individual and FamilyLow Deductible PPO Plan (LD PPO Plan) MPD; LD PPO Plan Summary of Benefits andCoverage (SBC) for Individual and FamilyPEBP PPO Dental Plan and Summary of Benefits for Basic Life Insurance MPDPremier Plan Master Plan Document; SBC for Individual and FamilyHealth Plan of Nevada Evidence of Coverage of Benefits; Summary of Benefits andCoverage for Individual and FamilyPEBP Enrollment and Eligibility MPDFlexible Spending Accounts (FSA) Summary Plan DescriptionSection 125 Health and Welfare Benefits Plan DocumentMedicare Retiree Health Reimbursement Arrangement Summary Plan DescriptionPublic Employees’ Benefits ProgramPPO Dental Plan & Life Insurance Plan Year 20233
Patient Rights and ResponsibilitiesParticipant Rights and ResponsibilitiesYou have the right to: Participate with your health care professionals and providers in making decisions aboutyour health care.Receive the benefits for which you have coverage.Be treated with respect and dignity.Privacy of your personal health information, consistent with State and Federal laws, andthe Plan’s policies.Receive information about the Plan’s organization and services, the Plan’s network ofhealth care professionals and providers and your rights and responsibilities.Candidly discuss with your physicians and providers appropriate or medically necessarycare for your condition, regardless of cost or benefit coverage.Make recommendations regarding the organization’s participants’ rights andresponsibilities policies.Express respectfully and professionally, any concerns you may have about PEBP or anybenefit or coverage decisions the Plan (or the Plan Administrator or its designee) makes.Refuse treatment for any conditions, illness, or disease without jeopardizing futuretreatment and be informed by your physician(s) of the medical consequences.You have the responsibility to: Establish a patient relationship with a participating primary care physician and aparticipating dental care provider.Take personal responsibility for your overall health by adhering to healthy lifestylechoices. Understand that you are solely responsible for the consequences of unhealthylifestyle choices.If you use tobacco products, seek advice regarding how to quit.Maintain a healthy weight through diet and exercise.Take medications as prescribed by your health care provider.Talk to your health care provider about preventive medical care.Understand the wellness/preventive benefits offered by the plan.Visit your health care provider(s) as recommended.Choose in-network participating provider(s) to provide your medical care.Treat all health care professionals and staff with courtesy and respect.Keep scheduled appointments with your health care providers.Read all materials concerning your health benefits or ask for assistance if you need it.Supply information that PEBP and/or your health care professionals need to provide care.Follow your physicians’ recommended treatment plan and ask questions if you do notfully understand your treatment plan and what is expected of you.Follow all the plan’s guidelines, provisions, policies, and procedures.Public Employees’ Benefits ProgramPPO Dental Plan & Life Insurance Plan Year 20234
Patient Rights and ResponsibilitiesInform PEBP if you experience any life changes such as a name change, change of addressor changes to your coverage status because of marriage, divorce, domestic partnership,birth of a child(ren) or adoption of a child(ren). Provide PEBP with accurate and complete information needed to administer your healthbenefit plan, including if you or a covered dependent has other health benefit coverage. Retain copies of the documents provided to you from PEBP and PEBP’s vendors. Thesedocuments include but are not limited to: Copies of the Explanation of Benefits (EOB) from PEBP’s third party claims administrator.Duplicates of your EOB’s may not be available to you. It is important that you store thesedocuments with your other important paperwork. Copies of your enrollment forms submitted to PEBP. Copies of your medical, vision and dental bills. Copies of your HSA contributions, distributions, and tax forms. The plan is committed to: Recognizing and respecting you as a participant.Encouraging open discussion between you and your health care professionals andproviders.Providing information to help you become an informed health care consumer.Providing access to health benefits and the plan’s network (participating) providers.Sharing the plan’s expectations of you as a participant.Public Employees’ Benefits ProgramPPO Dental Plan & Life Insurance Plan Year 20235
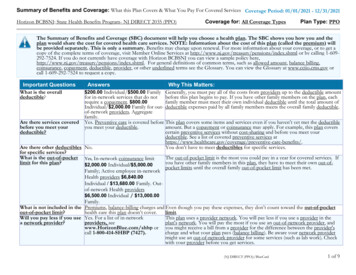
Summary of PPO Dental BenefitsSummary of PPO Dental BenefitsEligible Dental ExpensesYou are covered for expenses you incur for most, but not all, dental services and supplies providedby a dental care provider as defined in the Key Terms and Definitions section of this document thatare determined by PEBP or its designee to be “medically necessary,” but only to the extent that: PEBP or its designee determines that the services are the most cost-effective onesthat meet acceptable standards of dental practice and would produce a satisfactoryresult; andThe charges for them are “usual and customary (U&C)” (see Usual and Customaryin the Key Terms and Definitions section).Non-Eligible Dental ExpensesThe plan will not reimburse you for any expenses that are not eligible dental expenses. That meansyou must pay the full cost for all expenses that are not covered by the Plan, as well as any chargesfor eligible dental expenses that exceeds this Plan’s Usual and Customary determination.Out-of-Country Dental PurchasesThe PPO Dental Plan provides you with coverage worldwide. Whether you reside in the UnitedStates and you travel to a foreign country, or you reside outside of the United States, permanentlyor on a part-time basis and require dental care services, you may be eligible for reimbursement ofthe cost.Typically, foreign countries do not accept payment directly from PEBP. You may be required topay for dental care services and submit your receipts to PEBP’s third party administrator forreimbursement. Dental services received outside of the United States are subject to Planprovisions, limitations and exclusions, clinical review if necessary and determination of medicalnecessity. The review may include regulations determined by the FDA.Prior to submitting receipts from a foreign country to PEBP’s third party administrator, you mustcomplete the following. (PEBP and this Plan’s third-party administrator reserve the right to requestadditional information if needed): Proof of payment from you to the provider of service (typically your credit cardinvoice).Itemized bill to include complete description of the services rendered.Itemized bill must be translated to English.Any costs associated with the reimbursement request must be converted to UnitedStates dollars; andAny foreign purchases of dental care and services will be subject to Plan limitations such as: Benefits and coverage under the PlanDeductiblesCoinsurancePublic Employees’ Benefits ProgramPPO Dental Plan & Life Insurance Plan Year 20236
Summary of PPO Dental Benefits Frequency maximumsAnnual benefit maximumsMedical necessityFDA approvalUsual and Customary (U & C)Once payment is made to you or to the out of country provider, PEBP and its vendors are releasedfrom any further liability for the out of country claim. PEBP has the exclusive authority todetermine the eligibility of all dental services rendered by an out of country provider. PEBP mayor may not authorize payment to you or to the out of country provider if all requirements of thisprovision are not satisfied.Note: Please contact this Plan’s third-party administrator before traveling or moving to anothercountry to discuss any criteria that may apply to a dental service reimbursement request.DeductiblesEach Plan Year, you must satisfy the Plan Year Deductible before the Plan will pay benefits forBasic or Major dental services. Eligible dental expenses for preventive services are not subject tothe Plan Year Deductible or the annual maximum benefit. Benefits for some services are availablefour times each Plan Year, for example preventive cleanings and periodontal maintenancecleanings. Oral examinations and bitewing x-rays are available twice per Plan Year. If a personcovered under this Plan changes status from an employee or retiree to a dependent, or from adependent to an employee and the person is continuously covered under this Plan before, duringand after the change in status, credit will be given for portions of the Deductible already met, andaccumulation of benefit maximums will continue without interruption.There are two types of Deductibles: Individual and Family. The Individual Deductible is themaximum amount one covered person must pay each Plan Year before plan benefits are availablefor Basic or Major dental services. The Plan’s Individual Deductible is 100. The FamilyDeductible is the maximum amount a family of three or more is required to pay in a Plan year.The plan’s family Deductible is 300. The Family Deductible is accumulative meaning that onemember of the family cannot satisfy the entire Family Deductible. Both in- and out-of-networkservices are combined to meet your Plan Year Deductible.CoinsuranceThere is no Coinsurance amount for preventive services unless services are rendered by a nonPPO dental provider. For Basic or Major dental services, once you have met your Plan YearDeductible, the Plan pays its percentage of the eligible Usual and Customary dental expenses, andyou are responsible for paying the rest (the applicable percentage paid by the Plan is shown in theSchedule of Dental Benefits). The part you pay is called the Coinsurance. Note: Your out-ofpocket expenses will be less if you use the services of a dental care provider who is part of thePreferred Provider Organization (PPO), also called in-network.Plan Year Maximum Dental BenefitsThe Plan Year maximum dental benefits payable for any individual covered under this Plan is 1,500. The Plan Year maximum dental benefit is combined to include both in-network and outPublic Employees’ Benefits ProgramPPO Dental Plan & Life Insurance Plan Year 20237
Summary of PPO Dental Benefitsof-network services. Under no circumstances will the combination of in-network and out-ofnetwork benefit payments exceed the 1,500 Plan Year maximum benefit. This maximum doesnot include your Deductible or any amounts over Usual and Customary. Benefits paid for eligiblepreventive dental services do not apply to the annual maximum dental benefit.Payment of Dental BenefitsWhen charges for dental services and supplies are incurred, services and supplies are consideredto have been incurred on the date the services are performed or on the date the supplies arefurnished. However, this rule does not apply to the following services because they must beperformed over a period of time. Fixed partial dentures, bridgework, crowns, inlays and onlays: All services relatedto installation of fixed partial dentures, bridgework, crowns, inlays and onlays areconsidered to have been incurred on the date the tooth (or teeth) is (or are) preparedfor the installation.Removable partial or complete dentures: All services related to the preparation ofremovable partial or complete dentures are considered to have been incurred on thedate the impression for the dentures is taken.Root canal treatment (endodontics): All services related to root canal treatment areconsidered incurred on the date the tooth is opened for the treatment.Extension of Dental CoverageIf dental coverage ends for any reason, the Plan will pay benefits for you or your covereddependents through the last day of the month in which the coverage ends. The Plan will also paybenefits for a limited time beyond that date for the following: A prosthesis (such as a full or partial denture) if the dentist took the impressionsand prepared the abutment teeth while you or your dependents were covered andinstalls the device within 31 days after coverage ends.A crown, if the dentist prepared the crown while you or your dependent(s) werecovered and installs it within 31 days after coverage ends.Root canal treatment, if the dentist opened the tooth while you or your dependent(s)were covered and completes the treatment within 31 days after coverage ends.Dental Pretreatment EstimatesWhenever you expect that your dental expenses for a course of treatment will be more than 300,you are encouraged to obtain a pretreatment estimate from the third-party claims administrator.This procedure lets you know how much you will have to pay before you begin treatment.To obtain a pretreatment estimate, you and your dentist should complete the regular dental claimform (available from and to be sent to the third-party claims administrator, whose name andaddress are listed on the Participant Contact Guide in this document), indicating the type of workto be performed also referred to as a treatment plan, along with supporting x-rays and the estimatedcost (valid for a 60-day period following the submission of the pretreatment estimate request).Once it is received, the third-party claims administrator will review the treatment plan and thensend your dentist a statement within the next 60 days showing what the Plan may pay. Your dentistPublic Employees’ Benefits ProgramPPO Dental Plan & Life Insurance Plan Year 20238
Summary of PPO Dental Benefitsmay call the third-party claims administrator for a prompt determination of the benefits payablefor a dental procedure.Prescription Drugs Needed for Dental PurposesNecessary prescription drugs needed for a dental purpose, such as antibiotics or pain medications,should be obtained using the prescription drug benefit provided under your medical plan.NOTE: Some medications for a dental purpose are not payable, such as fluoride or periodontalmouthwash. See the Medical Exclusions section under Drugs for more information.Voluntary PPO Dental Plan Option for Medicare Retirees Enrolled through VIA BenefitsMedicare retirees enrolled in a medical plan through VIA Benefits (Medicare Exchange) and thoseretirees with Tricare for Life and Medicare Parts A and B who are eligible for a Medicare ExchangeHealth Reimbursement Arrangement (HRA) have the option to enroll in PEBP’s PPO Dental Plan.Enrollment in PEBP’s PPO Dental Plan requires automatic dental premium reimbursement fromthe retiree’s Health Reimbursement Arrangement (HRA). The dental premium will only bereimbursed up to the amount in retiree’s HRA. When the amount of the dental premium is morethan the unused amount in the retiree’s HRA, the amount of the premium will be carried forwardin the retiree’s HRA until the unused amount in the HRA is sufficient to reimburse for the dentalpremium.Public Employees’ Benefits ProgramPPO Dental Plan & Life Insurance Plan Year 20239
Dental NetworkDental NetworkIn-Network ServicesIn-network dental care providers have agreements with the Plan under which they
Plan, and Health Plan of Nevada include prescription drug benefits, dental coverage, and basic life insurance as applicable. he medical and prescription drug bT enefits are described in separately in the applicable plan's Master Plan Document or Evidence of Coverage certificate.